Chronic hypertension medical therapy: Difference between revisions
(→Choice of Initial Agent: broke content into two sections) |
|||
| Line 336: | Line 336: | ||
====Choice of Initial Agent==== | ====Choice of Initial Agent==== | ||
[[Clinical practice guideline]]s vary in their recommendations for selection of initial medication<ref name="pmid29133354">{{cite journal| author=Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C et al.| title=2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. | journal=Hypertension | year= 2018 | volume= 71 | issue= 6 | pages= 1269-1324 | pmid=29133354 | doi=10.1161/HYP.0000000000000066 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29133354 }} </ref><ref name="pmid28135725">{{cite journal| author=Qaseem A, Wilt TJ, Rich R, Humphrey LL, Frost J, Forciea MA et al.| title=Pharmacologic Treatment of Hypertension in Adults Aged 60 Years or Older to Higher Versus Lower Blood Pressure Targets: A Clinical Practice Guideline From the American College of Physicians and the American Academy of Family Physicians. | journal=Ann Intern Med | year= 2017 | volume= 166 | issue= 6 | pages= 430-437 | pmid=28135725 | doi=10.7326/M16-1785 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28135725 }} [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=&cmd=prlinks&id=28418540 Review in: Ann Intern Med. 2017 Apr 18;166(8):JC38] </ref><ref name="pmid24352797">{{cite journal| author=James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J et al.| title=2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). | journal=JAMA | year= 2014 | volume= 311 | issue= 5 | pages= 507-20 | pmid=24352797 | doi=10.1001/jama.2013.284427 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24352797 }} </ref><ref name="pmid23817082">{{cite journal| author=Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M et al.| title=2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). | journal=J Hypertens | year= 2013 | volume= 31 | issue= 7 | pages= 1281-357 | pmid=23817082 | doi=10.1097/01.hjh.0000431740.32696.cc | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23817082 }} </ref>. | |||
=====Selecting medication based on patient demographics===== | |||
[[Image:Materson et al. NEJM 1994. PMID 8177286.jpg|right|500px]] | |||
<br style="clear:left" />Some authors have proposed that either the renin level or the renin level indexed to urinary sodium excretion in 24 hours.<ref name="pmid4355699">{{cite journal| author=Laragh JH| title=Vasoconstriction-volume analysis for understanding and treating hypertension: the use of renin and aldosterone profiles. | journal=Am J Med | year= 1973 | volume= 55 | issue= 3 | pages= 261-74 | pmid=4355699 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=4355699 }} </ref><ref name="pmid4337477">{{cite journal| author=Laragh JH, Baer L, Brunner HR, Buhler FR, Sealey JE, Vaughan ED| title=Renin, angiotensin and aldosterone system in pathogenesis and management of hypertensive vascular disease. | journal=Am J Med | year= 1972 | volume= 52 | issue= 5 | pages= 633-52 | pmid=4337477 | doi= | pmc= | url= }} </ref> However, the Veterans Affairs Cooperative trial suggests the initial drug may be better selected based on the patient's age, race, and gender.<ref name="pmid8177286">{{cite journal |author=Materson BJ, Reda DJ |title=Correction: single-drug therapy for hypertension in men |journal=N. Engl. J. Med. |volume=330 |issue=23 |pages=1689 |year=1994 |pmid=8177286 |doi=}}</ref><ref name="pmid9777817">{{cite journal |author=Preston RA, Materson BJ, Reda DJ, ''et al'' |title=Age-race subgroup compared with renin profile as predictors of blood pressure response to antihypertensive therapy. Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents |journal=JAMA |volume=280 |issue=13 |pages=1168–72 |year=1998 |pmid=9777817 |doi=}}</ref> The patient's demographic roughly corresponds with their [[renin]] profile, but is more predictive than the renin profile.<ref name="pmid9777817"/> In the Veterans Affairs Cooperative, among the high renin demographic (young whites), diuretics had similar efficacy to placebo; whereas in the low renin demographic (older blacks), the [[Angiotensin-converting enzyme inhibitor|ace-inhibitors]] had similar efficacy to placebo in the Veterans Affairs Cooperative Study Group on Antihypertensive Agents (see figure).<ref name="pmid8177286"/> | |||
=====Selecting fixed-dose combination pills===== | |||
Two [[cohort study | cohort studies]] suggest that fixed-dose combination pills enhance adherence when compared to monotherapy<ref name="pmid28050754">{{cite journal| author=Lauffenburger JC, Landon JE, Fischer MA| title=Effect of Combination Therapy on Adherence Among US Patients Initiating Therapy for Hypertension: a Cohort Study. | journal=J Gen Intern Med | year= 2017 | volume= 32 | issue= 6 | pages= 619-625 | pmid=28050754 | doi=10.1007/s11606-016-3972-z | pmc=5442007 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28050754 }} </ref><ref name="pmid29889841">{{cite journal| author=Verma AA, Khuu W, Tadrous M, Gomes T, Mamdani MM| title=Fixed-dose combination antihypertensive medications, adherence, and clinical outcomes: A population-based retrospective cohort study. | journal=PLoS Med | year= 2018 | volume= 15 | issue= 6 | pages= e1002584 | pmid=29889841 | doi=10.1371/journal.pmed.1002584 | pmc=5995349 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29889841 }} </ref>. The increased adherence may lead to improved clinical outcomes<ref name="pmid29889841"/>. Therefore, it would not be unreasonable to consider starting combination therapy in order to increase patient compliance, a known barrier to hypertension pharmacotherapy. | |||
====JNC7: Compelling Indications and Choice of Antihypertensive Agents<ref name="pmid14656957">Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL et al. (2003) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=14656957 Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.] ''Hypertension'' 42 (6):1206-52.[http://dx.doi.org/10.1161/01.HYP.0000107251.49515.c2 DOI:10.1161/01.HYP.0000107251.49515.c2] PMID: [http://pubmed.gov/14656957 14656957]</ref>==== | ====JNC7: Compelling Indications and Choice of Antihypertensive Agents<ref name="pmid14656957">Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL et al. (2003) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=14656957 Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.] ''Hypertension'' 42 (6):1206-52.[http://dx.doi.org/10.1161/01.HYP.0000107251.49515.c2 DOI:10.1161/01.HYP.0000107251.49515.c2] PMID: [http://pubmed.gov/14656957 14656957]</ref>==== | ||
Revision as of 20:36, 16 April 2019
|
Chronic Hypertension Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Chronic hypertension medical therapy On the Web |
|
Directions to Hospitals Treating Chronic hypertension medical therapy |
|
Risk calculators and risk factors for Chronic hypertension medical therapy |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [5]; Associate Editor(s)-In-Chief: Yazan Daaboul; Serge Korjian; Ryan Norman; Arzu Kalayci, M.D. [6]
Overview
There has been a recent shift away from the administration of thiazide-type diuretics as first line therapy for patients with isolated essential hypertension to the use of any anti-hypertensive agent for isolated essential hypertension. Nonetheless, the administration of specific classes of drugs is indicated in particular patient populations with particular comorbid disease states.
Medical Therapy
To review the 2017 AHA/ACC guidelines on HTN, click here.
Blood Pressure Targets of Therapy
Recommendations from recent clinical practice guidelines are tabulated below. However, treated based on underlying risk rather than a blood pressure target may be more effective[1]. The logic supporting a target of 130/80 mm Hg has been disputed[2] and the Cochrane Collaboration found insufficient evidence to determine a treatment goal for adults[3] or adults over 65 years of age[4].
If the goal if 130/80, proper measurement includes (distilled from Table 8 of the guidelines[5], executive summary[6]):
- having the patient sit quietly for 5 minutes before a reading is taken
- supporting the limb used to measure BP
- ensuring the BP cuff is at heart level
- using the correct cuff size
- for auscultatory readings, deflating the cuff slowly
- the timing of BP measurements in relation to ingestion of the patient’s medication should be standardized
- a single reading is inadequate for clinical decision-making. An average of 2 to 3 BP measurements obtained on 2 to 3 separate occasions will minimize random error and provide a more accurate basis for estimation of BP.
If the above measurement methods are not use, a preliminary study from Kaiser Northern California suggests a target of 140 mm Hg[7].
| Goal >= 60 years old | Goal < 60 years old | |
|---|---|---|
| AHA/ACC/others, 2017[6] | 130/80* | 130/80* |
| ACP/AAFP, 2017[8] | 150 or 140 if high risk | Not applicable |
| JNC-8, 2014[9]; HEDIS | 150/90† | 140/90 |
| * Treat if > 140/90 or 130/80 if high risk which is defined as existing cardiovascular disease or 10-year cardiovascular risk ≥10%
† Treat to 140/90 if age >=60 with DMII or CKD. (HEDIS does not apply CKD to this adjustment.) | ||
Newer randomized controlled trials have identified conflicting benefits to more intensive therapy.
| Patients | BP target in intervention group | Final BP in intervention group | Primary outcome (composite) (Hazard ratio) | |||
|---|---|---|---|---|---|---|
| Baseline blood pressure | Estimated cardiac risk (calculated with pooled cohort equation) |
Outcome rate in the control group | ||||
| ACCORD, 2010 | 140/76 | 9% for anglo women and 23% for anglo men | 2.1% per year | SBP 120 vs 140 | 119/64 | 0.88 (95% CI: 0.73 to 1.06) |
| SPRINT, 2015 | 140/78 | 16% for anglo women and 23% for anglo men (20% overall) | 2.2% per year | SBP 120 vs 140 | 121/67 | 0.75 (95% CI: 0.64 to 0.89) |
| HOPE-3, 2016 | 138/82 | 16% for anglo women and 23% for anglo men | 4.4% over 5.6 years | No target BP. Intervention group all received candesartan 16 mg per day plus hydrochlorothiazide 12.5 mg per day |
128/76 | 0.93 (95% CI: 0.79 to 1.10) |
| Notes | ||||||
- In the SPRINT randomized control trial, patients with an average blood pressure of 140/78 mm Hg and at high risk for CVD but who do not have a history of stroke or diabetes, intensive BP control (target SBP <120 mm Hg) that lowered systolic blood pressure to an average of 121/67 mm Hg improved CV outcomes and overall survival compared to standard therapy, while modestly increasing the risk of some serious adverse events[10].
- Assuming the average patient in this trial was not diabetic, 50% were smokers (per their publication)), 33% were women, and LDL was 113 (per their publication Friedrwald estimate is 191 - 53 - 125/5)) the estimated 10 year cardiovascular risk is 12% for anglo women and 20% for anglo men.
- In the HOPE-3 trial randomized controlled trial, patients with average blood pressure of 138/82 mm HG and with intermediate risk who did not have cardiovascular disease lowering systolic blood pressure to an average of 128 mm Hg was insignificantly beneficial. [11]
- Assuming the average patients in this trial was a nonsmoker and not diabetic, the estimated 10 year cardiovascular risk is 10% for anglo women and 19% for anglo men.
- Benefit was found in a subgroup analysis of patients with systolic blood pressure above 144 mm Hg (mean 154 mm Hg).
- In the ACCORD (Action to Control Cardiovascular Risk in Diabetes) randomized controlled trial patients with average blood pressure of 140/76 mm Hg and diabetes did not benefit from targeting a systolic blood pressure of less than 120 mm Hg (average 119/64 mm Hg), as compared with less than 140 mm Hg.[12]
- Assuming the average patients in this trial was a nonsmoker and was diabetic, the estimated 10 year cardiovascular risk is 9% for anglo women and 23% for anglo men.
Debate exists on how low should physicians target blood pressure in their patients especially in light of studies that have shown a J or U-shaped curve phenomenon associated with hypertension treatment where low and very high blood pressure values are associated with increased risk of cardiovascular events.[13] A less strict target in diabetic and elderly patients is in the new ADA and ESH/ESC 2013 clinical practice guidelines respectively. This rationale is supported by the fact that lower SBP targets in diabetic patients have not been shown to generate better outcomes.[14] Similarly, treatment of stage 1 hypertension in elderly patients and targeting SBP values to <140 mmHg have not been well substantiated and may sometimes carry more risk than benefit.[15]
American College of Cardiology / American Heart Association
The ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA 2017 clinical practice guidelines[5], executive summary[6], and underlying systematic review[6] by the ACC/AHA taskforce recommend a treatment goal for everyone is <130/80 mm Hg:
| Definition | Treatment | |
|---|---|---|
| Elevated blood pressure | Systolic BP, 120–129 mm Hg - and - Diastolic BP, <80 mm Hg |
Lifestyle |
| Stage 1 hypertension | Systolic BP, 130–139 mm Hg - or - Diastolic BP, 80–89 mm Hg |
Lifestyle and Medications if high risk* |
| Stage 2 hypertension |
Systolic BP, ≥140 mm Hg - or - Diastolic BP, ≥90 mm Hg |
Lifestyle and Medications |
| * High risk defined as existing cardiovascular disease or 10-year cardiovascular risk ≥10% (calculator and alternative calculator with facts box) | ||
American College of Physicians / American Academy of Family Physicians
For patients aged 60 or more, the American College of Physicians and American Academy of Family Physicians clinical practice guideline[8] and underlying systematic review[16] from 2017 recommend:
- " initiate treatment in adults aged 60 years or older with systolic blood pressure persistently at or above 150 mm Hg to achieve a target systolic blood pressure of less than 150 mm Hg"
- "consider initiating or intensifying pharmacologic treatment in adults aged 60 years or older with a history of stroke or transient ischemic attack to achieve a target systolic blood pressure of less than 140 mm Hg"
- "consider initiating or intensifying pharmacologic treatment in some adults aged 60 years or older at high cardiovascular risk, based on individualized assessment, to achieve a target systolic blood pressure of less than 140 mm Hg"
Eighth Joint National Committee (JNC 8)
JNC 8 recommendations in 2014 for BP goals:[9]
- Strong evidence for BP goal less than 150/90 mm Hg for patients above age 60.
- Strong evidence exists for a diastolic goal of less than 90 mm Hg for hypertensive patients between ages 30 - 59.
- There is insufficient evidence for patients below age 60 for a systolic goal, or in those below age 30 for a diastolic goal, so the panel recommended a BP of less than 140/90 mm Hg for those groups based on expert opinion.
Approach to Medical Therapy
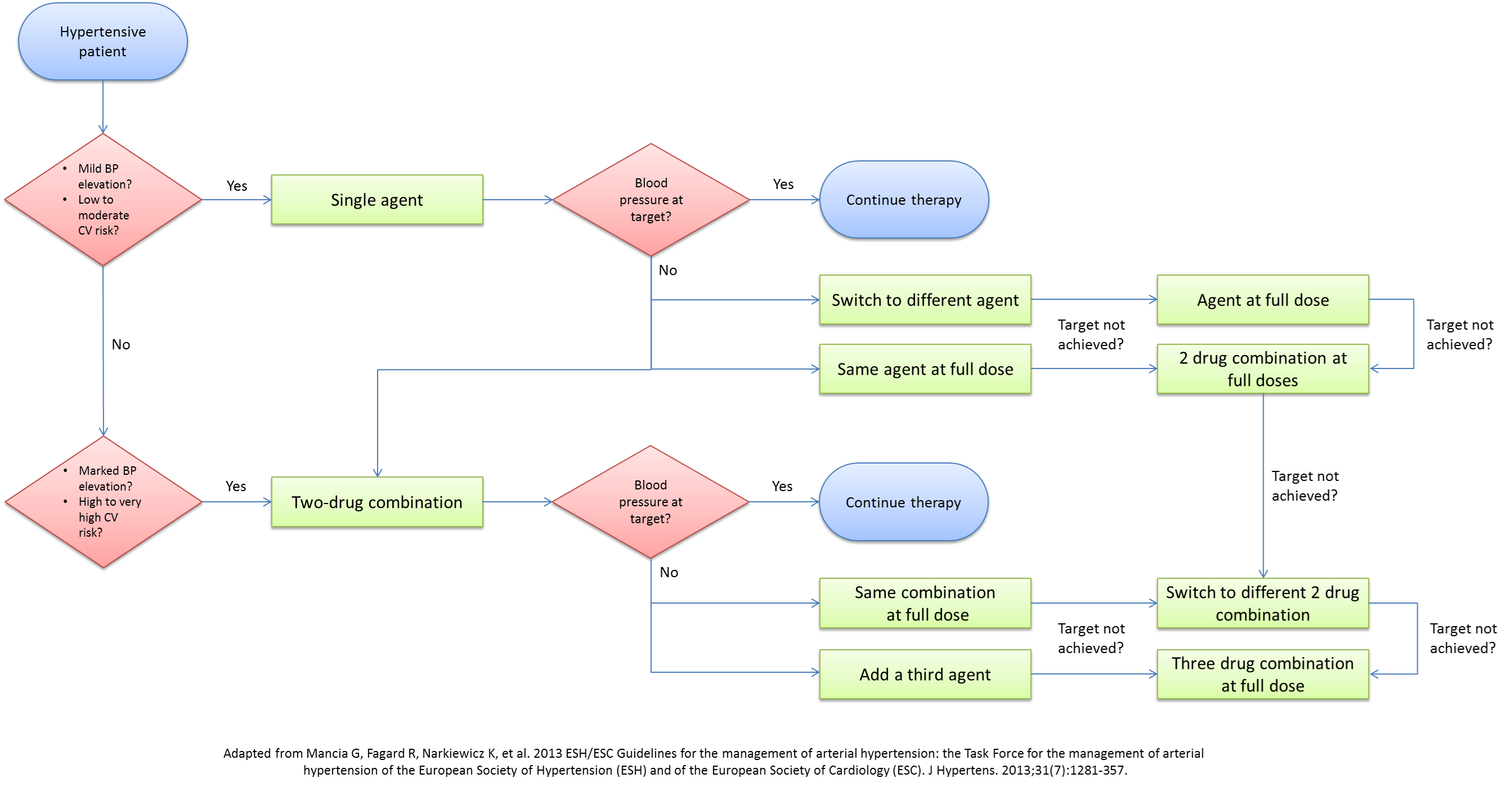
Pharmacologic therapy is normally initiated based on the cardiovascular risk. Failure to achieve BP goals in patients with low and moderate cardiovascular risk after three to six months of non-pharmacologic measures necessitates the initiation of pharmacologic therapy. Medical management should be reserved to patients with BP>140/90 mmHg (except in certain cases discussed below). A lot of debate exists on the optimal approach to the medical management of hypertension. With the multitude of classes and agents that can be used, several questions arise about the single best agent, the optimal combination of agents, and the best step-wise approach to medical management. Although JNC7 tried to address these issues, almost a decade has passed since the release of their recommendations, with a myriad of studies and trials presenting newer compelling evidence to update the current recommendations. The 2013 ESH/ESC guidelines for the management of hypertension have dwelled into these issues and have outlined the rationale behind adopting a new approach. Below are the algorithms for the approach to the medical therapy of hypertension presented by ESH/ESC and JNC8 in 2013.
| Adult aged ≥18 years with hypertension | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Implement lifestyle interventions (continue throughout management) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Set blood pressure goal Inititate BP lowering-medication | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| General population (no diabetes or CKD) | Diabetes or CKD present | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Age ≥60 years | Age <60 years | All ages Diabetes present No CKD | All ages CKD present with or without diabetes | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Blood pressure goal SBP <150 mm Hg DBP <90 mm Hg | Blood pressure goal SBP <140 mm Hg DBP <90 mm Hg | Blood pressure goal SBP <140 mm Hg DBP <90 mm Hg | Blood pressure goal SBP <140 mm Hg DBP <90 mm Hg | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Nonblack | Black | All races | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Initiate thiazide-type diuretic or ACEI or ARB or CCB, alone or in combination | Initiate thiazide-type diuretic or CCB, alone or in combination | Initiate ACEI or ARB, alone or in combination with other drug class. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Select a drug treatment titration strategy A. Maximize 1st medication before adding 2nd OR B. Add 2nd medication before reaching maximum dose of 1st medication OR C. Start with 2 medication classes separately or as fixed-dose combination | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| At goal blood pressure? | Yes | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| No | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Reinforce medication and lifestyle adherence.
For strategies A and B: Add and titrate thiazide-type diuretic or ACEI or ARB or CCB (use medication class not previously selected and avoid combined use of ACEI & ARB). For strategy C: Titrate doses of initial medications to maximum. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| At goal blood pressure? | Yes | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| No | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Reinforce medication and lifestyle adherence.
Add and titrate thiazide-type diuretic or ACEI or ARB or CCB (use medication class not previously selected and avoid combined use of ACEI & ARB). | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| At goal blood pressure? | Yes | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| No | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Reinforce medication and lifestyle adherence.
Add additional medication class (eg, β-blocker, aldosterone antagonist, or others) and/or refer to physician with expertise in HTN management. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| No | At goal blood pressure? | Yes | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Continue current treatment and monitoring. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Antihypertensive Agents & Indications
Common Antihypertensive Agents
Several classes of medications are used in the treatment of hypertension namely diuretics, ACE inhibitors, angiotensin receptor blockers, beta-blockers, alpha-blockers, and direct vasodilators. Below is a list of common oral agents used in the treatment of hypertension.
| Class | Drug | Usual Dose Range (mg/day) |
| Thiazide Diuretics | Chlorothiazide | 125-500 |
| Chlorthalidone | 12.5-25 | |
| Hydrochlorothiazide | 12.5-50 | |
| Polythiazide | 2-4 | |
| Indapamide | 1.25-2.5 | |
| Metolazone | 0.5-5 | |
| Loop Diuretics | Bumetanide | 0.5-2 |
| Furosemide | 20-80 | |
| Torsemide | 2.5-10 | |
| Potassium-sparing Diuretics | Amiloride | 5-10 |
| Triamterene | 50-100 | |
| Aldosterone Receptor Diuretics | Spironolactone | 25-50 |
| Eplerenone | 50-100 | |
| Beta-Blockers | Atenolol | 25-100 |
| Betaxolol | 5-20 | |
| Bisoprolol | 2.5-10 | |
| Metoprolol | 50-100 | |
| Metoprolol extended release | 50-100 | |
| Nadolol | 40-120 | |
| Propranolol | 40-160 | |
| Propranolol long-acting | 60-180 | |
| Timolol | 20-40 | |
| Beta-Blockers with intrinsic sympathomimetic activity | Acebutolol | 200-800 |
| Penbutolol | 10-40 | |
| Pindolol | 10-40 | |
| Combined Alpha- and Beta-Blockers | Carvedilol | 12.5-50 |
| Labetalol | 200-800 | |
| ACE Inhibitors | Benazepril | 10-40 |
| Captopril | 25-100 | |
| Enalapril | 5-40 | |
| Fosinopril | 10-40 | |
| Lisinopril | 10-40 | |
| Moexipril | 7.5-30 | |
| Perindopril | 4-8 | |
| Quinapril | 10-80 | |
| Ramipril | 2.5-20 | |
| Trandolapril | 1-4 | |
| Angiotensin Receptor Blockers | Candesartan | 8-32 |
| Eprosartan | 400-800 | |
| Irbesartan | 150-300 | |
| Losartan | 25-100 | |
| Olmesartan | 20-40 | |
| Telmisartan | 20-80 | |
| Valsartan | 80-320 | |
| Nondihydropyridine Calcium Channel Blockers | Diltiazem extended release | 120-540 |
| Verapamil immediate release | 80-320 | |
| Verapamil long acting | 120-480 | |
| Verapamil | 120-360 | |
| Dihydropyridine Calcium Channel Blockers | Amlodipine | 2.5-10 |
| Felodipine | 2.5-10 | |
| Isradipine | 2.5-10 | |
| Nicardipine sustained release | 60-120 | |
| Nifedipine long-acting | 30-60 | |
| Nisoldipine | 10-40 | |
| Alpha-1 Blockers | Doxazosin | 1-16 |
| Prazosin | 2-20 | |
| Terazosin | 1-20 | |
| Centrally Acting Drugs | Clonidine | 0.1-0.8 |
| Methyldopa | 250-1000 | |
| Reserpine | 0.1-0.25 | |
| Guanfacine | 0.5-2 | |
| Direct Vasodilators | Hydralazine | 25-100 |
| Minoxidil | 2.5-80 |
Choice of Initial Agent
Clinical practice guidelines vary in their recommendations for selection of initial medication[6][8][9][18].
Selecting medication based on patient demographics
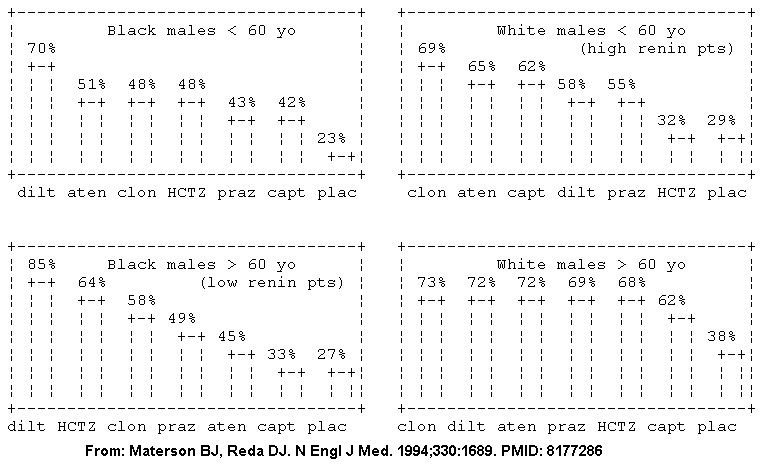
Some authors have proposed that either the renin level or the renin level indexed to urinary sodium excretion in 24 hours.[19][20] However, the Veterans Affairs Cooperative trial suggests the initial drug may be better selected based on the patient's age, race, and gender.[21][22] The patient's demographic roughly corresponds with their renin profile, but is more predictive than the renin profile.[22] In the Veterans Affairs Cooperative, among the high renin demographic (young whites), diuretics had similar efficacy to placebo; whereas in the low renin demographic (older blacks), the ace-inhibitors had similar efficacy to placebo in the Veterans Affairs Cooperative Study Group on Antihypertensive Agents (see figure).[21]
Selecting fixed-dose combination pills
Two cohort studies suggest that fixed-dose combination pills enhance adherence when compared to monotherapy[23][24]. The increased adherence may lead to improved clinical outcomes[24]. Therefore, it would not be unreasonable to consider starting combination therapy in order to increase patient compliance, a known barrier to hypertension pharmacotherapy.
JNC7: Compelling Indications and Choice of Antihypertensive Agents[17]
| Compelling Indication | Recommended Drugs | Clinical Trial Basis |
| Heart failure | Diuretics, Beta blockers, ACEIs, ARBs, Aldosterone antagonist | ACC/AHA Heart Failure Guideline [25]; MERIT-HF [26];COPERNICUS [27]; CIBIS [28]; SOLVD [29]; AIRE [30]; TRACE [31]; ValHEFT [32]; RALES [33] |
| Post-Myocardial infarction | Beta blockers, ACEIs, Aldosterone antagonist | ACC/AHA Post-MI Guideline [34]; BHAT [35]; SAVE [36]; CAPRICORN [37]; EPHESUS [38] |
| High coronary disease risk | Diuretics, Beta blockers, ACEIs, CCBs, | ALLHAT [39]; HOPE[40]; ANBP2 [41]; LIFE [42]; CONVINCE [43] |
| Diabetes | Diuretics, Beta blockers, ACEIs, ARBs, CCBs | NKF-ADA Guideline [44][45];UKPDS [46]; ALLHAT [39] |
| Chronic kidney disease | ACEIs, ARBs | NFK Guideline [45]; Captopril Trial [47]; RENAAL [48]; IDNT [49]; REIN [50]; AASK [51] |
| Recurrent stroke prevention | Diuretics, ACEIs | PROGRESS [52] |
Contraindicated medications
Chronic hypertension is considered an absolute contraindication to the use of the following medications:
Severe uncontrolled arterial hypertension is considered an absolute contraindication to the use of the following medications:
ESH/ESC 2013 Guidelines: Drugs to be Preferred in Specific Conditions [18]
| Patient Characteristic | Drug |
| Asymptomatic organ damage | |
| Left Ventricular Hypertrophy | ACE inhibitor, calcium antagonist, ARB |
| Asymptomatic atherosclerosis | Calcium antagonist, ACE inhibitor |
| Microalbuminuria | ACE inhibitor, ARB |
| Renal dysfunction | ACE inhibitor, ARB |
| Clinical CV event | |
| Previous stroke | Any agent effectively lowering BP |
| Previous myocardial infarction | BB, ACE inhibitor, ARB |
| Angina pectoris | BB, calcium antagonist |
| Heart failure | Diuretic, BB, ACE inhibitor, ARB, mineralocorticoid receptor antagonists |
| Aortic aneurysm | BB |
| Atrial fibrillation, prevention | Consider ARB, ACE inhibitor, BB or mineralocorticoid receptor antagonist |
| Atrial fibrillation, ventricular rate control | BB, non-dihydropyridine calcium antagonist |
| ESRD/proteinuria | ACE inhibitor, ARB |
| Peripheral artery disease | ACE inhibitor, calcium antagonist |
| Other | |
| ISH (elderly) | Diuretic, calcium antagonist |
| Metabolic syndrome | ACE inhibitor, ARB, calcium antagonist |
| Diabetes mellitus | ACE inhibitor, ARB |
| Pregnancy | Methyldopa, BB, calcium antagonist |
| Blacks | Diuretic, calcium antagonist |
Impact of Blood Pressure self-monitoring in Hypertension Control
According to systematic review in 2017 [53], self-monitoring blood pressures alone is not an effective treatment for high blood pressure. However, as an adjunct to interventions such as patient education, medication titration, and lifestyle counselling, self-monitoring blood pressures significantly aids in controlling patient blood pressure. “Overall, self-monitoring was associated with reduced clinic systolic blood pressure (sBP) compared to usual care at 12 months (−3.2 mmHg, [95% CI −4.9, −1.6 mmHg]). However, this effect was strongly influenced by the intensity of co-intervention ranging from no effect with self-monitoring alone (−1.0 mmHg [−3.3, 1.2]), to a 6.1 mmHg (−9.0, −3.2) reduction when monitoring was combined with intensive support.”
This assessment is supported by another systematic review in 2018 [54], who determined that self-monitoring blood pressures significantly helps control patient blood pressure by aiding in physician anti-hypertensive medication titration. “Compared with usual care, the decrease in clinic measured systolic blood pressure at 12 months in patients in both self-monitoring groups was clinically meaningful. The adjusted mean differences vs usual care: self-monitoring alone −3.5 mm Hg [95% CI −5.8 to −1.2]; and telemonitoring −4.7 mm Hg [–7.0 to −2.4]). If sustained, such reductions in blood pressure could be expected to reduce stroke risk by 20% and coronary heart disease risk by 10%.”
Interdisciplinary Approach to Hypertension Management
Recent literature suggests that an interdisciplinary approach to hypertension provides higher control rates and more comprehensive management of hypertension on a population level. [55] [55] Systems-based interventions such as increasing the role of medical assistants and pharmacists in the management of hypertension has shown the most marked improvements in control. Other interventions include single-pill medical therapy, monitoring visits with medical assistants, creating a hypertension registry, and home blood pressure management. [56] [57] [58] [59]
- When a team approach is used to manage hypertension, the addition of pharmacists alone were found to have the most substantial effect on hypertension control at the population level. [58]
- There is conflicting evidence on home-monitoring alone as an effective method for increasing blood pressure control. [60] [53] [61]
- Interventions such as optimizing single pill combination medications or promoting home blood pressure monitoring have not been shown to provide significant improvements in blood pressure when implemented alone.
Management of Hypertension in Special Populations
Diabetic Patients
- According to the American Diabetes Association, BP goal for diabetic patients must be < 140/80 mmHg to reduce the progression of target organ damage but that lower systolic blood pressure targets <130 mmHg can be targeted in younger patients.[14] The recent shift in the approach to hypertension in diabetics proposed by the 2013 ADA guidelines as well as the 2013 ESH/ESC guidelines is supported by the fact that no major trials have consistently achieved a blood pressure level below 130/80 mmHg in diabetics nor have the smaller trials shown any major benefit from intensive treatment to reach that threshold. In parallel to the ADA, the 2013 ESH/ESC guidelines only support a lower DBP goal set at 80-85 mmHg.[18]
- According to the American Diabetes Association, ACEI and ARBs are considered superior agents in diabetic patients for their renal protective effects (delay in both GFR decrease and albuminuria worsening).[62] Although RAAS blockers such as ACEI and ARBs are beneficial their combination can sometimes have significant effects on renal function especially in high risk patients.[63]
- Thiazide-type diuretics were shown to be beneficial in reducing heart disease in diabetic patients.[64] Despite their side effects of worsening hyperglycemia, thiazide-type diuretics were associated with stable target organ damage compared to other anti-hypertensive agents.[65]
- According to the LIFE study, beta-blockers are especially beneficial in diabetic patients with ischemic heart disease despite their controversial role as monotherapy.[66] Even though decreased insulin sensitivity is a side effect, beta-blockers are not absolutely contraindicated in diabetes.[67]
- In the management of hypertension, CCBs are unquestionably useful in the reduction of BP values. However, their role in preventing target organ damage in diabetic patients is inferior to other agents. The ALLHAT study demonstrated that amlodipine, a DHP CCB, was less effective than thiazides in reducing heart failure.[64] Similarly, the ABCD Trial also showed that nisoldipine, a dihydropyridine CCB was less effective than enalapril, an ACEI, in reducing ischemic heart disease.[68]
Chronic Kidney Disease Patients
- Based mostly on the results from meta-analyses of patients with proteinuria showing slower rate of CKD progression when SBP was targeted to <130 mmHg, JNC7 and the National Kidney Foundation recommended a set BP goal below 130/80 mmHg for all CKD patients and the use of more than a single agent for therapy. The recommended treatment regimen usually includes an ACEI or ARB in combination with a loop diuretic. [17]
- In 2012, the KDIGO Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease recommended that diabetic and non-diabetic patients with CKD without proteinuria or microalbuminuria should be treated if their BP measurements are consistently above 140/90 mmHg. Target of treatment in this group is to maintain blood pressure below 140/90 mmHg. In patients with CKD and microalbuminuria or proteinuria, initiation of therapy should be at BP values >130/80 mmHg with target below 130/80 mmHg. The guidelines also advocated the use ACEIs and ARBs in patients with microalbuminuria or proteinuria. Lifestyle modifications proposed included lowering salt intake to <2g per day of sodium, exercise for at least 30 minutes 5 times per week.
- In contrast, the 2013 ESH/ESC guidelines updated their old recommendations, changing the blood pressure target to <140/90 mmHg, no different than the general population. They based their recommendations on three trials[69][70][71] conducted in patients with chronic kidney disease without diabetes, that showed no difference in ESRD progression and all-cause mortality between patients randomized to low BP targets (<130 mmHg) to those randomized to a higher target (<140 mmHg). To note, observational follow-up data from 2 of these studies showed a tendency to lower adverse events in the lower target group especially in patients with proteinuria.[15]
Patients with Metabolic Syndrome
- Metabolic syndrome as a clinical concept is largely debatable, mostly since studies have shown little added benefit of the definition on the predictive power of each of the constitutive individual factors, making recommendations about hypertension treatment in this subpopulation limited.[18]
- Lifestyle modification plays the most important role in anti-hypertensive therapy in patients with metabolic syndrome.
- Persistence of high BP > 140/90 mmHg still warrants pharmacologic therapy.
- Management of dyslipidemia, glucose intolerance, and other concomitant comorbidities is essential for reduction of BP in patients with metabolic syndrome.[67]
Ethnic groups
- African Americans: Enforcement of DASH diet due to its association with greater reduction of BP than other ethnicities.[72] According to the ALLHAT trial that included 15,000 Blacks, diuretics were more effective for African Americans than other classes of anti-hypertensive agents.[64]
- Mexican Americans, other Hispanic Americans, Native Americans, and Asian/Pacific Islanders have been recruited in insufficient numbers in research trials to adequately identify special considerations.[67]
Elderly Patients
- There is particular advantage in weight loss and reduced sodium intake in elderly subjects. Trial of Non-pharmacologic Interventions in the Elderly (TONE) showed that sodium intake of less than 80 mmol per day (2 g of sodium per day or 5 grams of sodium chloride salt) could allow the discontinuation of anti-hypertensive agents in 40% of elderly.[73]
- The 2013 ESH/ESC guidelines modified the approach adopted in 2007 to treat hypertension regardless of age. The new guidelines advocate holding medical therapy for elderly patients with stage 1 hypertension and initiating treatment only in those with stage 2 hypertension or greater. It is also recommended to target a SBP below 150 mmHg rather than 140mmHg. This rationale follows several studies involving elderly patients not achieving blood pressure measurements below 140mmHg. In patients below 80 years of age, treatment can be targeted below 140 mmHg if goal can be tolerated.[18]
- The HYpertension in the Very Elderly Trial (HYVET) showed that in patients older than 80 years-old with SBP >160mmHg, a significant reduction in major CV events and all-cause mortality can be seen by aiming at SBP values <150mmHg. [74]
- The JNC7 guidelines concluded in 2004 that antihypertensive therapy should not be withheld in patients with stage 1 hypertension based on age, even though no RCTs had shown benefits from treatment in this population at the time.
Underserved or vulnerable populations
Underserved or vulnerable populations face additional socioeconomic barriers to hypertension control including decreased clinic resources, limited access to care, and inconsistent follow-up.
A recent cohort study with a time-series analysis conducted in San Francisco safety net clinics adapted the 2013 Kaiser protocol[56] to fit the specific needs of safety-net clinics by focusing on 4 specific modifications[75]:
- Creating a hypertension patient registry
- Simplified intensification of therapy
- Standardized BP measurements
- Team-based interdisciplinary BP checks by RNs and pharmacists.
Implementation of the modified Kaiser protocol led to an increase in the percent of patients with controlled hypertension from a baseline of 68% to 74% over the course of fifteen months. Overall, the results of this study demonstrated that large-scale hypertension protocols can be successfully applied to high-risk populations[75].
Pregnant Women
- Distinguishing gestational from pre-gestational hypertension in pregnant women is essential. Hypertension is not considered to be caused by pregnancy when it develops before 20 weeks of gestation.[67]
- Hypertensive women who plan to become pregnant should be instructed to use safe anti-hypertensive medications, such as methyldopa preferentially because long-term follow up studies are available. [76] Labetolol and nifedipine are also other treatment options that can be considered in pregnancy.[18]
- Pregnant women with stage 1 hypertension present with low cardiovascular risk and anticipated physiological lowering of blood pressure during pregnancy. Thus healthcare providers might advise mere lifestyle modification as therapy during pregnancy and breast feeding, with caution on excessive weight reduction and with possible restriction of aerobic physical activity.[67]
- The 2013 ESH/ESC guidelines recommend drug treatment of severe hypertension in pregnancy defined as SBP >160 mmHg or DBP >110 mmHg. They also advocate considering treatment in pregnant women with persistant hypertension ≥150/95 mmHg and in symptomatic patients or patients with target organ damage with BP ≥140/90 mmHg.[18]
Patients with Hypertensive Emergency or Urgency
- Hypertensive emergency is defined as high blood pressure causing acute target organ damage. Usually BP exceed 180/20 mmHg, but can sometimes occur at even lower values in patients who do not usually have high blood pressure.
- Hypertensive urgency is defined as a BP > 180/120 mmHg without target organ damage. Hypertensive urgency may or may not be symptomatic.
- Triage to differentiate between hypertensive emergency and urgency is crucial for appropriate management. While hypertensive emergencies require intensive care unit (ICU) admission for close monitoring and aggressive parenteral agents, hypertensive urgencies can be managed in the emergency department with outpatient follow-up for optimization of therapy.[67]
- Treatment is based on titrated intravenous medications that act rapidly but safely especially in avoiding severe hypotension and ischemic organ damage. Nicardipine, sodium nitroprusside, labetalol, furosemide and nitrates are some of the agents used. In certain cases of volume overload-associated hypertensive emergency where diuresis is insufficient, dialysis and ultrafiltration may be of benefit.[18]
- Generally, JNC 7 outlines the acute management of hypertensive emergencies as reduction of a maximum of 25% of mean arterial BP within the first hour followed by decrease of BP to 160/100 within the next 2 to 6 hours. Normalization of blood pressure should occur at a span of 24-48 hours. Rapid decrease in BP might precipitate ischemia caused by target organ damage.[67]
- The 2013 ESH/ESC guidelines do not dwell much into the treatment of hypertensive emergencies due to the lack of evidence considering the small number of cases but recommend that treatment be individualized by the physician.[18]
- Specific clinical situations are considered exceptions to the abovementioned management plan:[67]
- Ischemic stroke will not require immediate BP lowering to maintain cerebral perfusion.
- Aortic dissection requires SBP to be lowered immediately to < 100 mmHg if tolerated followed by rapid specific management.
2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults
General Principles of Drug Therapy
| Class III: Harm |
| "1. Simultaneous use of an ACE inhibitor, ARB, and/or renin inhibitor is potentially harmful and is not recommended to treat adults with hypertension.(Level of Evidence: A) " |
Treatment Threshold and the Use of Cardiovascular Disease (CVD) Risk Estimation to Guide Drug Treatment of Hypertension
| Class I |
| "1. Use of BP-lowering medications is recommended for secondary prevention of recurrent CVD events in patients with clinical CVD and an average SBP of 130 mm Hg or higher or an average DBP of 80 mm Hg or higher, and for primary prevention in adults with an estimated 10-year atherosclerotic cardiovascular disease (ASCVD) risk of 10% or higher and an average SBP 130 mm Hg or higher or an average DBP 80 mm Hg or higher.(Level of Evidence: SBP: A, DBP: C-EO) " |
| "2. Use of BP-lowering medication is recommended for primary prevention of CVD in adults with no history of CVD and with an estimated 10-year ASCVD risk <10% and an SBP of 140 mm Hg or higher or a DBP of 90 mm Hg or higher.(Level of Evidence: C-LD) " |
Blood Pressure (BP) Goal for Patients With Hypertension
| Class I |
| "1. For adults with confirmed hypertension and known CVD or 10-year ASCVD event risk of 10% or higher, a BP target of less than 130/80 mm Hg is recommended.(Level of Evidence: SBP: B-R, DPB: C-EO) " |
| Class IIb |
| "1. For adults with confirmed hypertension, without additional markers of increased CVD risk, a BP target of less than 130/80 mm Hg may be reasonable. (Level of Evidence: SBP: B-NR, DPB: C-EO) " |
Choice of Initial Medication
| Class I |
| "1. For initiation of antihypertensive drug therapy, first-line agents include thiazide diuretics, calcium channel blockers (CCBs), and angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs).(Level of Evidence: A) " |
Choice of Initial Monotherapy Versus Initial Combination Drug Therapy
| Class I |
| "1. Initiation of antihypertensive drug therapy with 2 first-line agents of different classes, either as separate agents or in a fixed-dose combination, is recommended in adults with stage 2 hypertension and an average BP more than 20/10 mm Hg above their BP target.(Level of Evidence: C-EO) " |
| Class IIa |
| "1. Initiation of antihypertensive drug therapy with a single antihypertensive drug is reasonable in adults with stage 1 hypertension and BP goal <130/80 mm Hg with dosage titration and sequential addition of other agents to achieve the BP target. (Level of Evidence: C-EO) " |
Follow-Up After Initiating Antihypertensive Drug Therapy
| Class I |
| "1. Adults initiating a new or adjusted drug regimen for hypertension should have a follow-up evaluation of adherence and response to treatment at monthly intervals until control is achieved.(Level of Evidence: B-R) " |
Monitoring Strategies to Improve Control of Blood Pressure (BP) in Patients on Drug Therapy for High BP
| Class I |
| "1. Follow-up and monitoring after initiation of drug therapy for hypertension control should include systematic strategies to help improve BP, including use of HBPM, team-based care, and telehealth strategies.(Level of Evidence: A) " |
Stable Ischemic Heart Disease (SIHD)
| Class I |
| "1. In adults with SIHD and hypertension, a blood pressure (BP) target of less than 130/80 mm Hg is recommended.(Level of Evidence: SBP: B-R DPB: C-EO) " |
| "2. Adults with SIHD and hypertension (BP ≥130/80 mm Hg) should be treated with medications (e.g., guideline-directed medical therapy (GDMT) beta blockers, ACE inhibitors, or ARBs) for compelling indications (e.g., previous MI, stable angina) as first-line therapy, with the addition of other drugs (e.g., dihydropyridine CCBs, thiazide diuretics, and/or mineralocorticoid receptor antagonists) as needed to further control hypertension.(Level of Evidence: SBP: B-R DPB: C-EO) " |
| "3. In adults with SIHD with angina and persistent uncontrolled hypertension, the addition of dihydropyridine CCBs to GDMT beta blockers is recommended.(Level of Evidence: B-NR) " |
| Class IIa |
| "1. In adults who have had a MI or acute coronary syndrome, it is reasonable to continue GDMT beta blockers beyond 3 years as long-term therapy for hypertension. (Level of Evidence: B-NR) " |
| Class IIb |
| "1. Beta blockers and/or CCBs might be considered to control hypertension in patients with CAD (without HFrEF) who had an MI more than 3 years ago and have angina. (Level of Evidence: C-EO) " |
Heart Failure
| Class I |
| "1. In adults at increased risk of HF, the optimal BP in those with hypertension should be less than 130/80 mm Hg.(Level of Evidence: SBP: B-R DPB: C-EO) " |
Heart Failure With Reduced Ejection Fraction
| Class I |
| "1. Adults with HFrEF and hypertension should be prescribed guideline-directed medical therapy (GDMT) titrated to attain a BP of less than 130/80 mm Hg.(Level of Evidence: C-EO) " |
| Class III: No Benefit |
| "1.Nondihydropyridine CCBs are not recommended in the treatment of hypertension in adults with HFrEF.(Level of Evidence: B-R) " |
Heart Failure With Preserved Ejection Fraction
| Class I |
| "1. In adults with HFpEF who present with symptoms of volume overload, diuretics should be prescribed to control hypertension.(Level of Evidence: C-EO) " |
| "2. Adults with HFpEF and persistent hypertension after management of volume overload should be prescribed ACE inhibitors or ARBs and beta blockers titrated to attain SBP of less than 130 mm Hg.(Level of Evidence: C-LD) " |
Chronic Kidney Disease (CKD)
Recommendations for Treatment of Hypertension in Patients With CKD
| Class I |
| "1. Adults with hypertension and CKD should be treated to a BP goal of less than 130/80 mm Hg.(Level of Evidence: SBP:B-R, DBP:C-EO) " |
| Class IIa |
| "1. In adults with hypertension and CKD (stage 3 or higher or stage 1 or 2 with albuminuria [≥300 mg/d, or ≥300 mg/g albumin-to-creatinine ratio or the equivalent in the first morning void), treatment with an ACE inhibitor is reasonable to slow kidney disease progression. (Level of Evidence: B-R) " |
| Class IIb |
| "1. In adults with hypertension and CKD (stage 3 or higher or stage 1 or 2 with albuminuria [≥300 mg/d, or ≥300 mg/g albumin-to-creatinine ratio in the first morning void), treatment with an ARB may be reasonable if an ACE inhibitor is not tolerated. (Level of Evidence: C-EO) " |
Hypertension After Renal Transplantation
Recommendations for Treatment of Hypertension After Renal Transplantation
| Class IIa |
| "1. After kidney transplantation, it is reasonable to treat patients with hypertension to a BP goal of less than 130/80 mm Hg. (Level of Evidence: SBP:B-NR, DBP:C-EO) " |
| "2. After kidney transplantation, it is reasonable to treat patients with hypertension with a calcium antagonist on the basis of improved GFR and kidney survival. (Level of Evidence: B-R) " |
Acute Intracerebral Haemorrhage (ICH)
| Class IIa |
| "1. In adults with ICH who present with SBP greater than 220 mm Hg, it is reasonable to use continuous intravenous drug infusion and close blood pressure (BP) monitoring to lower systolic blood pressure (SBP).(Level of Evidence: C-EO) " |
| Class III: Harm |
| "1.Immediate lowering of SBP to less than 140 mm Hg in adults with spontaneous ICH who present within 6 hours of the acute event and have an SBP between 150 mm Hg and 220 mm Hg is not of benefit to reduce death or severe disability and can be potentially harmful.(Level of Evidence: A) " |
Acute Ischemic Stroke
| Class I |
| "1. Adults with acute ischemic stroke and elevated blood pressure (BP) who are eligible for treatment with intravenous tissue plasminogen activator should have their BP slowly lowered to less than 185/110 mm Hg before thrombolytic therapy is initiated.(Level of Evidence: B-NR) " |
| "2. In adults with an acute ischemic stroke, BP should be less than 185/110 mm Hg before administration of intravenous tissue plasminogen activator and should be maintained below 180/105 mm Hg for at least the first 24 hours after initiating drug therapy.(Level of Evidence: B-NR) " |
| Class IIa |
| "1. Starting or restarting antihypertensive therapy during hospitalization in patients with BP greater than 140/90 mm Hg who are neurologically stable is safe and reasonable to improve long-term BP control, unless contraindicated.(Level of Evidence: B-NR) " |
| Class IIb |
| "1. In patients with BP of 220/120 mm Hg or higher who did not receive intravenous alteplase or endovascular treatment and have no comorbid conditions requiring acute antihypertensive treatment, the benefit of initiating or reinitiating treatment of hypertension within the first 48 to 72 hours is uncertain. It might be reasonable to lower BP by 15% during the first 24 hours after onset of stroke.(Level of Evidence: C-EO) " |
| Class III: No Benefit |
| "1.In patients with BP less than 220/120 mm Hg who did not receive intravenous thrombolysis or endovascular treatment and do not have a comorbid condition requiring acute antihypertensive treatment, initiating or reinitiating treatment of hypertension within the first 48 to 72 hours after an acute ischemic stroke is not effective to prevent death or dependency.(Level of Evidence: A) " |
Secondary Stroke Prevention
| Class I |
| "1. Adults with previously treated hypertension who experience a stroke or transient ischemic attack (TIA) should be restarted on antihypertensive treatment after the first few days of the index event to reduce the risk of recurrent stroke and other vascular events.(Level of Evidence: A) " |
| "2. For adults who experience a stroke or TIA, treatment with a thiazide diuretic, ACE inhibitor, or ARB, or combination treatment consisting of a thiazide diuretic plus ACE inhibitor, is useful.(Level of Evidence: A) " |
| "3. Adults not previously treated for hypertension who experience a stroke or TIA and have an established BP of 140/90 mm Hg or higher should be prescribed antihypertensive treatment a few days after the index event to reduce the risk of recurrent stroke and other vascular events.(Level of Evidence: B-R) " |
| "4. For adults who experience a stroke or TIA, selection of specific drugs should be individualized on the basis of patient comorbidities and agent pharmacological class.(Level of Evidence: B-R) " |
| Class IIb |
| "1. For adults who experience a stroke or TIA, a BP goal of less than 130/80 mm Hg may be reasonable.(Level of Evidence: B-R) " |
| "2. For adults with a lacunar stroke, a target SBP goal of less than 130 mm Hg may be reasonable.(Level of Evidence: B-R) " |
| "3. In adults previously untreated for hypertension who experience an ischemic stroke or TIA and have a SBP less than 140 mm Hg and a DBP less than 90 mm Hg, the usefulness of initiating antihypertensive treatment is not well established.(Level of Evidence: C-LD) " |
Peripheral Arterial Disease (PAD)
| Class I |
| "1. Adults with hypertension and PAD should be treated similarly to patients with hypertension without PAD.(Level of Evidence: B-NR) " |
Diabetes Mellitus
| Class I |
| "1. In adults with DM and hypertension, antihypertensive drug treatment should be initiated at a BP of 130/80 mm Hg or higher with a treatment goal of less than 130/80 mm Hg.(Level of Evidence: SBP:B-R, DBP:C-EO) " |
| "2. In adults with DM and hypertension, all first-line classes of antihypertensive agents (i.e., diuretics, ACE inhibitors, ARBs, and CCBs) are useful and effective.(Level of Evidence: A) " |
| Class IIb |
| "1. In adults with DM and hypertension, ACE inhibitors or ARBs may be considered in the presence of albuminuria.(Level of Evidence: B-NR) " |
Atrial Fibrillation (AF)
| Class IIa |
| "1. Treatment of hypertension with an ARB can be useful for prevention of recurrence of AF.(Level of Evidence: B-R) " |
Valvular Heart Disease (VHD)
| Class I |
| "1. In adults with asymptomatic aortic stenosis, hypertension should be treated with pharmacotherapy, starting at a low dose and gradually titrating upward as needed.(Level of Evidence: B-NR) " |
| Class IIa |
| "1. In patients with chronic aortic insufficiency, treatment of systolic hypertension with agents that do not slow the heart rate (i.e., avoid beta blockers) is reasonable.(Level of Evidence: C-LD) " |
Aortic Disease
| Class I |
| "1. Beta blockers are recommended as the preferred antihypertensive agents in patients with hypertension and thoracic aortic disease.(Level of Evidence: C-EO) " |
Racial and Ethnic Differences in Treatment
| Class I |
| "1. In black adults with hypertension but without heart failure (HF) or chronic kidney disease (CKD), including those with diabetes mellitus (DM), initial antihypertensive treatment should include a thiazide-type diuretic or calcium channel blockers (CCB).(Level of Evidence: B-R) " |
| "2. Two or more antihypertensive medications are recommended to achieve a blood pressure target of less than 130/80 mm Hg in most adults with hypertension, especially in black adults with hypertension.(Level of Evidence: C-LD) " |
Pregnancy
| Class I |
| "1. Women with hypertension who become pregnant, or are planning to become pregnant, should be transitioned to methyldopa, nifedipine, and/or labetalol during pregnancy .(Level of Evidence: C-LD) " |
| Class III: Harm |
| "1.Women with hypertension who become pregnant should not be treated with ACE inhibitors, ARBs, or direct renin inhibitors.(Level of Evidence: C-LD) " |
Older Persons
| Class I |
| "1. Treatment of hypertension with a SBP treatment goal of less than 130 mm Hg is recommended for noninstitutionalized ambulatory community dwelling adults (≥65 years of age) with an average SBP of 130 mm Hg or higher.(Level of Evidence: A) " |
| Class IIa |
| "1. For older adults (≥65 years of age) with hypertension and a high burden of comorbidity and limited life expectancy, clinical judgment, patient preference, and a team-based approach to assess risk/benefit is reasonable for decisions regarding intensity of BP lowering and choice of antihypertensive drugs.(Level of Evidence: C-EO) " |
Hypertensive Crises—Emergencies and Urgencies
| Class I |
| "1. In adults with a hypertensive emergency, admission to an intensive care unit is recommended for continuous monitoring of BP and target organ damage and for parenteral administration of an appropriate agent.(Level of Evidence: B-NR) " |
| "2. For adults with a compelling condition (i.e., aortic dissection, severe preeclampsia or eclampsia, or pheochromocytoma crisis), SBP should be reduced to less than 140 mm Hg during the first hour and to less than 120 mm Hg in aortic dissection.(Level of Evidence: C-EO) " |
| "3. For adults without a compelling condition, SBP should be reduced by no more than 25% within the first hour; then, if stable, to 160/100 mm Hg within the next 2 to 6 hours; and then cautiously to normal during the following 24 to 48 hours.(Level of Evidence: C-EO) " |
Cognitive Decline and Dementia
| Class IIa |
| "1. In adults with hypertension, BP lowering is reasonable to prevent cognitive decline and dementia.(Level of Evidence: B-R) " |
Patients Undergoing Surgical Procedures
| Class I |
| "1. In patients with hypertension undergoing major surgery who have been on beta blockers chronically, beta blockers should be continued.(Level of Evidence: B-NR) " |
| Class IIa |
| "1. In patients with hypertension undergoing planned elective major surgery, it is reasonable to continue medical therapy for hypertension until surgery.(Level of Evidence: C-EO) " |
| Class IIb |
| "1. In patients with hypertension undergoing major surgery, discontinuation of ACE inhibitors or ARBs perioperatively may be considered.(Level of Evidence: B-NR) " |
| "2. In patients with planned elective major surgery and SBP of 180 mm Hg or higher or DBP of 110 mm Hg or higher, deferring surgery may be considered.(Level of Evidence: C-LD) " |
| Class III: Harm |
| "1.For patients undergoing surgery, abrupt preoperative discontinuation of beta blockers or clonidine is potentially harmful.(Level of Evidence: B-NR) " |
| "2.Beta blockers should not be started on the day of surgery in beta blocker– naïve patients.(Level of Evidence: B-NR) " |
| Intraoperative |
| Class I |
| "1. Patients with intraoperative hypertension should be managed with intravenous medications until such time as oral medications can be resumed.(Level of Evidence: C-EO) " |
Antihypertensive Medication Adherence Strategies
| Class I |
| "1. In adults with hypertension, dosing of antihypertensive medication once daily rather than multiple times daily is beneficial to improve adherence.(Level of Evidence: B-R) " |
| Class IIa |
| "1. Use of combination pills rather than free individual components can be useful to improve adherence to antihypertensive therapy.(Level of Evidence: B-NR) " |
2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults JNC 8 (DO NOT EDIT)[77]
Recommendations for the Management of Hypertension
| "1. In the general population aged ≥60 years, initiate pharmacologic treatment to lower blood pressure (BP) at systolic blood pressure (SBP) ≥150 mm Hg or diastolic blood pressure (DBP) ≥90 mm Hg and treat to a goal SBP <150 mm Hg and goal DBP <90 mm Hg. (Strong Recommendation: Grade A)" |
| "2. In the general population for ages 30-59 years, initiate pharmacologic treatment to lower BP at DBP ≥90 mm Hg and treat to a goal DBP <90 mm Hg. (Strong Recommendation: Grade A)" |
| "1. In the general population aged ≥60 years, if pharmacologic treatment for high BP results in lower achieved SBP (eg, <140 mm Hg) and treatment is well tolerated and without adverse effects on health or quality of life, treatment does not need to be adjusted. (Expert Opinion: Grade E)" |
| "2. In the general population for ages 18-29 years, initiate pharmacologic treatment to lower BP at DBP ≥90 mm Hg and treat to a goal DBP <90 mm Hg. (Expert Opinion: Grade E)" |
| "3. In the general population <60 years, initiate pharmacologic treatment to lower BP at SBP ≥140 mm Hg and treat to a goal SBP <140 mm Hg. (Expert Opinion: Grade E)" |
| "4. In the population aged ≥18 years with chronic kidney disease (CKD), initiate pharmacologic treatment to lower BP at SBP ≥140 mm Hg or DBP ≥90 mm Hg and treat to goal SBP <140 mm Hg and goal DBP <90 mm Hg. (Expert Opinion: Grade E)" |
| "5. In the population aged ≥18 years with diabetes, initiate pharmacologic treatment to lower BP at SBP ≥140 mm Hg or DBP ≥90 mm Hg and treat to a goal SBP <140 mm Hg and goal DBP <90 mm Hg. (Expert Opinion: Grade E)" |
| "6. In the general non-black population, including those with diabetes, initial antihypertensive treatment should include a thiazide-type diuretic, calcium channel blocker (CCB), angiotensin-converting enzyme inhibitor (ACEI), or angiotensin receptor blocker (ARB). (Moderate Recommendation: Grade B)" |
| "7. In the general black population, initial antihypertensive treatment should include a thiazide-type diuretic or CCB. (Moderate Recommendation: Grade B)" |
| "8. In the general black population with diabetes, initial antihypertensive treatment should include a thiazide-type diuretic or CCB. (Weak Recommendation: Grade C)" |
| "9. In the population aged ≥18 years with CKD, initial (or add-on) antihypertensive treatment should include an ACEI or ARB to improve kidney outcomes. This applies to all CKD patients with hypertension regardless of race or diabetes status. (Moderate Recommendation: Grade B)" |
| "10. The main objective of hypertension treatment is to attain and maintain goal BP. If goal BP is not reached within a month of treatment, increase the dose of the initial drug or add a second drug from one of the classes in recommendation 6 (thiazide-type diuretic, CCB, ACEI, or ARB). The clinician should continue to assess BP and adjust the treatment regimen until goal BP is reached. If goal BP cannot be reached with 2 drugs, add and titrate a third drug from the list provided. Do not use an ACEI and an ARB together in the same patient. If goal BP cannot be reached using only the drugs in recommendation 6 because of a contraindication or the need to use more than 3 drugs to reach goal BP, antihypertensive drugs from other classes can be used. Referral to a hypertension specialist may be indicated for patients in whom goal BP cannot be attained using the above strategy or for the management of complicated patients for whom additional clinical consultation is needed. (Expert Opinion: Grade E)" |
2013 ESH/ESC Guidelines For The Management of Arterial Hypertension (DO NOT EDIT)[78]
Summary of Recommendations on Initiation of Antihypertensive Drug Treatment (DO NOT EDIT)[78]
| Class I |
| "1. Prompt initiation of drug treatment is recommended in individuals with grade 2 and 3 hypertension with any level of CV risk, a few weeks after or simultaneously with initiation of lifestyle changes. (Level of Evidence: A)" |
| "3. In elderly hypertensive patients drug treatment is recommended when SBP is ≥160 mmHg.(Level of Evidence: A)" |
| "2. Lowering BP with drugs is also recommended when total CV risk is high because of OD, diabetes, CVD or CKD, even when hypertension is in the grade 1 range.(Level of Evidence: B)" |
| Class IIa |
| "1. Initiation of antihypertensive drug treatment should also be considered in grade 1 hypertensive patients at low to moderate risk, when BP is within this range at several repeated visits or elevated by ambulatory BP criteria, and remains within this range despite a reasonable period of time with lifestyle measures. (Level of Evidence: B)" |
| Class IIb |
| "1. Antihypertensive drug treatment may also be considered in the elderly (at least when younger than 80 years) when SBP is in the 140–159 mmHg range, provided that antihypertensive treatment is well tolerated.(Level of Evidence: C)" |
| Class III |
| "1. Unless the necessary evidence is obtained it is not recommended to initiate antihypertensive drug therapy at high normal BP. (Level of Evidence: A)" |
| "2. Lack of evidence does also not allow recommending to initiate antihypertensive drug therapy in young individuals with isolated elevation of brachial SBP, but these individuals should be followed closely with lifestyle recommendations. (Level of Evidence: A)" |
Summary of Recommendations on Blood pressure Goals in Hypertensive Patients(DO NOT EDIT)[78]
| Class I |
| "1. A SBP goal <140 mmHg: a) is recommended in patients at low–moderate CV risk. (Level of Evidence: B) b) is recommended in patients with diabetes. (Level of Evidence: A)" |
| "2. In elderly hypertensives less than 80 years old with SBP ≥160 mmHg there is solid evidence to recommend reducing SBP to between 150 and 140 mmHg.(Level of Evidence: A)" |
| "3. In individuals older than 80 years and with initial SBP ≥160 mmHg, it is recommended to reduce SBP to between 150 and 140 mmHg provided they are in good physical and mental conditions.(Level of Evidence: B)" |
| "3. A DBP target of <90 mmHg is always recommended, except in patients with diabetes, in whom values <85 mmHg are recommended. It should nevertheless be considered that DBP values between 80 and 85 mmHg are safe and well tolerated.(Level of Evidence: A)" |
| Class IIa |
| "1. A SBP goal <140 mmHg: a) should be considered in patients with previous stroke or TIA. (Level of Evidence: B) b) should be considered in patients with CHD. (Level of Evidence: B) c) should be considered in patients with diabetic or non-diabetic CKD. (Level of Evidence: B)" |
| Class IIb |
| "1. In fit elderly patients less than 80 years old SBP values <140 mmHg may be considered, whereas in the fragile elderly population SBP goals should be adapted to individual tolerability.(Level of Evidence: C)" |
Summary of Recommendations on Treatment Strategies and Choice of Drugs (DO NOT EDIT)[78]
| Class I |
| "1. Diuretics (thiazides, chlorthalidone and indapamide), beta-blockers, calcium antagonists, ACE inhibitors, and angiotensin receptor blockers are all suitable and recommended for the initiation and maintenance of antihypertensive treatment, either as monotherapy or in some combinations with each other.(Level of Evidence: A)" |
| Class IIa |
| "1. Some agents should be considered as the preferential choice in specific conditions because used in trials in those conditions or because of greater effectiveness in specific types of OD. (Level of Evidence: C)" |
| "2. Other drug combinations should be considered and probably are beneficial in proportion to the extent of BP reduction. However, combinations that have been successfully used in trials may be preferable. (Level of Evidence: C)" |
| Class IIb |
| "1. Initiation of antihypertensive therapy with a two-drug combination may be considered in patients with markedly high baseline BP or at high CV risk.(Level of Evidence: C)" |
| "1. Combinations of two antihypertensive drugs at fixed doses in a single tablet may be recommended and favoured, because reducing the number of daily pills improves adherence, which is low in patients with hypertension.(Level of Evidence: B)" |
| Class III |
| "1. The combination of two antagonists of the RAS is not recommended and should be discouraged. (Level of Evidence: A)" |
References
- ↑ Blood Pressure Lowering Treatment Trialists' Collaboration (2014). "Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data". Lancet. 384 (9943): 591–598. doi:10.1016/S0140-6736(14)61212-5. PMID 25131978. Review in: Ann Intern Med. 2014 Dec 16;161(12):JC5 Review in: Evid Based Med. 2015 Feb;20(1):21
- ↑ Wilt TJ, Kansagara D, Qaseem A, Clinical Guidelines Committee of the American College of Physicians (2018). "Hypertension Limbo: Balancing Benefits, Harms, and Patient Preferences Before We Lower the Bar on Blood Pressure". Ann Intern Med. 168 (5): 369–370. doi:10.7326/M17-3293. PMID 29357397.
- ↑ Saiz LC, Gorricho J, Garjón J, Celaya MC, Erviti J, Leache L (2018). "Blood pressure targets for the treatment of people with hypertension and cardiovascular disease". Cochrane Database Syst Rev. 7: CD010315. doi:10.1002/14651858.CD010315.pub3. PMID 30027631.
- ↑ Garrison SR, Kolber MR, Korownyk CS, McCracken RK, Heran BS, Allan GM (2017). "Blood pressure targets for hypertension in older adults". Cochrane Database Syst Rev. 8: CD011575. doi:10.1002/14651858.CD011575.pub2. PMID 28787537.
- ↑ 5.0 5.1 Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C; et al. (2017). "2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines". Hypertension. doi:10.1161/HYP.0000000000000065. PMID 29133356.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C; et al. (2017). "2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines". Hypertension. doi:10.1161/HYP.0000000000000066. PMID 29133354.
- ↑ Go AS (2018). "Impact of SPRINT-Based Blood Pressure Levels on Clinical Outcomes in a Large, Community-Based Population: The Kaiser Permanente Experience". Circulation. doi:10.1161/circ.136.suppl_1.14468.
- ↑ 8.0 8.1 8.2 8.3 Qaseem A, Wilt TJ, Rich R, Humphrey LL, Frost J, Forciea MA; et al. (2017). "Pharmacologic Treatment of Hypertension in Adults Aged 60 Years or Older to Higher Versus Lower Blood Pressure Targets: A Clinical Practice Guideline From the American College of Physicians and the American Academy of Family Physicians". Ann Intern Med. 166 (6): 430–437. doi:10.7326/M16-1785. PMID 28135725. Review in: Ann Intern Med. 2017 Apr 18;166(8):JC38
- ↑ 9.0 9.1 9.2 9.3 James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J; et al. (2014). "2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8)". JAMA. 311 (5): 507–20. doi:10.1001/jama.2013.284427. PMID 24352797.
- ↑ SPRINT Research Group. Wright JT, Williamson JD, Whelton PK, Snyder JK, Sink KM; et al. (2015). "A Randomized Trial of Intensive versus Standard Blood-Pressure Control". N Engl J Med. 373 (22): 2103–16. doi:10.1056/NEJMoa1511939. PMC 4689591. PMID 26551272.
- ↑ Yusuf S, Lonn E, Pais P, Bosch J, López-Jaramillo P, Zhu J; et al. (2016). "Blood-Pressure and Cholesterol Lowering in Persons without Cardiovascular Disease". N Engl J Med. 374 (21): 2032–43. doi:10.1056/NEJMoa1600177. PMID 27039945.
- ↑ ACCORD Study Group. Cushman WC, Evans GW, Byington RP, Goff DC, Grimm RH; et al. (2010). "Effects of intensive blood-pressure control in type 2 diabetes mellitus". N Engl J Med. 362 (17): 1575–85. doi:10.1056/NEJMoa1001286. PMC 4123215. PMID 20228401. Review in: Evid Based Med. 2010 Oct;15(5):142-3 Review in: Ann Intern Med. 2010 Jul 20;153(2):JC1-4, JC1-5
- ↑ Bangalore S, Messerli FH, Wun CC, Zuckerman AL, DeMicco D, Kostis JB; et al. (2010). "J-curve revisited: An analysis of blood pressure and cardiovascular events in the Treating to New Targets (TNT) Trial". Eur Heart J. 31 (23): 2897–908. doi:10.1093/eurheartj/ehq328. PMID 20846991.
- ↑ 14.0 14.1 "Summary of revisions for the 2013 clinical practice recommendations". Diabetes Care. 36 Suppl 1: S3. 2013. doi:10.2337/dc13-S003. PMC 3537268. PMID 23264423.
- ↑ 15.0 15.1 Mancia G, Fagard R, Narkiewicz K, Redán J, Zanchetti A, Böhm M; et al. (2013). "2013 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC): ESH/ESC Task Force for the Management of Arterial Hypertension". J Hypertens. 31 (10): 1925–38. doi:10.1097/HJH.0b013e328364ca4c. PMID 24107724.
- ↑ Weiss J, Freeman M, Low A, Fu R, Kerfoot A, Paynter R; et al. (2017). "Benefits and Harms of Intensive Blood Pressure Treatment in Adults Aged 60 Years or Older: A Systematic Review and Meta-analysis". Ann Intern Med. 166 (6): 419–429. doi:10.7326/M16-1754. PMID 28114673.
- ↑ 17.0 17.1 17.2 Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL; et al. (2003). "Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure". Hypertension. 42 (6): 1206–52. doi:10.1161/01.HYP.0000107251.49515.c2. PMID 14656957.
- ↑ 18.0 18.1 18.2 18.3 18.4 18.5 18.6 18.7 18.8 Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M; et al. (2013). "2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)". J Hypertens. 31 (7): 1281–357. doi:10.1097/01.hjh.0000431740.32696.cc. PMID 23817082.
- ↑ Laragh JH (1973). "Vasoconstriction-volume analysis for understanding and treating hypertension: the use of renin and aldosterone profiles". Am J Med. 55 (3): 261–74. PMID 4355699.
- ↑ Laragh JH, Baer L, Brunner HR, Buhler FR, Sealey JE, Vaughan ED (1972). "Renin, angiotensin and aldosterone system in pathogenesis and management of hypertensive vascular disease". Am J Med. 52 (5): 633–52. PMID 4337477.
- ↑ 21.0 21.1 Materson BJ, Reda DJ (1994). "Correction: single-drug therapy for hypertension in men". N. Engl. J. Med. 330 (23): 1689. PMID 8177286.
- ↑ 22.0 22.1 Preston RA, Materson BJ, Reda DJ; et al. (1998). "Age-race subgroup compared with renin profile as predictors of blood pressure response to antihypertensive therapy. Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents". JAMA. 280 (13): 1168–72. PMID 9777817.
- ↑ Lauffenburger JC, Landon JE, Fischer MA (2017). "Effect of Combination Therapy on Adherence Among US Patients Initiating Therapy for Hypertension: a Cohort Study". J Gen Intern Med. 32 (6): 619–625. doi:10.1007/s11606-016-3972-z. PMC 5442007. PMID 28050754.
- ↑ 24.0 24.1 Verma AA, Khuu W, Tadrous M, Gomes T, Mamdani MM (2018). "Fixed-dose combination antihypertensive medications, adherence, and clinical outcomes: A population-based retrospective cohort study". PLoS Med. 15 (6): e1002584. doi:10.1371/journal.pmed.1002584. PMC 5995349. PMID 29889841.
- ↑ Hunt SA, Baker DW, Chin MH, Cinquegrani MP, Feldman AM, Francis GS et al. (2001)ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to revise the 1995 Guidelines for the Evaluation and Management of Heart Failure). J Am Coll Cardiol 38 (7):2101-13. PMID:11738322
- ↑ Tepper D (1999) Frontiers in congestive heart failure: Effect of Metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Congest Heart Fail 5 (4):184-185. PMID: 12189311
- ↑ Packer M, Coats AJ, Fowler MB, Katus HA, Krum H, Mohacsi P et al. (2001)Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med 344 (22):1651-8. DOI:10.1056/NEJM200105313442201 PMID:11386263
- ↑ (1994) A randomized trial of beta-blockade in heart failure. The Cardiac Insufficiency Bisoprolol Study (CIBIS). CIBIS Investigators and Committees. Circulation 90 (4):1765-73. PMID: 7923660
- ↑ (1991) Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. The SOLVD Investigators. N Engl J Med 325 (5):293-302.DOI:10.1056/NEJM199108013250501 PMID: 2057034
- ↑ (1993) Effect of ramipril on mortality and morbidity of survivors of acute myocardial infarction with clinical evidence of heart failure. The Acute Infarction Ramipril Efficacy (AIRE) Study Investigators. Lancet 342 (8875):821-8. PMID: 8104270
- ↑ Køber L, Torp-Pedersen C, Carlsen JE, Bagger H, Eliasen P, Lyngborg K et al. (1995) A clinical trial of the angiotensin-converting-enzyme inhibitor trandolapril in patients with left ventricular dysfunction after myocardial infarction. Trandolapril Cardiac Evaluation (TRACE) Study Group. N Engl J Med 333 (25):1670-6.DOI:10.1056/NEJM199512213332503 PMID: 7477219
- ↑ Cohn JN, Tognoni G, Valsartan Heart Failure Trial Investigators (2001) A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med345 (23):1667-75. DOI:10.1056/NEJMoa010713 PMID: 11759645
- ↑ Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A et al. (1999) The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med 341 (10):709-17. DOI:10.1056/NEJM199909023411001PMID: 10471456
- ↑ Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JS et al. (2002)ACC/AHA 2002 guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction--summary article: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee on the Management of Patients With Unstable Angina). J Am Coll Cardiol 40 (7):1366-74. PMID: 12383588
- ↑ (1982) A randomized trial of propranolol in patients with acute myocardial infarction. I. Mortality results.JAMA 247 (12):1707-14. PMID: 7038157
- ↑ Hager WD, Davis BR, Riba A, Moye LA, Wun CC, Rouleau JL et al. (1998) Absence of a deleterious effect of calcium channel blockers in patients with left ventricular dysfunction after myocardial infarction: The SAVE Study Experience. SAVE Investigators. Survival and Ventricular Enlargement. Am Heart J 135 (3):406-13. PMID: 9506325
- ↑ Dargie HJ (2001) Effect of carvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: the CAPRICORN randomised trial. Lancet 357 (9266):1385-90. PMID:11356434
- ↑ Pitt B, Remme W, Zannad F, Neaton J, Martinez F, Roniker B et al. (2003)Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 348 (14):1309-21. [1] PMID: 12668699
- ↑ 39.0 39.1 ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (2002) Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 288 (23):2981-97. PMID: 12479763
- ↑ Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G (2000) Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med 342 (3):145-53. [2] PMID: 10639539
- ↑ Wing LM, Reid CM, Ryan P, Beilin LJ, Brown MA, Jennings GL et al. (2003) A comparison of outcomes with angiotensin-converting--enzyme inhibitors and diuretics for hypertension in the elderly. N Engl J Med 348 (7):583-92.DOI:10.1056/NEJMoa021716 PMID: 12584366
- ↑ Dahlöf B, Devereux RB, Kjeldsen SE, Julius S, Beevers G, de Faire U et al. (2002) Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet 359 (9311):995-1003. DOI:10.1016/S0140-6736(02)08089-3 PMID: 11937178
- ↑ Black HR, Elliott WJ, Grandits G, Grambsch P, Lucente T, White WB et al. (2003) Principal results of the Controlled Onset Verapamil Investigation of Cardiovascular End Points (CONVINCE) trial. JAMA 289 (16):2073-82.DOI:10.1001/jama.289.16.2073 PMID: 12709465
- ↑ Arauz-Pacheco C, Parrott MA, Raskin P, American Diabetes Association (2003)Treatment of hypertension in adults with diabetes.Diabetes Care 26 Suppl 1 ():S80-2. PMID: 12502624
- ↑ 45.0 45.1 National Kidney Foundation (2002)K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 39 (2 Suppl 1):S1-266. PMID: 11904577
- ↑ (1998) Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. UK Prospective Diabetes Study Group.BMJ 317 (7160):713-20. PMID: 9732338
- ↑ Lewis EJ, Hunsicker LG, Bain RP, Rohde RD (1993) The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. N Engl J Med 329 (20):1456-62. DOI:10.1056/NEJM199311113292004 PMID: [3]
- ↑ Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH et al. (2001)Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 345 (12):861-9. DOI:10.1056/NEJMoa011161PMID: 11565518
- ↑ Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA, Lewis JB et al. (2001) Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med 345 (12):851-60. [4] PMID: 11565517
- ↑ (1997)Randomised placebo-controlled trial of effect of ramipril on decline in glomerular filtration rate and risk of terminal renal failure in proteinuric, non-diabetic nephropathy. The GISEN Group (Gruppo Italiano di Studi Epidemiologici in Nefrologia) Lancet 349 (9069):1857-63. PMID: 9217756
- ↑ Wright JT, Agodoa L, Contreras G, Greene T, Douglas JG, Lash J et al. (2002) Successful blood pressure control in the African American Study of Kidney Disease and Hypertension. Arch Intern Med 162 (14):1636-43. PMID: 12123409
- ↑ PROGRESS Collaborative Group (2001) Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet 358 (9287):1033-41. DOI:10.1016/S0140-6736(01)06178-5 PMID:11589932
- ↑ 53.0 53.1 Tucker KL, Sheppard JP, Stevens R, Bosworth HB, Bove A, Bray EP; et al. (2017). "Self-monitoring of blood pressure in hypertension: A systematic review and individual patient data meta-analysis". PLoS Med. 14 (9): e1002389. doi:10.1371/journal.pmed.1002389. PMC 5604965. PMID 28926573. Review in: Ann Intern Med. 2018 Feb 20;168(4):JC16
- ↑ McManus RJ, Mant J, Franssen M, Nickless A, Schwartz C, Hodgkinson J; et al. (2018). "Efficacy of self-monitored blood pressure, with or without telemonitoring, for titration of antihypertensive medication (TASMINH4): an unmasked randomised controlled trial". Lancet. 391 (10124): 949–959. doi:10.1016/S0140-6736(18)30309-X. PMC 5854463. PMID 29499873.
- ↑ 55.0 55.1 Carter BL, Rogers M, Daly J, Zheng S, James PA (2009). "The potency of team-based care interventions for hypertension: a meta-analysis". Arch Intern Med. 169 (19): 1748–55. doi:10.1001/archinternmed.2009.316. PMC 2882164. PMID 19858431. Review in: Evid Based Nurs. 2010 Apr;13(2):47-8
- ↑ 56.0 56.1 Jaffe MG, Lee GA, Young JD, Sidney S, Go AS (2013). "Improved blood pressure control associated with a large-scale hypertension program". JAMA. 310 (7): 699–705. doi:10.1001/jama.2013.108769. PMC 4270203. PMID 23989679.
- ↑ Hebert PL, Sisk JE, Tuzzio L, Casabianca JM, Pogue VA, Wang JJ; et al. (2012). "Nurse-led disease management for hypertension control in a diverse urban community: a randomized trial". J Gen Intern Med. 27 (6): 630–9. doi:10.1007/s11606-011-1924-1. PMC 3358388. PMID 22143452.
- ↑ 58.0 58.1 Proia KK, Thota AB, Njie GJ, Finnie RK, Hopkins DP, Mukhtar Q; et al. (2014). "Team-based care and improved blood pressure control: a community guide systematic review". Am J Prev Med. 47 (1): 86–99. doi:10.1016/j.amepre.2014.03.004. PMC 4672378. PMID 24933494.
- ↑ Fortuna RJ, Nagel AK, Rose E, McCann R, Teeters JC, Quigley DD; et al. (2015). "Effectiveness of a multidisciplinary intervention to improve hypertension control in an urban underserved practice". J Am Soc Hypertens. 9 (12): 966–74. doi:10.1016/j.jash.2015.10.004. PMID 26687551.
- ↑ Yi SS, Tabaei BP, Angell SY, Rapin A, Buck MD, Pagano WG; et al. (2015). "Self-blood pressure monitoring in an urban, ethnically diverse population: a randomized clinical trial utilizing the electronic health record". Circ Cardiovasc Qual Outcomes. 8 (2): 138–45. doi:10.1161/CIRCOUTCOMES.114.000950. PMC 4366280. PMID 25737487.
- ↑ Uhlig K, Patel K, Ip S, Kitsios GD, Balk EM (2013). "Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis". Ann Intern Med. 159 (3): 185–94. doi:10.7326/0003-4819-159-3-201308060-00008. PMID 23922064.
- ↑ "Executive summary: Standards of medical care in diabetes--2013". Diabetes Care. 36 Suppl 1: S4–10. 2013. doi:10.2337/dc13-S004. PMC 3537272. PMID 23264424.
- ↑ ONTARGET Investigators. Yusuf S, Teo KK, Pogue J, Dyal L, Copland I; et al. (2008). "Telmisartan, ramipril, or both in patients at high risk for vascular events". N Engl J Med. 358 (15): 1547–59. doi:10.1056/NEJMoa0801317. PMID 18378520. Review in: J Fam Pract. 2009 Jan;58(1):24-7 Review in: Evid Based Med. 2008 Oct;13(5):147
- ↑ 64.0 64.1 64.2 Rodeheffer RJ (2011). "Hypertension and heart failure: the ALLHAT imperative". Circulation. 124 (17): 1803–5. doi:10.1161/CIRCULATIONAHA.111.059303. PMID 22025634.
- ↑ Weinberger MH (1985). "Blood pressure and metabolic responses to hydrochlorothiazide, captopril, and the combination in black and white mild-to-moderate hypertensive patients". J Cardiovasc Pharmacol. 7 Suppl 1: S52–5. PMID 2580177.
- ↑ Sica DA (2002). "Cardiovascular morbidity and mortality in patients with diabetes in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol". Curr Hypertens Rep. 4 (4): 321–3. PMID 12117460.
- ↑ 67.0 67.1 67.2 67.3 67.4 67.5 67.6 67.7 Cuddy ML (2005). "Treatment of hypertension: guidelines from JNC 7 (the seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure 1)". J Pract Nurs. 55 (4): 17–21, quiz 22-3. PMID 16512265.
- ↑ Schrier RW, Estacio RO, Esler A, Mehler P (2002). "Effects of aggressive blood pressure control in normotensive type 2 diabetic patients on albuminuria, retinopathy and strokes". Kidney Int. 61 (3): 1086–97. doi:10.1046/j.1523-1755.2002.00213.x. PMID 11849464.
- ↑ Wright JT, Bakris G, Greene T, Agodoa LY, Appel LJ, Charleston J; et al. (2002). "Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial". JAMA. 288 (19): 2421–31. PMID 12435255.
- ↑ Klahr S, Levey AS, Beck GJ, Caggiula AW, Hunsicker L, Kusek JW; et al. (1994). "The effects of dietary protein restriction and blood-pressure control on the progression of chronic renal disease. Modification of Diet in Renal Disease Study Group". N Engl J Med. 330 (13): 877–84. doi:10.1056/NEJM199403313301301. PMID 8114857.
- ↑ Ruggenenti P, Perna A, Loriga G, Ganeva M, Ene-Iordache B, Turturro M; et al. (2005). "Blood-pressure control for renoprotection in patients with non-diabetic chronic renal disease (REIN-2): multicentre, randomised controlled trial". Lancet. 365 (9463): 939–46. doi:10.1016/S0140-6736(05)71082-5. PMID 15766995.
- ↑ Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D; et al. (2001). "Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group". N Engl J Med. 344 (1): 3–10. doi:10.1056/NEJM200101043440101. PMID 11136953.
- ↑ Appel LJ, Espeland MA, Easter L, Wilson AC, Folmar S, Lacy CR (2001). "Effects of reduced sodium intake on hypertension control in older individuals: results from the Trial of Nonpharmacologic Interventions in the Elderly (TONE)". Arch Intern Med. 161 (5): 685–93. PMID 11231700.
- ↑ Bulpitt CJ, Beckett NS, Peters R, Leonetti G, Gergova V, Fagard R; et al. (2012). "Blood pressure control in the Hypertension in the Very Elderly Trial (HYVET)". J Hum Hypertens. 26 (3): 157–63. doi:10.1038/jhh.2011.10. PMID 21390056.
- ↑ 75.0 75.1 Fontil V, Gupta R, Moise N, Chen E, Guzman D, McCulloch CE; et al. (2018). "Adapting and Evaluating a Health System Intervention From Kaiser Permanente to Improve Hypertension Management and Control in a Large Network of Safety-Net Clinics". Circ Cardiovasc Qual Outcomes. 11 (7): e004386. doi:10.1161/CIRCOUTCOMES.117.004386. PMC 6071320. PMID 30002140.
- ↑ ACOG Committee on Practice Bulletins--Obstetrics (2002). "ACOG practice bulletin. Diagnosis and management of preeclampsia and eclampsia. Number 33, January 2002". Obstet Gynecol. 99 (1): 159–67. PMID 16175681.
- ↑ James, Paul A.; Oparil, Suzanne; Carter, Barry L.; Cushman, William C.; Dennison-Himmelfarb, Cheryl; Handler, Joel; Lackland, Daniel T.; LeFevre, Michael L.; MacKenzie, Thomas D.; Ogedegbe, Olugbenga; Smith, Sidney C.; Svetkey, Laura P.; Taler, Sandra J.; Townsend, Raymond R.; Wright, Jackson T.; Narva, Andrew S.; Ortiz, Eduardo (2013). "2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults". JAMA. doi:10.1001/jama.2013.284427. ISSN 0098-7484.
- ↑ 78.0 78.1 78.2 78.3 Authors/Task Force Members. Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A; et al. (2013). "2013 ESH/ESC Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)". Eur Heart J. 34 (28): 2159–219. doi:10.1093/eurheartj/eht151. PMID 23771844.