Cirrhosis other imaging findings: Difference between revisions
No edit summary |
|||
| (31 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Cirrhosis}} | {{Cirrhosis}} | ||
{{CMG}} {{AE}} {{ADI}} {{Cherry}} | |||
==Overview== | ==Overview== | ||
[[Tc-99m]] labeled sulfur may be used in nuclear imaging to provide some indication of [[Liver|hepatic]] function in cirrhotic patients. In candidates for [[liver transplant]], [[CTA]] is used to asses the drainage of the [[liver]]. All patients with cirrhosis must undergo a diagnostic [[endoscopy]] for the evaluation of [[varices]]. [[Stomach|Gastric]] [[endoscopy]] is an option if [[gastric varices]] are suspected, and [[endoscopic ultrasound]] may also help in the visualization of [[varices]]. [[ERCP]] is performed if a [[Bile duct|biliary]] pathology such as [[primary sclerosing cholangitis]] is suspected as the underlying cause of cirrhosis. | |||
==Other Imaging Findings== | |||
===Nuclear Imaging=== | |||
*[[Radionuclide]] testing may be useful in the diagnosis of cirrhosis:<ref name="pmid26494949">{{cite journal |vauthors=Nishikawa H, Osaki Y |title=Liver Cirrhosis: Evaluation, Nutritional Status, and Prognosis |journal=Mediators Inflamm. |volume=2015 |issue= |pages=872152 |year=2015 |pmid=26494949 |pmc=4606163 |doi=10.1155/2015/872152 |url=}}</ref><ref name="pmid3995244">{{cite journal |vauthors=McLaren MI, Fleming JS, Walmsley BH, Ackery DM, Taylor I, Karran SJ |title=Dynamic liver scanning in cirrhosis |journal=Br J Surg |volume=72 |issue=5 |pages=394–6 |year=1985 |pmid=3995244 |doi= |url=}}</ref> | |||
**[[Tc-99m]] labeled sulfur used for [[Functional imaging|functional imaging techniques]] provides some indication of [[Liver|hepatic]] function | |||
** 99mTc sulfur [[colloid]] is normally taken up by cells of the [[reticuloendothelial system]] | |||
**Cirrhosis: heterogeneity in the uptake of [[Technetium-99m|99mTc sulfur colloid]] by the [[liver]] and increased uptake by the [[spleen]] and [[bone marrow]] provides evidence of [[portal hypertension]]<ref>{{cite journal |author=Kim YS, Cho SW, Lee KJ, ''et al.'' |title=Tc-99m MIBI SPECT is useful for noninvasively predicting the presence of MDR1 gene-encoded P-glycoprotein in patients with hepatocellular carcinoma |journal=Clin Nucl Med |volume=24 |issue=11 |pages=874–9 |pmid=10551471 |doi= |url=}}</ref> | |||
===Angiography=== | |||
* The [[Angiogram|angiographic]] findings of [[Liver|hepatic]] [[perfusion]] are essential in [[Organ transplant|transplant]] assessment, given the variability of [[Liver|hepatic]] drainage from its [[Artery|arterial]] and [[Vein|venous]] supplies. | |||
===Endoscopy=== | |||
* All patients with cirrhosis should undergo a diagnostic endoscopy to document the presence or absence of [[varices]] and to determine the risk for [[Esophageal varices|variceal]] [[Bleeding|hemorrhage]].<ref name="pmid17879356">{{cite journal |author=Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W |title=Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis |journal=[[Hepatology (Baltimore, Md.)]] |volume=46 |issue=3 |pages=922–38 |year=2007 |pmid=17879356 |doi=10.1002/hep.21907 |url=http://dx.doi.org/10.1002/hep.21907 |accessdate=2012-09-06}}</ref><ref name="pmid24328372">{{cite journal |vauthors=Zardi EM, Di Matteo FM, Pacella CM, Sanyal AJ |title=Invasive and non-invasive techniques for detecting portal hypertension and predicting variceal bleeding in cirrhosis: a review |journal=Ann. Med. |volume=46 |issue=1 |pages=8–17 |year=2014 |pmid=24328372 |pmc=4904298 |doi=10.3109/07853890.2013.857831 |url=}}</ref> | |||
* [[Esophageal varices]] are dilated collaterals in the lower [[esophagus]] that interconnect [[Portal venous system|portal]] and [[systemic circulation]] in [[Patient|patients]] with [[portal hypertension]]. | |||
* [[Esophageal varices]] appear as irregular, serpiginous, bluish structures running longitudinally in the [[submucosa]] of the [[esophageal]] wall on [[endoscopy]]. | |||
* It may be difficult to differentiate small [[varices]] from [[esophageal]] folds and [[Endoscopic ultrasound|EUS]] may be helpful. | |||
* Findings on an [[upper endoscopy]] diagnostic of [[esophageal varices]] include:<ref name="pmid27324725">{{cite journal| author=Abby Philips C, Sahney A| title=Oesophageal and gastric varices: historical aspects, classification and grading: everything in one place. | journal=Gastroenterol Rep (Oxf) | year= 2016 | volume= 4 | issue= 3 | pages= 186-95 | pmid=27324725 | doi=10.1093/gastro/gow018 | pmc=4976684 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27324725 }}</ref> | |||
** Visible [[submucosal]] tortuous veins | |||
** Congested [[veins]] without compression during air [[insufflation]] | |||
** Grape-like [[Varicose veins|varicose]] veins that may occlude the [[lumen]]<ref name="pmid8076547">{{cite journal |vauthors=Thakeb F, Salem SA, Abdallah M, el Batanouny M |title=Endoscopic diagnosis of gastric varices |journal=Endoscopy |volume=26 |issue=3 |pages=287–91 |year=1994 |pmid=8076547 |doi=10.1055/s-2007-1008969 |url=}}</ref> | |||
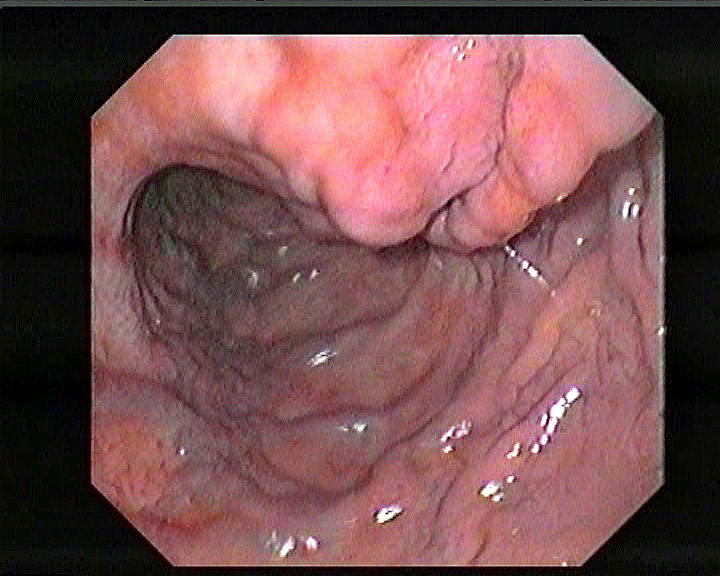
[[image:OEV wale.jpg|thumb|300px|left|Esophageal varices-By Samir, via Wikimedia Commons<ref><"https://commons.wikimedia.org/wiki/File%3AEsophageal_varices_-_wale.jpg">via Wikimedia Commons</ref>]] | |||
[[image:Gastric Varices.jpg|thumb|350px|center|Gastric varices-By Jeremias (Own work), via Wikimedia Commons<ref><"https://commons.wikimedia.org/wiki/File%3AGastric_Varices.jpg">via Wikimedia Commons</ref>]] | |||
<br> | |||
* The presence of [[varices]] in patients with cirrhosis is considered an independent risk factor for survival.<ref name="pmid6969201">{{cite journal |author=Lebrec D, De Fleury P, Rueff B, Nahum H, Benhamou JP |title=Portal hypertension, size of esophageal varices, and risk of gastrointestinal bleeding in alcoholic cirrhosis |journal=[[Gastroenterology]] |volume=79 |issue=6 |pages=1139–44 |year=1980 |pmid=6969201 |doi= |url= |accessdate=2012-09-07}}</ref> | |||
* The appearance of [[esophageal varices]] is not diagnostic of [[portal hypertension]] and does not allow for differentiation between [[portal hypertension]] secondary to cirrhosis, pre-[[Liver sinusoid|sinusoidal]] hypertension, or [[Portal vein|portal]] or [[splenic vein]] [[thrombosis]]. | |||
* Majority of patients with cirrhosis develop [[varices]] and approximately one third [[Bleeding|bleed]] at some point.<ref name="pmid7026343">{{cite journal |author=Christensen E, Fauerholdt L, Schlichting P, Juhl E, Poulsen H, Tygstrup N |title=Aspects of the natural history of gastrointestinal bleeding in cirrhosis and the effect of prednisone |journal=[[Gastroenterology]] |volume=81 |issue=5 |pages=944–52 |year=1981 |pmid=7026343 |doi= |url= |accessdate=2012-09-07}}</ref> | |||
* The most popular model used to target [[Patient|patients]] with high risk of [[Esophageal varices|variceal]] [[Bleeding|bleed]] is devised by the North Italian Endoscopic Club for the Study and Treatment of [[esophageal varices]].<ref name="pmid3262200">{{cite journal |author= |title=Prediction of the first variceal hemorrhage in patients with cirrhosis of the liver and esophageal varices. A prospective multicenter study |journal=[[The New England Journal of Medicine]] |volume=319 |issue=15 |pages=983–9 |year=1988 |pmid=3262200 |doi=10.1056/NEJM198810133191505 |url=http://www.nejm.org/doi/abs/10.1056/NEJM198810133191505?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed |accessdate=2012-09-07}}</ref> | |||
* The severity of the underlying [[liver]] disease, presence or absence of red markings on the [[varices]], and [[Esophageal varices|variceal]] size are the most important risk factors for [[bleeding]]. | |||
* [[Gastroscopy]] ([[Endoscopy|endoscopic]] examination of the [[esophagus]], stomach and [[duodenum]]) is performed in patients with cirrhosis to exclude the possibility of [[esophageal varices]]. | |||
* In patients with [[varices]], [[Prophylaxis|prophylactic]] therapy may include: | |||
** Local therapy: | |||
*** [[Sclerotherapy]] | |||
*** [[Esophageal varices|Variceal]] [[Banding (medical)|banding]] | |||
** Medical therapy: | |||
*** [[Beta blockers]] | |||
====Endoscopic Ultrasound (EUS)==== | |||
* [[Varices]] may be seen within the [[submucosa]] of the [[esophagus]] and in the periesophageal or perigastric soft tissue.<ref name="pmid2184080">{{cite journal |author=Yasuda K, Cho E, Nakajima M, Kawai K |title=Diagnosis of submucosal lesions of the upper gastrointestinal tract by endoscopic ultrasonography |journal=[[Gastrointestinal Endoscopy]] |volume=36 |issue=2 Suppl |pages=S17–20 |year=1990 |pmid=2184080 |doi= |url= |accessdate=2012-09-07}}</ref> | |||
* In the esophagus, [[Endoscopic ultrasound|EUS]] does not appear to be superior to [[endoscopy]] in the detection of [[esophageal varices]]. | |||
* [[Endoscopic ultrasound|EUS]] is invaluable in differentiating [[gastric varices]] from [[Submucosa|submucosal]] [[Tumor|tumors]] and prominent [[Stomach|gastric]] folds. | |||
* The role of [[Endoscopic ultrasound|EUS]] in determining whether or not [[varices]] are obliterated is under evaluation. | |||
* [[Endoscopic ultrasound|EUS]] is a very safe procedure with a complication rate of approximately 0.05%. | |||
* The major complication of [[Endoscopic ultrasound|EUS]] is [[perforation]], which is related to the relatively large diameter and stiffness of the [[Endoscopy|endoscope]] used. | |||
====ERCP==== | |||
* If a [[Bile duct|biliary]] pathology ([[primary sclerosing cholangitis]] - [[PSC]]) is suspected, [[Endoscopic retrograde cholangiopancreatography|ERCP]] may be performed. | |||
* [[Magnetic resonance cholangiopancreatography|MRCP]] (MRI of [[Bile duct|biliary tract]] and [[pancreas]]) is usually sufficient for diagnosis, but [[Endoscopic retrograde cholangiopancreatography|ERCP]] allows for particular interventions, such as placement of a biliary [[stent]] or extraction of [[gallstones]]. | |||
=== Three dimensional portal venography === | |||
* Three dimensional [[portal]] [[venography]] may be helpful in the diagnosis of [[Esophageal varices|gasteroesophageal varices]]. | |||
* Findings on a [[portal]] [[venography]] diagnostic of [[esophageal varices]] include:<ref name="pmid18373819">{{cite journal| author=Agarwal A, Jain M| title=Multidetector CT portal venography in evaluation of portosystemic collateral vessels. | journal=J Med Imaging Radiat Oncol | year= 2008 | volume= 52 | issue= 1 | pages= 4-9 | pmid=18373819 | doi=10.1111/j.1440-1673.2007.01903.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18373819 }}</ref><ref name="pmid12235335">{{cite journal| author=Kang HK, Jeong YY, Choi JH, Choi S, Chung TW, Seo JJ et al.| title=Three-dimensional multi-detector row CT portal venography in the evaluation of portosystemic collateral vessels in liver cirrhosis. | journal=Radiographics | year= 2002 | volume= 22 | issue= 5 | pages= 1053-61 | pmid=12235335 | doi=10.1148/radiographics.22.5.g02se011053 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12235335 }}</ref> | |||
** Reverse flow in [[Portocaval anastomoses|porto-systemic shunts]] | |||
** [[Collateral]] [[Vein|veins]] draining into [[Inferior vena cava|inferior vena cava (IVC)]] | |||
** Other [[collateral]] [[veins]] | |||
[[image:Venography.png|thumb|600px|left|Venography Source:Open-i<ref>{{cite web |url=https://openi.nlm.nih.gov/detailedresult.php?img=PMC3859884_kjped-56-500-g001&req=4 |title=(A) Angiographic portography revealed portal vein, coro | Open-i |format= |work= |accessdate=}}</ref>]] | |||
[[image:Portal-vein-anatomy.jpg|thumb|500px|center|Venography-Case courtesy of Dr Omar Bashir, via radiopaedia.org<ref name="https://radiopaedia.org/">Radiopaedia.org. From the case <"https://radiopaedia.org/cases/16761">rID: 16761</ref>]] | |||
<br> | |||
<br> | |||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
[[Category:Gastroenterology]] | |||
[[Category:Hepatology]] | |||
[[Category:Disease]] | |||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
Latest revision as of 15:05, 14 December 2017
|
Cirrhosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case studies |
|
Cirrhosis other imaging findings On the Web |
|
American Roentgen Ray Society Images of Cirrhosis other imaging findings |
|
Risk calculators and risk factors for Cirrhosis other imaging findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Aditya Govindavarjhulla, M.B.B.S. [2] Sudarshana Datta, MD [3]
Overview
Tc-99m labeled sulfur may be used in nuclear imaging to provide some indication of hepatic function in cirrhotic patients. In candidates for liver transplant, CTA is used to asses the drainage of the liver. All patients with cirrhosis must undergo a diagnostic endoscopy for the evaluation of varices. Gastric endoscopy is an option if gastric varices are suspected, and endoscopic ultrasound may also help in the visualization of varices. ERCP is performed if a biliary pathology such as primary sclerosing cholangitis is suspected as the underlying cause of cirrhosis.
Other Imaging Findings
Nuclear Imaging
- Radionuclide testing may be useful in the diagnosis of cirrhosis:[1][2]
- Tc-99m labeled sulfur used for functional imaging techniques provides some indication of hepatic function
- 99mTc sulfur colloid is normally taken up by cells of the reticuloendothelial system
- Cirrhosis: heterogeneity in the uptake of 99mTc sulfur colloid by the liver and increased uptake by the spleen and bone marrow provides evidence of portal hypertension[3]
Angiography
- The angiographic findings of hepatic perfusion are essential in transplant assessment, given the variability of hepatic drainage from its arterial and venous supplies.
Endoscopy
- All patients with cirrhosis should undergo a diagnostic endoscopy to document the presence or absence of varices and to determine the risk for variceal hemorrhage.[4][5]
- Esophageal varices are dilated collaterals in the lower esophagus that interconnect portal and systemic circulation in patients with portal hypertension.
- Esophageal varices appear as irregular, serpiginous, bluish structures running longitudinally in the submucosa of the esophageal wall on endoscopy.
- It may be difficult to differentiate small varices from esophageal folds and EUS may be helpful.
- Findings on an upper endoscopy diagnostic of esophageal varices include:[6]
- Visible submucosal tortuous veins
- Congested veins without compression during air insufflation
- Grape-like varicose veins that may occlude the lumen[7]

- The presence of varices in patients with cirrhosis is considered an independent risk factor for survival.[10]
- The appearance of esophageal varices is not diagnostic of portal hypertension and does not allow for differentiation between portal hypertension secondary to cirrhosis, pre-sinusoidal hypertension, or portal or splenic vein thrombosis.
- Majority of patients with cirrhosis develop varices and approximately one third bleed at some point.[11]
- The most popular model used to target patients with high risk of variceal bleed is devised by the North Italian Endoscopic Club for the Study and Treatment of esophageal varices.[12]
- The severity of the underlying liver disease, presence or absence of red markings on the varices, and variceal size are the most important risk factors for bleeding.
- Gastroscopy (endoscopic examination of the esophagus, stomach and duodenum) is performed in patients with cirrhosis to exclude the possibility of esophageal varices.
- In patients with varices, prophylactic therapy may include:
- Local therapy:
- Medical therapy:
Endoscopic Ultrasound (EUS)
- Varices may be seen within the submucosa of the esophagus and in the periesophageal or perigastric soft tissue.[13]
- In the esophagus, EUS does not appear to be superior to endoscopy in the detection of esophageal varices.
- EUS is invaluable in differentiating gastric varices from submucosal tumors and prominent gastric folds.
- The role of EUS in determining whether or not varices are obliterated is under evaluation.
- EUS is a very safe procedure with a complication rate of approximately 0.05%.
- The major complication of EUS is perforation, which is related to the relatively large diameter and stiffness of the endoscope used.
ERCP
- If a biliary pathology (primary sclerosing cholangitis - PSC) is suspected, ERCP may be performed.
- MRCP (MRI of biliary tract and pancreas) is usually sufficient for diagnosis, but ERCP allows for particular interventions, such as placement of a biliary stent or extraction of gallstones.
Three dimensional portal venography
- Three dimensional portal venography may be helpful in the diagnosis of gasteroesophageal varices.
- Findings on a portal venography diagnostic of esophageal varices include:[14][15]
- Reverse flow in porto-systemic shunts
- Collateral veins draining into inferior vena cava (IVC)
- Other collateral veins


References
- ↑ Nishikawa H, Osaki Y (2015). "Liver Cirrhosis: Evaluation, Nutritional Status, and Prognosis". Mediators Inflamm. 2015: 872152. doi:10.1155/2015/872152. PMC 4606163. PMID 26494949.
- ↑ McLaren MI, Fleming JS, Walmsley BH, Ackery DM, Taylor I, Karran SJ (1985). "Dynamic liver scanning in cirrhosis". Br J Surg. 72 (5): 394–6. PMID 3995244.
- ↑ Kim YS, Cho SW, Lee KJ; et al. "Tc-99m MIBI SPECT is useful for noninvasively predicting the presence of MDR1 gene-encoded P-glycoprotein in patients with hepatocellular carcinoma". Clin Nucl Med. 24 (11): 874–9. PMID 10551471.
- ↑ Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W (2007). "Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis". Hepatology (Baltimore, Md.). 46 (3): 922–38. doi:10.1002/hep.21907. PMID 17879356. Retrieved 2012-09-06.
- ↑ Zardi EM, Di Matteo FM, Pacella CM, Sanyal AJ (2014). "Invasive and non-invasive techniques for detecting portal hypertension and predicting variceal bleeding in cirrhosis: a review". Ann. Med. 46 (1): 8–17. doi:10.3109/07853890.2013.857831. PMC 4904298. PMID 24328372.
- ↑ Abby Philips C, Sahney A (2016). "Oesophageal and gastric varices: historical aspects, classification and grading: everything in one place". Gastroenterol Rep (Oxf). 4 (3): 186–95. doi:10.1093/gastro/gow018. PMC 4976684. PMID 27324725.
- ↑ Thakeb F, Salem SA, Abdallah M, el Batanouny M (1994). "Endoscopic diagnosis of gastric varices". Endoscopy. 26 (3): 287–91. doi:10.1055/s-2007-1008969. PMID 8076547.
- ↑ <"https://commons.wikimedia.org/wiki/File%3AEsophageal_varices_-_wale.jpg">via Wikimedia Commons
- ↑ <"https://commons.wikimedia.org/wiki/File%3AGastric_Varices.jpg">via Wikimedia Commons
- ↑ Lebrec D, De Fleury P, Rueff B, Nahum H, Benhamou JP (1980). "Portal hypertension, size of esophageal varices, and risk of gastrointestinal bleeding in alcoholic cirrhosis". Gastroenterology. 79 (6): 1139–44. PMID 6969201.
|access-date=requires|url=(help) - ↑ Christensen E, Fauerholdt L, Schlichting P, Juhl E, Poulsen H, Tygstrup N (1981). "Aspects of the natural history of gastrointestinal bleeding in cirrhosis and the effect of prednisone". Gastroenterology. 81 (5): 944–52. PMID 7026343.
|access-date=requires|url=(help) - ↑ "Prediction of the first variceal hemorrhage in patients with cirrhosis of the liver and esophageal varices. A prospective multicenter study". The New England Journal of Medicine. 319 (15): 983–9. 1988. doi:10.1056/NEJM198810133191505. PMID 3262200. Retrieved 2012-09-07.
- ↑ Yasuda K, Cho E, Nakajima M, Kawai K (1990). "Diagnosis of submucosal lesions of the upper gastrointestinal tract by endoscopic ultrasonography". Gastrointestinal Endoscopy. 36 (2 Suppl): S17–20. PMID 2184080.
|access-date=requires|url=(help) - ↑ Agarwal A, Jain M (2008). "Multidetector CT portal venography in evaluation of portosystemic collateral vessels". J Med Imaging Radiat Oncol. 52 (1): 4–9. doi:10.1111/j.1440-1673.2007.01903.x. PMID 18373819.
- ↑ Kang HK, Jeong YY, Choi JH, Choi S, Chung TW, Seo JJ; et al. (2002). "Three-dimensional multi-detector row CT portal venography in the evaluation of portosystemic collateral vessels in liver cirrhosis". Radiographics. 22 (5): 1053–61. doi:10.1148/radiographics.22.5.g02se011053. PMID 12235335.
- ↑ "(A) Angiographic portography revealed portal vein, coro | Open-i".
- ↑ Radiopaedia.org. From the case <"https://radiopaedia.org/cases/16761">rID: 16761