Cilostazol
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Gerald Chi
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
CONTRAINDICATION
See full prescribing information for complete Boxed Warning.
* Cilostazol and several of its metabolites are inhibitors of phosphodiesterase III. Several drugs with this pharmacologic effect have caused decreased survival compared to placebo in patients with class III-IV congestive heart failure. Cilostazol is contraindicated in patients with congestive heart failure of any severity.
|
Overview
Cilostazol is a phosphodiesterase 3 (PDE3) inhibitor and platelet aggregation inhibitor that is FDA approved for the {{{indicationType}}} of intermittent claudication, as indicated by an increased walking distance. There is a Black Box Warning for this drug as shown here. Common adverse reactions include palpitations, peripheral edema, tachyarrhythmia, abdominal pain, diarrhea, indigestion, decreased platelet aggregation, backache, myalgia, dizziness, headache, cough, pharyngitis, and rhinitis.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Intermittent Claudication
- Dosing Information
- 100 mg PO bid, taken at least half an hour before or two hours after breakfast and dinner.
- A dose of 50 mg PO bid should be considered during coadministration of such inhibitors of CYP3A4 as ketoconazole, itraconazole, erythromycin and diltiazem, and during coadministration of such inhibitors of CYP2C19 as omeprazole.
- Patients may respond as early as 2 to 4 weeks after the initiation of therapy, but treatment for up to 12 weeks may be needed before a beneficial effect is experienced.
- Discontinuation of Therapy
- The available data suggest that the dosage of Cilostazol can be reduced or discontinued without rebound (i.e., platelet hyperaggregability).
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Secondary Prophylaxis of Noncardioembolic Ischemic Stroke or TIA
- Developed by: American College of Chest Physicians (ACCP)
- Dosing Information
- In patients with a history of noncardioembolic ischemic stroke or TIA, ACCP recommends long-term treatment with aspirin (75-100 mg once daily), clopidogrel (75 mg once daily), aspirin/extended-release dipyridamole (25 mg/200 mg bid), or Cilostazol (100 mg bid) over no antiplatelet therapy (Grade 1A), oral anticoagulants (Grade 1B), the combination of clopidogrel plus aspirin (Grade 1B), or triflusal (Grade 2B).
- Of the recommended antiplatelet regimens, ACCP suggests clopidogrel or aspirin/extended-release dipyridamole over aspirin (Grade 2B) or Cilostazol (Grade 2C).
Elective Percutaneous Coronary Intervention with Bare-Metal or Drug-Eluting Stent
- Developed by: American College of Chest Physicians (ACCP)
- Dosing Information
- Use of low-dose aspirin 75 to 100 mg daily and clopidogrel 75 mg daily alone is recommended, rather than Cilostazol in addition to these drugs (Grade 1B).
- Aspirin 75 to 100 mg daily and clopidogrel 75 mg daily as part of dual antiplatelet therapy is suggested, rather than the use of either drug with Cilostazol (Grade 1B).
- Cilostazol 100 mg twice daily as substitute for either low-dose aspirin 75 to 100 mg daily or clopidogrel 75 mg daily as part of a dual antiplatelet regimen is suggested in patients with an allergy or intolerance of either drug class (Grade 2C).
Non–Guideline-Supported Use
Primary Prophylaxis of Cerebrovascular Accident
- Dosing Information
Prophylaxis of Femoral Artery Occlusion After Percutaneous Coronary Intervention
- Dosing Information
- Cilostazol 200 mg/day plus aspirin 100 mg/day significantly reduced the rate of restenosis of femoropopliteal lesions, and significantly improved event-free survival at 12 months after percutaneous transluminal angioplasty with provisional nitinol stenting when compared with use of aspirin alone.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
- The safety and effectiveness of Cilostazole in pediatric patients have not been established.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Cilostazol in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Cilostazol in pediatric patients.
Contraindications
- Congestive heart failure of any severity
- Hemostatic disorders or active pathologic bleeding, such as bleeding peptic ulcer and intracranial bleeding
- Hypersensitivity to any of its components
Warnings
|
CONTRAINDICATION
See full prescribing information for complete Boxed Warning.
* Cilostazol and several of its metabolites are inhibitors of phosphodiesterase III. Several drugs with this pharmacologic effect have caused decreased survival compared to placebo in patients with class III-IV congestive heart failure. Cilostazol is contraindicated in patients with congestive heart failure of any severity.
|
Precautions
- Hematologic Adverse Reactions
- Rare cases have been reported of thrombocytopenia or leukopenia progressing to agranulocytosis when Cilostazol was not immediately discontinued. The agranulocytosis, however, was reversible on discontinuation of Cilostazol.
- Use with Clopidogrel
- There is limited information with respect to the efficacy or safety of the concurrent use of Cilostazol and clopidogrel, a platelet-aggregation inhibiting drug indicated for use in patients with peripheral arterial disease. Although it cannot be determined whether there was an additive effect on bleeding times during concomitant administration with Cilostazol and clopidogrel, caution is advised for checking bleeding times during coadministration.
- Hepatic Impairment
- Patients with moderate or severe hepatic impairment have not been studied in clinical trials. Special caution is advised when Cilostazol is used in such patients.
- Renal Impairment
- Patients on dialysis have not been studied, but, it is unlikely that Cilostazol can be removed efficiently by dialysis because of its high protein binding (95-98%).
- Special caution is advised when Cilostazol is used in patients with severe renal impairment: estimated creatinine clearance < 25 mL/min.
- Use with other antiplatelet agents
- Cilostazol inhibits platelet aggregation but in a reversible manner. Caution is advised in patients at risk of bleeding from surgery or pathologic processes. Platelet aggregability returns to normal within 96 hours of stopping Cilostazol. Caution is advised in patients receiving both Cilostazol and any other antiplatelet agent, or in patients with thrombocytopenia.
- Cardiovascular Toxicity
- Repeated oral administration of Cilostazol to dogs (30 or more mg/kg/day for 52 weeks, 150 or more mg/kg/day for 13 weeks, and 450 mg/kg/day for 2 weeks), produced cardiovascular lesions that included endocardial hemorrhage, hemosiderin deposition and fibrosis in the left ventricle, hemorrhage in the right atrial wall, hemorrhage and necrosis of the smooth muscle in the wall of the coronary artery, intimal thickening of the coronary artery, and coronary arteritis and periarteritis. At the lowest dose associated with cardiovascular lesions in the 52-week study, systemic exposure (AUC) to unbound Cilostazol was less than that seen in humans at the maximum recommended human dose (MRHD) of 100 mg b.i.d. Similar lesions have been reported in dogs following the administration of other positive inotropic agents (including PDE III inhibitors) and/or vasodilating agents. No cardiovascular lesions were seen in rats following 5 or 13 weeks of administration of Cilostazol at doses up to 1500 mg/kg/day. At this dose, systemic exposures (AUCs) to unbound Cilostazol were only about 1.5 and 5 times (male and female rats, respectively) the exposure seen in humans at the MRHD. Cardiovascular lesions were also not seen in rats following 52 weeks of administration of Cilostazol at doses up to 150 mg/kg/day. At this dose, systemic exposures (AUCs) to unbound Cilostazol were about 0.5 and 5 times (male and female rats, respectively) the exposure in humans at the MRHD. In female rats, Cilostazol AUCs were similar at 150 and 1500 mg/kg/day. Cardiovascular lesions were also not observed in monkeys after oral administration of Cilostazol for 13 weeks at doses up to 1800 mg/kg/day. While this dose of Cilostazol produced pharmacologic effects in monkeys, plasma Cilostazol levels were less than those seen in humans given the MRHD, and those seen in dogs given doses associated with cardiovascular lesions.
Adverse Reactions
Clinical Trials Experience
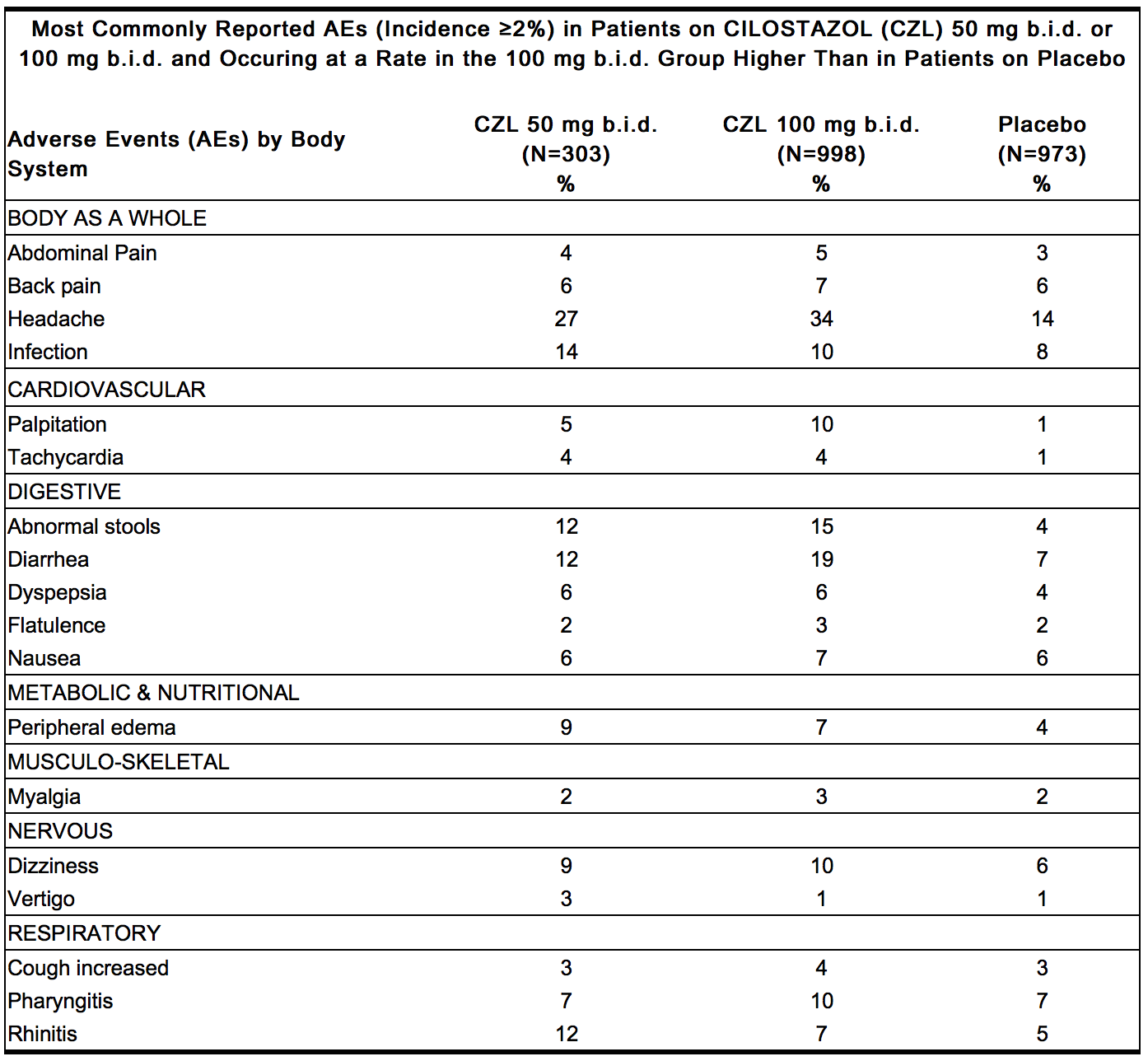
- Adverse events were assessed in eight placebo-controlled clinical trials involving 2274 patients exposed to either 50 or 100 mg b.i.d. Cilostazol (n=1301) or placebo (n=973), with a median treatment duration of 127 days for patients on Cilostazol and 134 days for patients on placebo.
- The only adverse event resulting in discontinuation of therapy in ≥ 3% of patients treated with Cilostazol 50 or 100 mg b.i.d. was headache, which occurred with an incidence of 1.3%, 3.5%, and 0.3% in patients treated with Cilostazol 50 mg b.i.d., 100 mg b.i.d, or placebo, respectively. Other frequent causes of discontinuation included palpitation and diarrhea, both 1.1% for Cilostazol (all doses) versus 0.1% for placebo.
- The most commonly reported adverse events, occurring in ≥ 2% of patients treated with Cilostazol 50 or 100 mg b.i.d., are shown in the table (below).
- Other events seen with an incidence of ≥ 2%, but occurring in the placebo group at least as frequently as in the 100 mg b.i.d. group were: asthenia, hypertension, vomiting, leg cramps, hypesthesia, paresthesia, dyspnea, rash, hematuria, urinary tract infection, flu syndrome, angina pectoris, arthritis, and bronchitis.
- Less frequent adverse events (<2%) that were experienced by patients exposed to Cilostazol 50 mg b.i.d. or 100 mg b.i.d. in the eight controlled clinical trials and that occurred at a frequency in the 100 mg b.i.d. group greater than in the placebo group, regardless of suspected drug relationship, are listed below.
Body as a Whole
Chills, face edema, fever, generalized edema, malaise, neck rigidity, pelvic pain, retroperitoneal hemorrhage.
Cardiovascular
Atrial fibrillation, atrial flutter, cerebral infarct, cerebral ischemia, congestive heart failure, cardiac arrest, hemorrhage, hypotension, myocardial infarction, myocardial ischemia, nodal arrhythmia, postural hypotension, supraventricular tachycardia, syncope, varicose vein, vasodilation, ventricular extrasystoles, ventricular tachycardia.
Digestive
Anorexia, cholelithiasis, colitis, duodenal ulcer, duodenitis, esophageal hemorrhage, esophagitis, increased GGT, gastritis, gastroenteritis, gum hemorrhage, hematemesis, melena, peptic ulcer, periodontal abscess, rectal hemorrhage, peptic ulcer, tongue edema.
Endocrine
Hematologic and Lymphatic
Anemia, ecchymosis, iron deficiency anemia, polycythemia, purpura.
Metabolic and Nutritional
Increased creatinine, gout, hyperlipemia, hyperuricemia.
Musculoskeletal
Arthralgia, bone pain, bursitis.
Nervous
Respiratory
Asthma, epistaxis, hemoptysis, pneumonia, sinusitis.
Skin and Appendages
Dry skin, furunculosis, skin hypertrophy, urticaria.
Special Senses
Amblyopia, blindness, conjunctivitis, diplopia, ear pain, eye hemorrhage, retinal hemorrhage, tinnitus.
Urogenital
Albuminuria, cystitis, urinary frequency, vaginal hemorrhage, vaginitis.
Postmarketing Experience
The following events have been reported spontaneously from worldwide postmarketing experience since the launch of Cilostazol in the U.S.
Blood and Lymphatic System Disorders
Agranulocytosis, aplastic anemia, granulocytopenia, thrombocytopenia, leukopenia, bleeding tendency
Cardiac Disorders
Torsades de pointes, QTc prolongation (torsades de pointes and QTc prolongation occurred in patients with cardiac disorders, e.g. complete atrioventricular block, heart failure and bradyarrhythmia, when treated with Cilostazol. Cilostazol was used "off label" due to its positive chronotropic action.)
Gastrointestinal Disorders
Gastrointestinal hemorrhage
General Disorders and Administration Site Conditions
Hepatobiliary disorders
Hepatic dysfunction/Abnormal liver function tests, jaundice
Injury, Poisoning and Procedural Complications
Extradural hematoma and subdural hematoma
Investigations
Blood glucose increased, blood uric acid increased, platelet count decreased, white blood cell count decreased, increase in BUN (blood urea nitrogen increased), blood pressure increase
Nervous System Disorders
Intracranial hemorrhage, cerebral hemorrhage, cerebrovascular accident
Respiratory, Thoracic and Mediastinal Disorders
Pulmonary hemorrhage, interstitial pneumonia
Skin and Subcutaneous Tissue Disorders
Subcutaneous hemorrhage, pruritus, skin eruptions including Stevens-Johnson syndrome, skin drug eruption (dermatitis medicamentosa)
Vascular Disorders
Subacute thrombosis (These cases of subacute thrombosis occurred in patients treated with aspirin and "off label" use of Cilostazol for prevention of thrombotic complication after coronary stenting.)
Drug Interactions
- Since Cilostazol is extensively metabolized by cytochrome P-450 isoenzymes, caution should be exercised when Cilostazol is coadministered with inhibitors of CYP3A4 such as ketoconazole and erythromycin or inhibitors of CYP2C19 such as omeprazole. Pharmacokinetic studies have demonstrated that omeprazole and erythromycin significantly increased the systemic exposure of Cilostazol and/or its major metabolites. Population pharmacokinetic studies showed higher concentrations of Cilostazol among patients concurrently treated with diltiazem, an inhibitor of CYP3A4. Cilostazol does not, however, appear to cause increased blood levels of drugs metabolized by CYP3A4, as it had no effect on lovastatin, a drug with metabolism very sensitive to CYP3A4 inhibition.
Aspirin
- Short-term (≤4 days) coadministration of aspirin with Cilostazol increased the inhibition of ADP-induced ex vivo platelet aggregation by 22% - 37% when compared to either aspirin or Cilostazol alone. Short-term (≤ 4 days) coadministration of aspirin with Cilostazol increased the inhibition of arachidonic acid-induced ex vivo platelet aggregation by 20% compared to Cilostazol alone and by 48% compared to aspirin alone. However, short-term coadministration of aspirin with Cilostazol had no clinically significant impact on PT, aPTT, or bleeding time compared to aspirin alone. Effects of long-term coadministration in the general population are unknown. In eight randomized, placebo-controlled, double-blind clinical trials, aspirin was coadministered with Cilostazol to 201 patients. The most frequent doses and mean durations of aspirin therapy were 75-81 mg daily for 137 days (107 patients) and 325 mg daily for 54 days (85 patients). There was no apparent increase in incidence of hemorrhagic adverse effects in patients taking Cilostazol and aspirin compared to patients taking placebo and equivalent doses of aspirin.
Warfarin
- The cytochrome P-450 isoenzymes involved in the metabolism of R-warfarin are CYP3A4, CYP1A2, and CYP2C19, and in the metabolism of S-warfarin, CYP2C9. Cilostazol did not inhibit either the metabolism or the pharmacologic effects (PT, aPTT, bleeding time, or platelet aggregation) of R- and S-warfarin after a single 25 mg dose of warfarin. The effect of concomitant multiple dosing of warfarin and Cilostazol on the pharmacokinetics and pharmacodynamics of both drugs is unknown.
Clopidogrel
- Multiple doses of clopidogrel do not significantly increase steady state plasma concentrations of Cilostazol.
Inhibitors of CYP3A4
Strong Inhibitors of CYP3A4
- A priming dose of ketoconazole 400 mg (a strong inhibitor of CYP3A4), was given one day prior to coadministration of single doses of ketoconazole 400 mg and Cilostazol 100 mg. This regimen increased Cilostazol Cmax by 94% and AUC by 117%. Other strong inhibitors of CYP3A4, such as itraconazole, fluconazole, miconazole, fluvoxamine, fluoxetine, nefazodone, and sertraline, would be expected to have a similar effect.
Moderate Inhibitors of CYP3A4
- Erythromycin and other macrolide antibiotics: Erythromycin is a moderately strong inhibitor of CYP3A4. Coadministration of erythromycin 500 mg q 8 h with a single dose of Cilostazol 100 mg increased Cilostazol Cmax by 47% and AUC by 73%. Inhibition of Cilostazol metabolism by erythromycin increased the AUC of 4 '-trans-hydroxy-Cilostazol by 141%. Other macrolide antibiotics (e.g., clarithromycin), but not all (e.g., azithromycin), would be expected to have a similar effect.
- Diltiazem: Diltiazem 180 mg decreased the clearance of Cilostazol by ~30%. Cilostazol Cmax increased ~30% and AUC increased ~40%.
- Grapefruit juice: Grapefruit juice increased the Cmax of Cilostazol by ~50%, but had no effect on AUC.
Inhibitors of CYP2C19
Omeprazole
- Coadministration of omeprazole did not significantly affect the metabolism of Cilostazol, but the systemic exposure to 3,4- dehydro-Cilostazol was increased by 69%, probably the result of omeprazole's potent inhibition of CYP2C19.
Quinidine
- Concomitant administration of quinidine with a single dose of Cilostazol 100 mg did not alter Cilostazol pharmacokinetics.
Lovastatin
- The concomitant administration of lovastatin with Cilostazol decreases Cilostazol Css, max and AUC by 15%. There is also a decrease, although nonsignificant, in Cilostazol metabolite concentrations. Coadministration of Cilostazol with lovastatin increases lovastatin and β-hydroxi lovastatin AUC approximately 70%. This is most likely clinically insignificant.
Use in Specific Populations
Pregnancy
- Pregnancy Category C
- In a rat developmental toxicity study, oral administration of 1000 mg Cilostazol/kg/day was associated with decreased fetal weights, and increased incidences of cardiovascular, renal, and skeletal anomalies (ventricular septal, aortic arch and subclavian artery abnormalities, renal pelvic dilation, 14th rib, and retarded ossification). At this dose, systemic exposure to unbound Cilostazol in nonpregnant rats was about 5 times the exposure in humans given the MRHD. Increased incidences of ventricular septal defect and retarded ossification were also noted at 150 mg/kg/day (5 times the MRHD on a systemic exposure basis). In a rabbit developmental toxicity study, an increased incidence of retardation of ossification of the sternum was seen at doses as low as 150 mg/kg/day. In nonpregnant rabbits given 150 mg/kg/day, exposure to unbound Cilostazol was considerably lower than that seen in humans given the MRHD, and exposure to 3,4-dehydro-Cilostazol was barely detectable.
- When Cilostazol was administered to rats during late pregnancy and lactation, an increased incidence of stillborn and decreased birth weights of offspring was seen at doses of 150 mg/kg/day (5 times the MRHD on a systemic exposure basis).
- There are no adequate and well-controlled studies in pregnant women.
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Cilostazol in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Cilostazol during labor and delivery.
Nursing Mothers
- Transfer of Cilostazol into milk has been reported in experimental animals (rats). Because of the potential risk to nursing infants, a decision should be made to discontinue nursing or to discontinue Cilostazol.
Pediatric Use
- The safety and effectiveness of Cilostazol in pediatric patients have not been established.
Geriatic Use
- Of the total number of subjects (n=2274) in clinical studies of Cilostazol, 56 percent were 65-years-old and over, while 16 percent were 75-years-old and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. Pharmacokinetic studies have not disclosed any age-related effects on the absorption, distribution, metabolism, and elimination of Cilostazol and its metabolites.
Gender
There is no FDA guidance on the use of Cilostazol with respect to specific gender populations.
Race
There is no FDA guidance on the use of Cilostazol with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Cilostazol in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Cilostazol in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Cilostazol in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Cilostazol in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
Monitoring
There is limited information regarding Monitoring of Cilostazol in the drug label.
IV Compatibility
There is limited information regarding IV Compatibility of Cilostazol in the drug label.
Overdosage
Acute Overdose
Signs and Symptoms
- Information on acute overdosage with Cilostazol in humans is limited. The signs and symptoms of an acute overdose can be anticipated to be those of excessive pharmacologic effect: severe headache, diarrhea, hypotension, tachycardia, and possibly cardiac arrhythmias. The oral LD50 of Cilostazol is >5 g/kg in mice and rats and >2 g/kg in dogs.
Management
- The patient should be carefully observed and given supportive treatment. Since Cilostazol is highly protein-bound, it is unlikely that it can be efficiently removed by hemodialysis or peritoneal dialysis.
Chronic Overdose
There is limited information regarding Chronic Overdose of Cilostazol in the drug label.
Pharmacology

| |
Cilostazol
| |
| Systematic (IUPAC) name | |
| 6-[4-(1-cyclohexyl-1H-tetrazol-5-yl)butoxy]- 3,4-dihydro-2(1H)-quinolinone | |
| Identifiers | |
| CAS number | |
| ATC code | B01 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 369.46 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Protein binding | 95–98% |
| Metabolism | Hepatic (CYP3A4- and CYP2C19-mediated) |
| Half life | 11–13 hours |
| Excretion | Renal |
| Therapeutic considerations | |
| Pregnancy cat. |
C(US) |
| Legal status | |
| Routes | Oral |
Mechanism of Action
- The mechanism of the effects of Cilostazol on the symptoms of intermittent claudication is not fully understood. Cilostazol and several of its metabolites are cyclic AMP (cAMP) phosphodiesterase III inhibitors (PDE III inhibitors), inhibiting phosphodiesterase activity and suppressing cAMP degradation with a resultant increase in cAMP in platelets and blood vessels, leading to inhibition of platelet aggregation and vasodilation, respectively. Cilostazol reversibly inhibits platelet aggregation induced by a variety of stimuli, including thrombin, ADP, collagen, arachidonic acid, epinephrine, and shear stress. Effects on circulating plasma lipids have been examined in patients taking Cilostazol. After 12 weeks, as compared to placebo, Cilostazol 100 mg b.i.d. produced a reduction in triglycerides of 29.3 mg/dL (15%) and an increase in HDL-cholesterol of 4 mg/dL (≥10%).
Cardiovascular Effects
- Cilostazol affects both vascular beds and cardiovascular function. It produces nonhomogeneous dilation of vascular beds, with greater dilation in femoral beds than in vertebral, carotid or superior mesenteric arteries. Renal arteries were not responsive to the effects of Cilostazol.
- In dogs or cynomolgous monkeys, Cilostazol increased heart rate, myocardial contractile force, and coronary blood flow as well as ventricular automaticity, as would be expected for a PDE III inhibitor. Left ventricular contractility was increased at doses required to inhibit platelet aggregation. A-V conduction was accelerated. In humans, heart rate increased in a dose-proportional manner by a mean of 5.1 and 7.4 beats per minute in patients treated with 50 and 100 mg b.i.d., respectively. In 264 patients evaluated with Holter monitors, numerically more Cilostazol-treated patients had increases in ventricular premature beats and nonsustained ventricular tachycardia events than did placebo-treated patients; the increases were not dose-related.
Structure
- Cilostazol is a quinolinone derivative that inhibits cellular phosphodiesterase (more specific for phosphodiesterase III). The molecular formula of Cilostazol is C20H27N5O2, and its molecular weight is 369.46. Cilostazol is 6-[4-(1-cyclohexyl-1H-tetrazol-5-yl) butoxy]- 3,4-dihydro-2(1H)-quinolinone. The structural formula is:
- Cilostazol occurs as white to off-white crystals or as a crystalline powder that is slightly soluble in methanol and ethanol, and is practically insoluble in water, 0.1 N HCl, and 0.1 N NaOH.
- Cilostazol tablets for oral administration are available in 50 mg and 100 mg round, white debossed tablets. Each tablet, in addition to the active ingredient, contains the following inactive ingredients: carboxymethylcellulose calcium, pregelantized starch, hypromellose, magnesium stearate, microcrystalline cellulose, and sodium lauryl sulfate.
Pharmacodynamics
Plasma Protein and Erythrocyte Binding
- Cilostazol is 95 - 98% protein bound, predominantly to albumin. The mean percent binding for 3,4-dehydro-Cilostazol is 97.4% and for 4 '-trans-hydroxy-Cilostazol is 66%. Mild hepatic impairment did not affect protein binding. The free fraction of Cilostazol was 27% higher in subjects with renal impairment than in normal volunteers. The displacement of Cilostazol from plasma proteins by erythromycin, quinidine, warfarin, and omeprazole was not clinically significant.
Pharmacokinetics
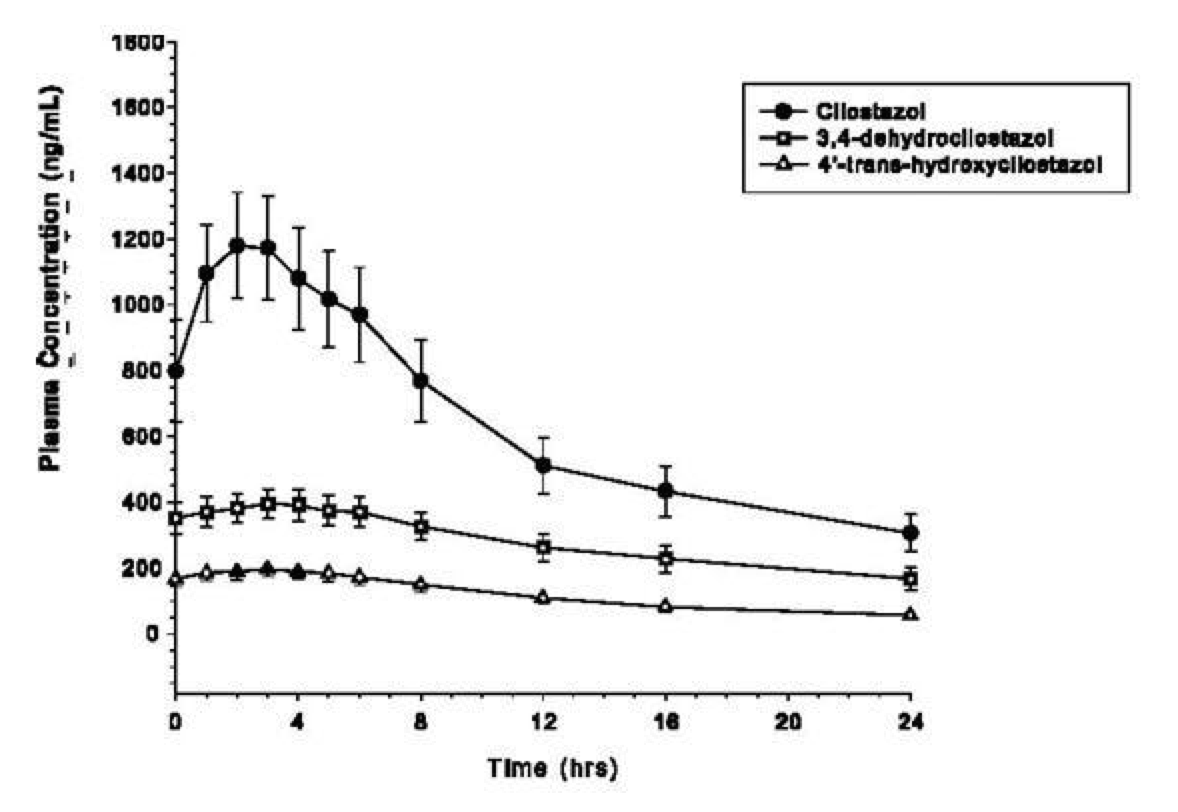
- Cilostazol is absorbed after oral administration. A high fat meal increases absorption, with an approximately 90% increase in Cmax and a 25% increase in AUC. Absolute bioavailability is not known. Cilostazol is extensively metabolized by hepatic cytochrome P-450 enzymes, mainly 3A4, and, to a lesser extent, 2C19, with metabolites largely excreted in urine. Two metabolites are active, with one metabolite appearing to account for at least 50% of the pharmacologic (PDE III inhibition) activity after administration of Cilostazol. Pharmacokinetics are approximately dose proportional. Cilostazol and its active metabolites have apparent elimination half-lives of about 11-13 hours. Cilostazol and its active metabolites accumulate about 2-fold with chronic administration and reach steady state blood levels within a few days. The pharmacokinetics of Cilostazol and its two major active metabolites were similar in healthy normal subjects and patients with intermittent claudication due to peripheral arterial disease (PAD).
- The mean ± SEM plasma concentration-time profile at steady state after multiple dosing of Cilostazol 100 mg b.i.d. is shown below:
Metabolism and Excretion
- Cilostazol is eliminated predominately by metabolism and subsequent urinary excretion of metabolites. Based on in vitro studies, the primary isoenzymes involved in Cilostazol's metabolism are CYP3A4 and, to a lesser extent, CYP2C19. The enzyme responsible for metabolism of 3,4-dehydro-Cilostazol, the most active of the metabolites, is unknown.
- Following oral administration of 100 mg radiolabeled Cilostazol, 56% of the total analytes in plasma was Cilostazol, 15% was 3,4-dehydro-Cilostazol (4-7 times as active as Cilostazol), and 4% was 4 '-trans-hydroxy-Cilostazol (one fifth as active as Cilostazol). The primary route of elimination was via the urine (74%), with the remainder excreted in feces (20%). No measurable amount of unchanged Cilostazol was excreted in the urine, and less than 2% of the dose was excreted as 3, 4- dehydro-Cilostazol. About 30% of the dose was excreted in urine as 4 '-trans-hydroxy-Cilostazol. The remainder was excreted as other metabolites, none of which exceeded 5%. There was no evidence of induction of hepatic microenzymes.
Special Populations
Age and Gender
- The total and unbound oral clearances, adjusted for body weight, of Cilostazol and its metabolites were not significantly different with respect to age and/or gender across a 50-to- 80-year-old age range.
Smokers
- Population pharmacokinetic analysis suggests that smoking decreased Cilostazol exposure by about 20%.
Hepatic Impairment
- The pharmacokinetics of Cilostazol and its metabolites were similar in subjects with mild hepatic disease as compared to healthy subjects. Patients with moderate or severe hepatic impairment have not been studied.
Renal Impairment
- The total pharmacologic activity of Cilostazol and its metabolites was similar in subjects with mild to moderate renal impairment and in normal subjects. Severe renal impairment increases metabolite levels and alters protein binding of the parent and metabolites. The expected pharmacologic activity, however, based on plasma concentrations and relative PDE III inhibiting potency of parent drug and metabolites, appeared little changed. Patients on dialysis have not been studied, but, it is unlikely that Cilostazol can be removed efficiently by dialysis because of its high protein binding (95 - 98%).
Nonclinical Toxicology
- Carcinogenesis, Mutagenesis, Impairment of Fertility
- Dietary administration of Cilostazol to male and female rats and mice for up to 104 weeks, at doses up to 500 mg/kg/day in rats and 1000 mg/kg/day in mice, revealed no evidence of carcinogenic potential. The maximum doses administered in both rat and mouse studies were, on a systemic exposure basis, less than the human exposure at the MRHD of the drug. Cilostazol tested negative in bacterial gene mutation, bacterial DNA repair, mammalian cell gene mutation, and mouse in vivo bone marrow chromosomal aberration assays. It was, however, associated with a significant increase in chromosomal aberrations in the in vitro Chinese Hamster Ovary Cell assay.
- Cilostazol did not affect fertility or mating performance of male and female rats at doses as high as 1000 mg/kg/day.
- At this dose, systemic exposures (AUCs) to unbound Cilostazol were less than 1.5 times in males, and about 5 times in females, the exposure in humans at the MRHD.
Clinical Studies
- The ability of Cilostazol to improve walking distance in patients with stable intermittent claudication was studied in eight large, randomized, placebo-controlled, double-blind trials of 12 to 24 weeks' duration using dosages of 50 mg b.i.d. (n=303), 100 mg b.i.d. (n=998), and placebo (n=973). Efficacy was determined primarily by the change in maximal walking distance from baseline (compared to change on placebo) on one of several standardized exercise treadmill tests.
- Compared to patients treated with placebo, patients treated with Cilostazol 50 or 100 mg b.i.d. experienced statistically significant improvements in walking distances both for the distance before the onset of claudication pain and the distance before exercise-limiting symptoms supervened (maximal walking distance). The effect of Cilostazol on walking distance was seen as early as the first on-therapy observation point of two or four weeks.
- The following figure depicts the percent mean improvement in maximal walking distance, at study end for each of the eight studies.
- Across the eight clinical trials, the range of improvement in maximal walking distance in patients treated with Cilostazol 100 mg b.i.d., expressed as the percent mean change from baseline, was 28% to 100%. The corresponding changes in the placebo group were -10% to 41%.
- The Walking Impairment Questionnaire, which was administered in six of the eight clinical trials, assesses the impact of a therapeutic intervention on walking ability. In a pooled analysis of the six trials, patients treated with either Cilostazol 100 mg b.i.d. or 50 mg b.i.d. reported improvements in their walking speed and walking distance as compared to placebo. Improvements in walking performance were seen in the various subpopulations evaluated, including those defined by gender, smoking status, diabetes mellitus, duration of peripheral artery disease, age, and concomitant use of beta-blockers or calcium channel blockers. Cilostazol has not been studied in patients with rapidly progressing claudication or in patients with leg pain at rest, ischemic leg ulcers, or gangrene. Its long-term effects on limb preservation and hospitalization have not been evaluated.
- A randomized, double-blind, placebo-controlled Phase IV study was conducted to assess the long-term effects of Cilostazol, with respect to mortality and safety, in 1,439 patients with intermittent claudication and no heart failure. The trial stopped early due to enrollment difficulties and a lower than expected overall death rate. With respect to mortality, the observed 36-month Kaplan-Meier event rate for deaths on study drug with a median time on study drug of 18 months was 5.6% (95% CI of 2.8 to 8.4%) on Cilostazol and 6.8% (95% CI of 1.9 to 11.5%) on placebo. These data appear to be sufficient to exclude a 75% increase in the risk of mortality on Cilostazol, which was the a priori study hypothesis.
How Supplied
- Cilostazol is supplied as 50 mg and 100 mg tablets. The 50 mg tablets are white, round, debossed with B167 on one side and 50 on the other, and are provided in bottles of 60 tablets (NDC #51991-167-06) and 1000 tablets (NDC #51991-167-10).
- The 100 mg tablets are white, round, debossed with B168 on one side and 100 on the other, and provided in bottles of 60 tablets (NDC #51991-168-06) and 1000 tablets (NDC #51991-168-10).
- Store Cilostazol tablets at 20°-25°C (68°-77°F); excursions permitted to 15°-30°C (59°-86°F)
Storage
There is limited information regarding Cilostazol Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Cilostazol |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Cilostazol |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- What is Cilostazol for?
- Cilostazol may improve the symptoms of patients with a medical condition called intermittent claudication.
- What is intermittent claudication?
- Intermittent claudication is pain in the legs that occurs with walking and disappears with rest. It occurs because narrowing or blockage of the arteries decreases blood flow to the legs. The decreased blood flow does not supply enough oxygen to the leg muscles during walking, resulting in these painful leg cramps.
- What treatments are available for intermittent claudication?
- The three main treatments available for intermittent claudication are:
- Exercise. Your doctor may advise an exercise program.
- Medication. Your doctor may prescribe a medication such as Cilostazol.
- Surgery. Your doctor may recommend a surgical procedure to bypass the blocked segment of the artery. Another procedure is called a percutaneous transluminal angioplasty. In this procedure, a catheter (a flexible tube) is inserted into the artery to reduce the blockage and improve blood flow.
- How does Cilostazol work?
- The exact way that many drugs work is not well understood. Although how Cilostazol works is not completely clear, its main effects are to dilate (widen) the arteries supplying blood to the legs and to decrease the ability of platelets in the blood to stick together. Platelets are particles that circulate in the blood and play a role in clotting.
- Cilostazol may reduce the leg pain that patients with intermittent claudication experience, allowing them to walk farther before their leg pain occurs.
- Improvement in symptoms may occur as soon as 2 weeks, but could take up to 12 weeks. If you have not noticed any benefit from Cilostazol after 12 weeks you and your doctor may wish to discuss other forms of treatment.
- Sometimes blood vessel disease of the legs causes pain at rest or breakdown of skin in the leg. Cilostazol has not been shown to work in patients with these problems.
- Who should not take Cilostazol?
- Patients who have congestive heart failure (CHF) must not take Cilostazol. The most common symptoms of CHF are shortness of breath and swelling of the legs. However, other conditions may also cause these symptoms. It is important that you discuss with your doctor whether you have CHF.
- How should Cilostazol be taken?
- Follow your doctor's advice about how to take Cilostazol.
- You should take Cilostazol twice a day, at least one half-hour before or two hours after breakfast and dinner. Take Cilostazol at about the same times each day.
- Do not share Cilostazol with anyone else. It was prescribed only for you.
- Keep Cilostazol and all drugs out of the reach of children.
- Can Cilostazol be taken with other drugs?
- Certain drugs and foods can increase the amount of Cilostazol in the blood. Because of this, your doctor may adjust your dose of Cilostazol or even stop it if you are taking or are going to take one of the following medications.
Precautions with Alcohol
- Alcohol-Cilostazol interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Pletal®[3]
Look-Alike Drug Names
- N/A[4]
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Shinoda-Tagawa, T. (2002-02). "A phosphodiesterase inhibitor, Cilostazol, prevents the onset of silent brain infarction in Japanese subjects with Type II diabetes". Diabetologia. 45 (2): 188–194. doi:10.1007/s00125-001-0740-2. ISSN 0012-186X. PMID 11935149. Unknown parameter
|coauthors=ignored (help); Check date values in:|date=(help) - ↑ Ahn, C. W. (2001-04). "Decrease in carotid intima media thickness after 1 year of Cilostazol treatment in patients with type 2 diabetes mellitus". Diabetes Research and Clinical Practice. 52 (1): 45–53. ISSN 0168-8227. PMID 11182215. Unknown parameter
|coauthors=ignored (help); Check date values in:|date=(help) - ↑ "Cilostazol tablet".
- ↑ "http://www.ismp.org". External link in
|title=(help)
{{#subobject:
|Page Name=Cilostazol |Pill Name=No image.jpg |Drug Name= |Pill Ingred=|+sep=; |Pill Imprint= |Pill Dosage= |Pill Color=|+sep=; |Pill Shape= |Pill Size (mm)= |Pill Scoring= |Pill Image= |Drug Author= |NDC=
}}
{{#subobject:
|Label Page=Cilostazol |Label Name=Cilostazol06.png
}}
{{#subobject:
|Label Page=Cilostazol |Label Name=Cilostazol07.png
}}
{{#subobject:
|Label Page=Cilostazol |Label Name=Cilostazol08.png
}}