Chronic hypertension medical therapy
|
Hypertension Main page |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Lakshmi Gopalakrishnan, M.B.B.S. [2]; Assistant Editor-In-Chief: Taylor Palmieri
Overview
There are many classes of medications for treating hypertension, together called antihypertensives, which by varying means act by lowering blood pressure. Evidence suggests that reduction of the blood pressure by 5-6 mmHg can decrease the risk of stroke by 40%, of coronary heart disease by 15-20%, and reduces the likelihood of dementia, heart failure, and mortality from vascular disease.
Medical Therapy
Goals of Therapy
In addition to alleviating symptoms of hypertension, such as headache and blurry vision, the ultimate long term goals of the management of hypertension are to reduce cardiovascular risk, prevent cardiovascular events, and reverse or ameliorate target organ damage. According to “Blood Pressure Lowering Treatment Trialists’ Collaboration” in 2000, lowering blood pressure decreases the incidence of stroke by an average of 30%, MI by an average of 20%, major cardiovascular events by an average of 21%, and heart failure by an average of more than 50%.[1]
JNC 7 has established the goal blood pressure to be < 140/90 mmHg[2], with major focus on reduction of systolic blood pressure due to its role in the consequential reduction of diastolic blood pressure. In special populations such as those with diabetes mellitus or renal disease, the blood pressure goal is < 130/80 mmHg.[3][4]
Approach to Medical Therapy
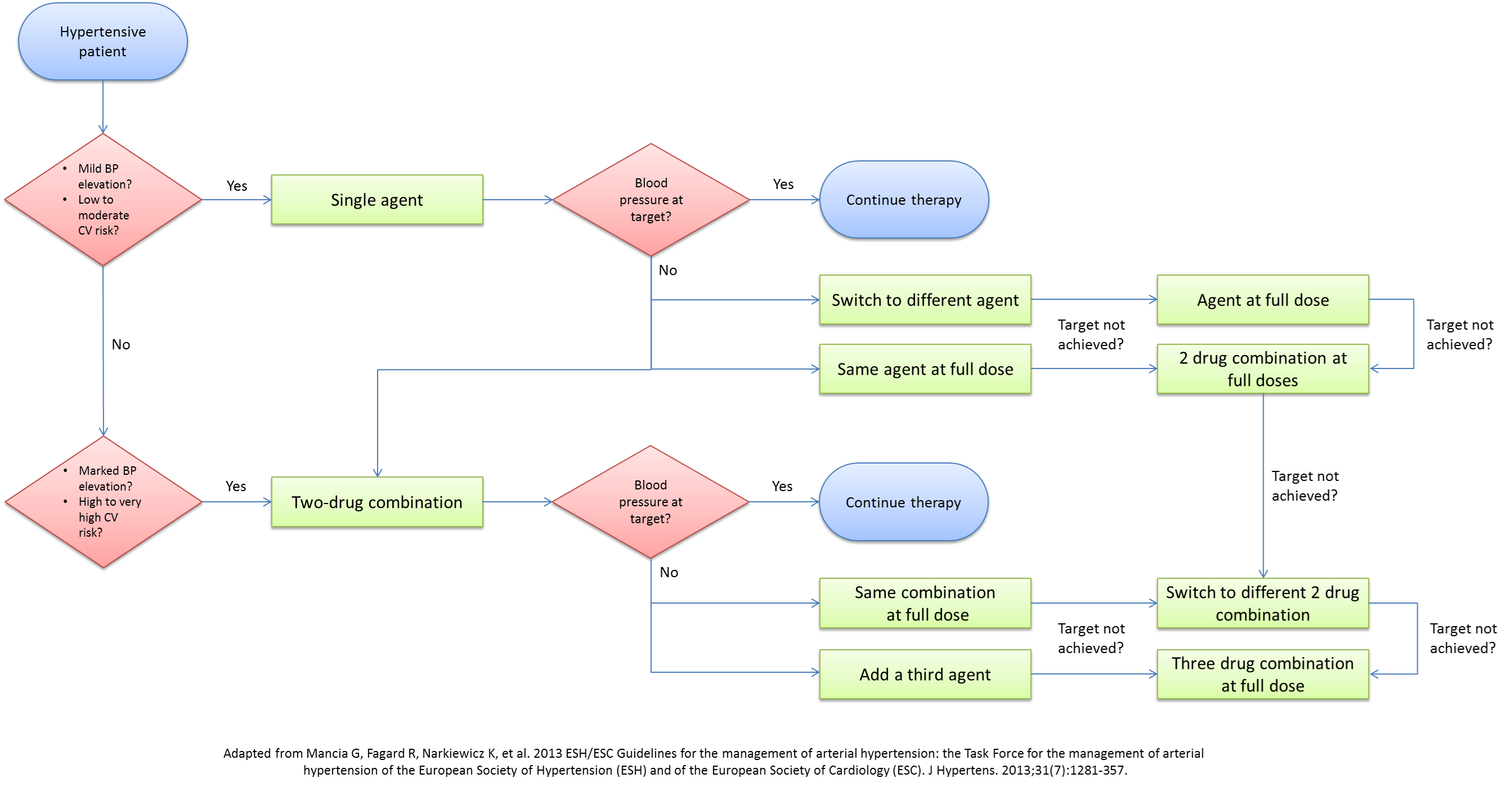
A lot of debate exists on the optimal approach to the medical management of hypertension. With the multitude of classes and agents that can be used, several questions arise about the single best agent, the optimal combination of agents, and the best step-wise approach to medical management. Although JNC7 tried to address these issues, almost a decade has passed since the release of their recommendations, with a myriad of studies and trials presenting newer compelling evidence to update the current recommendations. The 2013 ESH/ESC guidelines for the management of hypertension have dwelled into these issues and have outlined the rationale behind adopting a new approach. Below are the algorithms for the approach to the medical therapy of hypertension presented by JNC7 in 2004 and ESH/ESC in 2013.
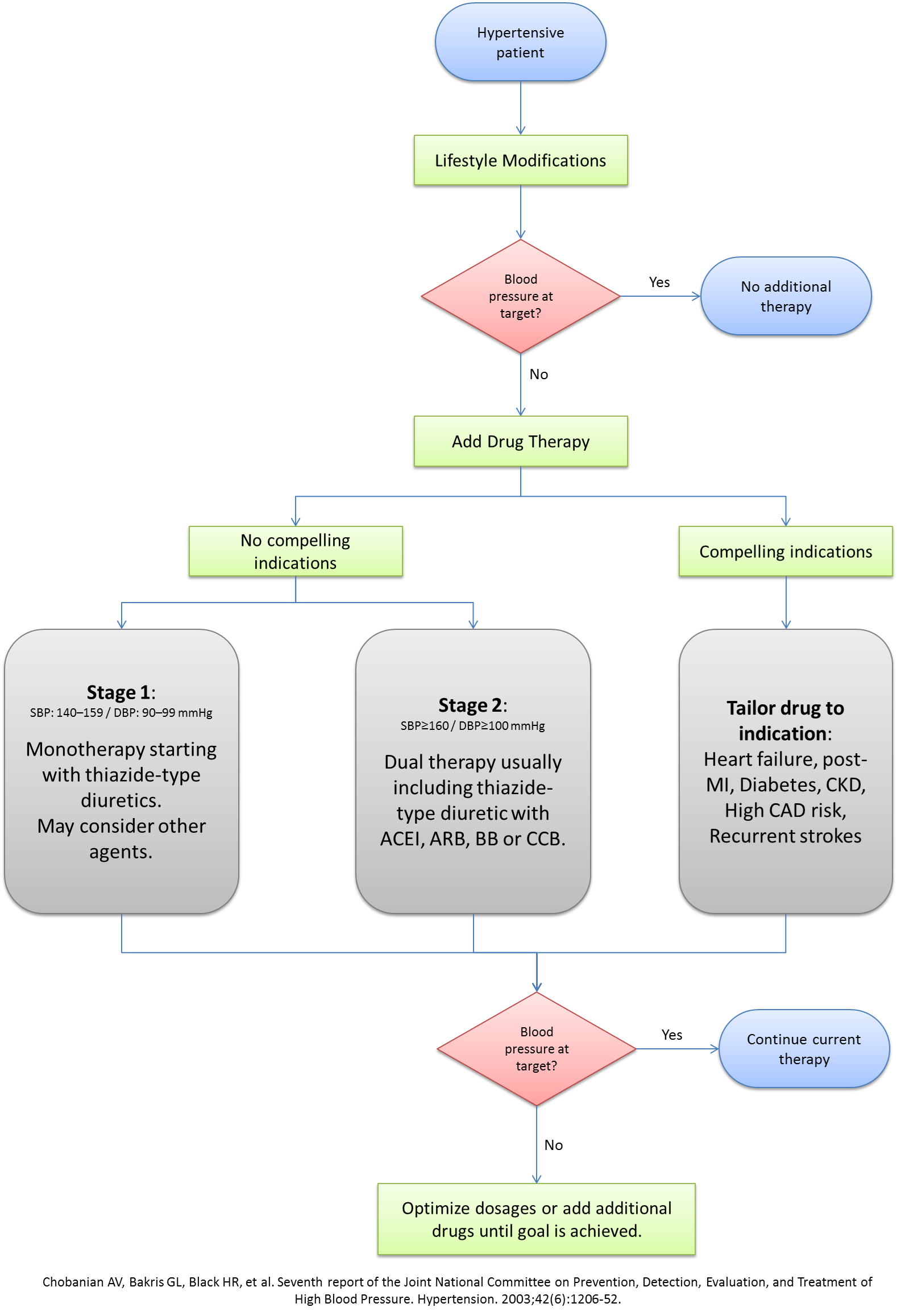
JNC- Seventh Report Recommendations: Medical Management[5]
| Compelling Indication | Recommended Drugs | Clinical Trial Basis |
| Heart failure | Diuretics, Beta blockers, ACEIs, ARBs, Aldosterone antagonist | ACC/AHA Heart Failure Guideline [6]; MERIT-HF [7]; COPERNICUS [8]; CIBIS [9]; SOLVD [10]; AIRE [11]; TRACE [12]; ValHEFT [13]; RALES [14] |
| Post-Myocardial infarction | Beta blockers, ACEIs, Aldosterone antagonist | ACC/AHA Post-MI Guideline [15]; BHAT [16]; SAVE [17]; Capricorn [18]; EPHESUS [19] |
| High coronary disease risk | Diuretics, Beta blockers, ACEIs, CCBs, | ALLHAT [20]; HOPE [21]; ANBP2 [22]; LIFE [23]; CONVINCE [24] |
| Diabetes | Diuretics, Beta blockers, ACEIs, ARBs, CCBs | NKF-ADA Guideline [3][4]; UKPDS [25]; ALLHAT [20] |
| Chronic kidney disease | ACEIs, ARBs | NFK Guideline [4]; Captopril Trial [26]; RENAAL [27]; IDNT [28]; REIN [29]; AASK [30] |
| Recurrent stroke prevention | Diuretics, ACEIs | PROGRESS [31] |
References
- ↑ Neal B, MacMahon S, Chapman N, Blood Pressure Lowering Treatment Trialists' Collaboration (2000). "Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Blood Pressure Lowering Treatment Trialists' Collaboration". Lancet. 356 (9246): 1955–64. PMID 11130523.
- ↑ Maldonado J (1998). "[Recommended article of the month: Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the hypertension optimal treatment (HOT) randomised trial]". Rev Port Cardiol. 17 (10): 843–4. PMID 9865094.
- ↑ 3.0 3.1 Arauz-Pacheco C, Parrott MA, Raskin P, American Diabetes Association (2003). "Treatment of hypertension in adults with diabetes". Diabetes Care. 26 Suppl 1: S80–2. PMID 12502624.
- ↑ 4.0 4.1 4.2 National Kidney Foundation (2002). "K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification". Am J Kidney Dis. 39 (2 Suppl 1): S1–266. PMID 11904577.
- ↑ Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL et al. (2003) Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 42 (6):1206-52. DOI:10.1161/01.HYP.0000107251.49515.c2 PMID: 14656957
- ↑ Hunt SA, Baker DW, Chin MH, Cinquegrani MP, Feldman AM, Francis GS et al. (2001) ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to revise the 1995 Guidelines for the Evaluation and Management of Heart Failure). J Am Coll Cardiol 38 (7):2101-13. PMID: 11738322
- ↑ Tepper D (1999) Frontiers in congestive heart failure: Effect of Metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Congest Heart Fail 5 (4):184-185. PMID: 12189311
- ↑ Packer M, Coats AJ, Fowler MB, Katus HA, Krum H, Mohacsi P et al. (2001) Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med 344 (22):1651-8. DOI:10.1056/NEJM200105313442201 PMID: 11386263
- ↑ (1994) A randomized trial of beta-blockade in heart failure. The Cardiac Insufficiency Bisoprolol Study (CIBIS). CIBIS Investigators and Committees. Circulation 90 (4):1765-73. PMID: 7923660
- ↑ (1991) Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. The SOLVD Investigators. N Engl J Med 325 (5):293-302. DOI:10.1056/NEJM199108013250501 PMID: 2057034
- ↑ (1993) Effect of ramipril on mortality and morbidity of survivors of acute myocardial infarction with clinical evidence of heart failure. The Acute Infarction Ramipril Efficacy (AIRE) Study Investigators. Lancet 342 (8875):821-8. PMID: 8104270
- ↑ Køber L, Torp-Pedersen C, Carlsen JE, Bagger H, Eliasen P, Lyngborg K et al. (1995) A clinical trial of the angiotensin-converting-enzyme inhibitor trandolapril in patients with left ventricular dysfunction after myocardial infarction. Trandolapril Cardiac Evaluation (TRACE) Study Group. N Engl J Med 333 (25):1670-6. DOI:10.1056/NEJM199512213332503 PMID: 7477219
- ↑ Cohn JN, Tognoni G, Valsartan Heart Failure Trial Investigators (2001) A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med 345 (23):1667-75. DOI:10.1056/NEJMoa010713 PMID: 11759645
- ↑ Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A et al. (1999) The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med 341 (10):709-17. DOI:10.1056/NEJM199909023411001 PMID: 10471456
- ↑ Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JS et al. (2002) ACC/AHA 2002 guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction--summary article: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee on the Management of Patients With Unstable Angina). J Am Coll Cardiol 40 (7):1366-74. PMID: 12383588
- ↑ (1982) A randomized trial of propranolol in patients with acute myocardial infarction. I. Mortality results. JAMA 247 (12):1707-14. PMID: 7038157
- ↑ Hager WD, Davis BR, Riba A, Moye LA, Wun CC, Rouleau JL et al. (1998) Absence of a deleterious effect of calcium channel blockers in patients with left ventricular dysfunction after myocardial infarction: The SAVE Study Experience. SAVE Investigators. Survival and Ventricular Enlargement. Am Heart J 135 (3):406-13. PMID: 9506325
- ↑ Dargie HJ (2001) Effect of carvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: the CAPRICORN randomised trial. Lancet 357 (9266):1385-90. PMID: 11356434
- ↑ Pitt B, Remme W, Zannad F, Neaton J, Martinez F, Roniker B et al. (2003) Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 348 (14):1309-21. DOI:10.1056/NEJMoa030207 PMID: 12668699
- ↑ 20.0 20.1 ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (2002) Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 288 (23):2981-97. PMID: 12479763
- ↑ Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G (2000) Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med 342 (3):145-53. DOI:10.1056/NEJM200001203420301 PMID: 10639539
- ↑ Wing LM, Reid CM, Ryan P, Beilin LJ, Brown MA, Jennings GL et al. (2003) A comparison of outcomes with angiotensin-converting--enzyme inhibitors and diuretics for hypertension in the elderly. N Engl J Med 348 (7):583-92. DOI:10.1056/NEJMoa021716 PMID: 12584366
- ↑ Dahlöf B, Devereux RB, Kjeldsen SE, Julius S, Beevers G, de Faire U et al. (2002) Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet 359 (9311):995-1003. DOI:10.1016/S0140-6736(02)08089-3 PMID: 11937178
- ↑ Black HR, Elliott WJ, Grandits G, Grambsch P, Lucente T, White WB et al. (2003) Principal results of the Controlled Onset Verapamil Investigation of Cardiovascular End Points (CONVINCE) trial. JAMA 289 (16):2073-82. DOI:10.1001/jama.289.16.2073 PMID: 12709465
- ↑ (1998) Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. UK Prospective Diabetes Study Group. BMJ 317 (7160):713-20. PMID: 9732338
- ↑ Lewis EJ, Hunsicker LG, Bain RP, Rohde RD (1993) The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. N Engl J Med 329 (20):1456-62. DOI:10.1056/NEJM199311113292004 PMID: 8413456
- ↑ Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH et al. (2001) Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 345 (12):861-9. DOI:10.1056/NEJMoa011161 PMID: 11565518
- ↑ Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA, Lewis JB et al. (2001) Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med 345 (12):851-60. DOI:10.1056/NEJMoa011303 PMID: 11565517
- ↑ (1997) Randomised placebo-controlled trial of effect of ramipril on decline in glomerular filtration rate and risk of terminal renal failure in proteinuric, non-diabetic nephropathy. The GISEN Group (Gruppo Italiano di Studi Epidemiologici in Nefrologia) Lancet 349 (9069):1857-63. PMID: 9217756
- ↑ Wright JT, Agodoa L, Contreras G, Greene T, Douglas JG, Lash J et al. (2002) Successful blood pressure control in the African American Study of Kidney Disease and Hypertension. Arch Intern Med 162 (14):1636-43. PMID: 12123409
- ↑ PROGRESS Collaborative Group (2001) Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet 358 (9287):1033-41. DOI:10.1016/S0140-6736(01)06178-5 PMID: 11589932