Cerebral hypoxia
| Cerebral hypoxia | |
 | |
|---|---|
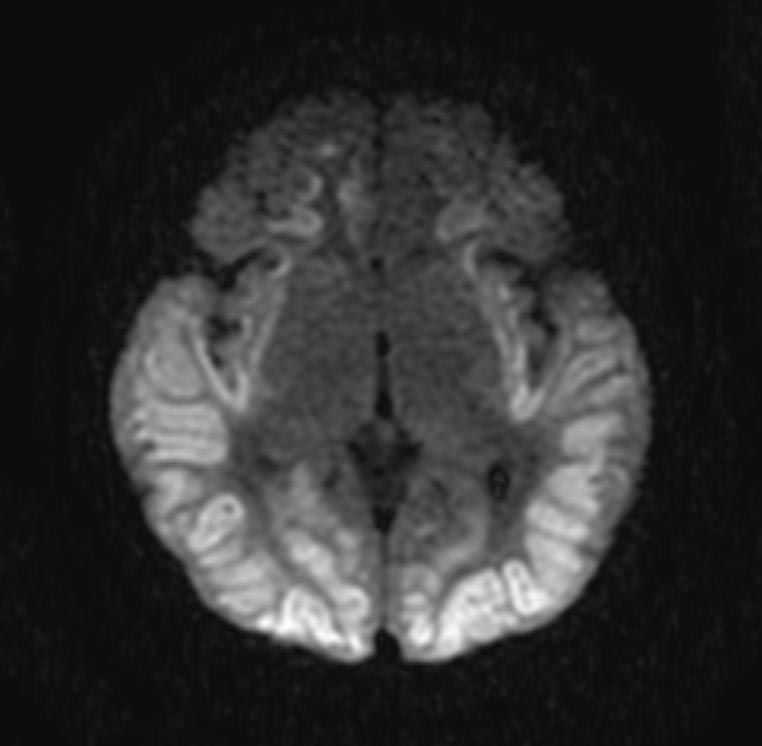
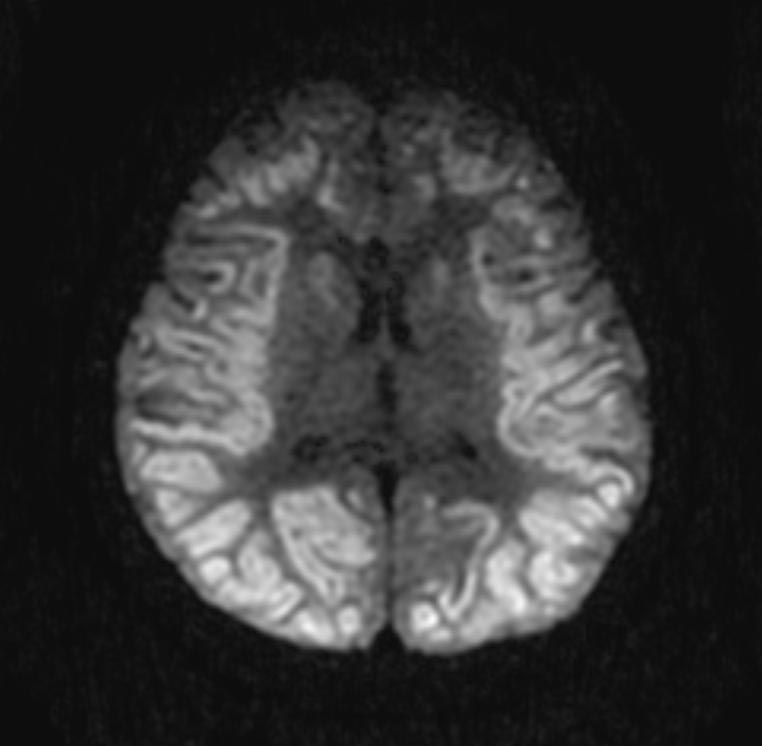
| Diffuse hypoxic ischemia. Image courtesy of RadsWiki |
|
WikiDoc Resources for Cerebral hypoxia |
|
Articles |
|---|
|
Most recent articles on Cerebral hypoxia Most cited articles on Cerebral hypoxia |
|
Media |
|
Powerpoint slides on Cerebral hypoxia |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Cerebral hypoxia at Clinical Trials.gov Trial results on Cerebral hypoxia Clinical Trials on Cerebral hypoxia at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Cerebral hypoxia NICE Guidance on Cerebral hypoxia
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Cerebral hypoxia Discussion groups on Cerebral hypoxia Patient Handouts on Cerebral hypoxia Directions to Hospitals Treating Cerebral hypoxia Risk calculators and risk factors for Cerebral hypoxia
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Cerebral hypoxia |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
- This article is about "cerebral hypoxia". For other uses of the term "hypoxia", see hypoxia.
Causes
Cerebral hypoxia can be caused by any event that severely interferes with the brain's ability to receive or process oxygen. This event may be internal or external to the body.
Mild and moderate forms of cerebral hypoxia may be caused by various diseases that interfere with breathing and blood oxygenation. Severe asthma and various sorts of anemia can cause some degree of diffuse cerebral hypoxia. Other causes include work in nitrogen rich environments, ascent from a deep water dive, flying at high altitudes in an un-pressurized cabin, and intense exercise at high altitudes prior to acclimatization.
Severe cerebral hypoxia and anoxia is usually caused by traumatic events. Examples include choking, drowning, strangulation, smoke inhalation, drug overdoses, crushing of the trachea, status asthmaticus, and shock.[1]
It is also recreationally self-induced in the choking game and in autoerotic asphyxiation.
Signs and symptoms
The brain requires approximately 3.3 ml of oxygen per 100 g of brain tissue per minute. Initially the body responds to lowered blood oxygen by redirecting blood to the brain and increasing cerebral blood flow. Blood flow may increase up to twice the normal flow but no more. If the increased blood flow is sufficient to supply the brain’s oxygen needs then no symptoms will result. [2]
However, if blood flow cannot be increased or if doubled blood flow does not correct the problem, symptoms of cerebral hypoxia will begin to appear. Mild symptoms include difficulties with complex learning tasks and reductions in short-term memory. If oxygen deprivation continues, cognitive disturbances and decreased motor control will result.[2] The skin may also appear bluish (cyanosis) and heart rate increases. Continued oxygen deprivation results in fainting, long term loss of consciousness, coma, seizures, cessation of brain stem reflexes, and brain death.[3]
Objective measurements of the severity of cerebral hypoxia depend on the cause. Blood oxygen saturation may be used for hypoxic hypoxia, but is generally meaningless in other forms of hypoxia. In hypoxic hypoxia 95-100% saturation is considered normal. 91-94% is considered mild. 86-90% is considered moderate. Anything below 86% is considered severe.[4]
It should be noted that cerebral hypoxia refers to oxygen levels in brain tissue, not blood. Blood oxygenation will usually appear normal in cases of hypemic, ischemic and hystoxic cerebral hypoxia. Even in hypoxic hypoxia blood measures are only an approximate guide – the oxygen level in the brain tissue will depend on how the body deals with the reduced oxygen content of the blood.
Diagnostic Findings
- Diffuse loss of gray/white differentiation
- Diffuse sulcal effacement
Patient #1:
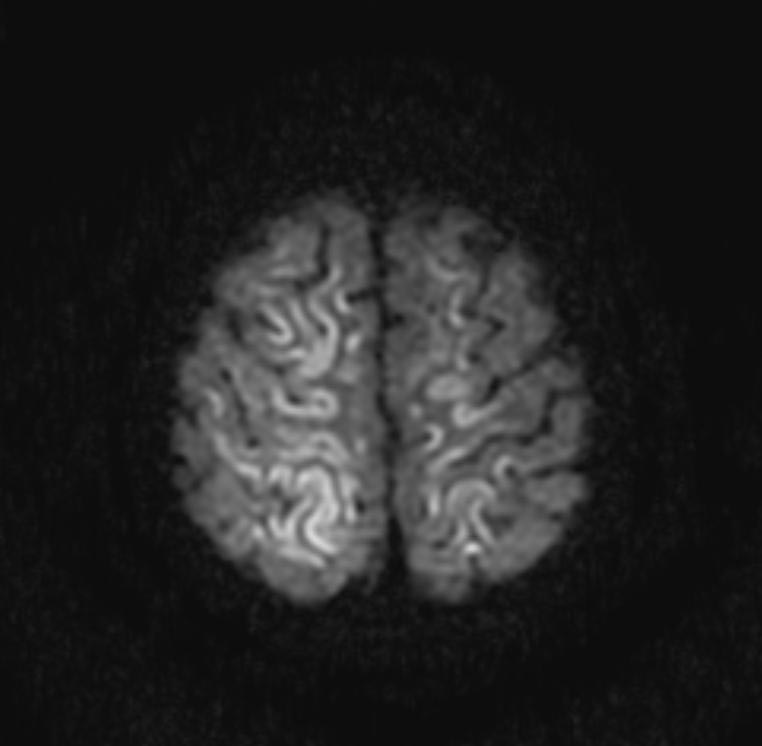
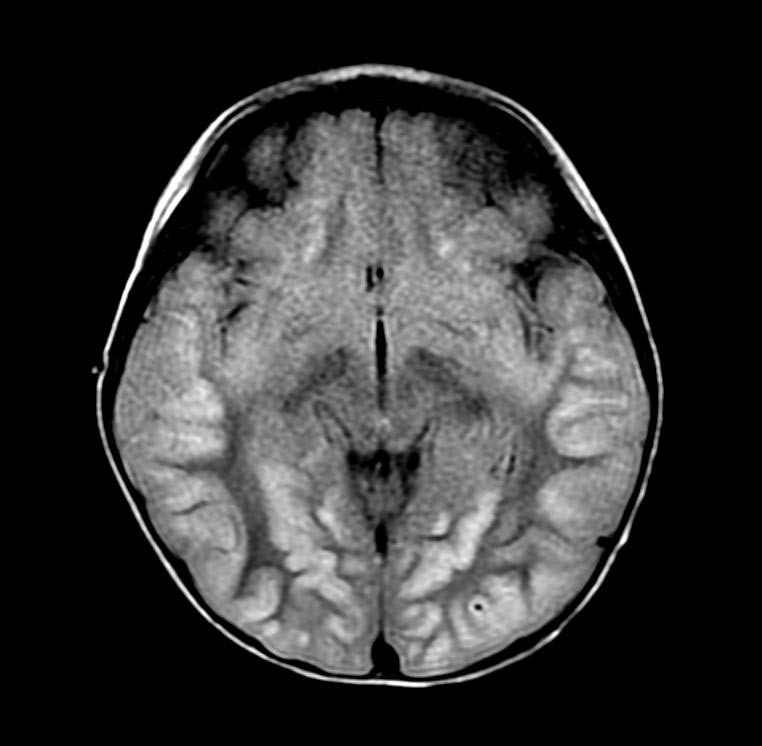
Patient #2:
-
DWI
-
DWI
-
DWI
-
DWI
-
FLAIR
-
FLAIR
-
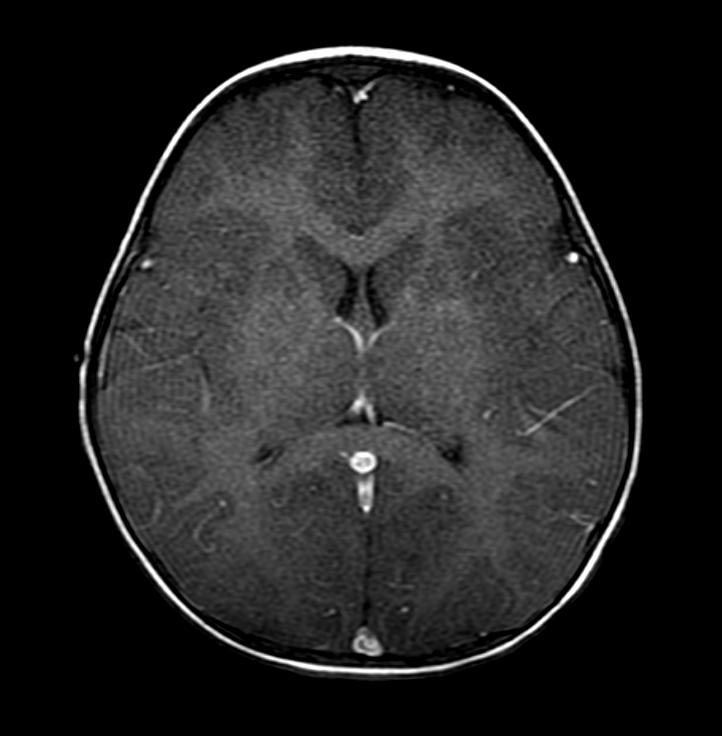
T1 with GAD
Treatment
The first goal of treatment is to restore oxygen to the brain. The method of restoration depends on the cause of the hypoxia.[5] For mild to moderate cases of hypoxia, removal of the cause of hypoxia may be sufficient. Inhaled oxygen may also be provided. In severe cases treatment may also involve life support and damage control measures.
A deep coma will interfere with body’s breathing reflexes even after the initial cause of hypoxia has been dealt with. Mechanical ventilation may be required. Additionally severe cerebral hypoxia causes an elevated heart rate. In extreme cases the heart may tire and stop pumping. CPR, defibrilation, epinephrine, and atropine may all be tried in an effort to get the heart to resume pumping.[4]
Severe cerebral hypoxia can also cause seizures. Seizures put the patient at risk of self injury. If convulsions are sufficiently severe medical professionals may not be able to provide medical treatment. Various anti-convulsant drugs may need to be administered before treatment can continue.
Brain damage can occur both during and after oxygen deprivation. During oxygen deprivation, cells die due to an increasing acidity in the brain tissue (acidosis). Additionally, during the period of oxygen deprivation, materials that can easily create free radicals build up. When oxygen enters the tissue these materials interact with oxygen to create high levels of oxidants. Oxidants interfere with the normal brain chemistry and cause further damage. This is called reperfusion injury.
Techniques for preventing damage to brain cells are an area of on-going research. Controlled hypothermia, anti-oxidant drugs, control of blood glucose levels, and hemodilution (thinning of the blood) coupled with drug-induced hypertension are some treatment techniques currently under investigation.[6]
In severe cases it is extremely important to act quickly. Brain cells are very sensitive to reduced oxygen levels. Once deprived of oxygen they will begin to die off within five minutes.[6]
Prognosis
Mild and moderate cerebral hypoxia generally has no impact beyond the episode of hypoxia. Severe cerebral hypoxia is another matter. Outcome will depend on the success of damage control measures, the amount of brain tissue deprived of oxygen, and the speed with which oxygen was restored to the brain.
If cerebral hypoxia was localized to a specific part of the brain, brain damage will be localized to that region. The long term effects will depend on the purpose of that portion of the brain. Damage to the Broca and Wernicke’s areas of the brain (left side) typically causes problems with speech and language. Damage to the right side of the brain may interfere with the ability to express emotions or interpret what one sees. Damage on either side can cause paralysis of the opposite side of the body.
The effects of certain kinds of severe generalized hypoxias may take time to develop. For example, the long term effects of serious carbon monoxide poisoning usually may take several weeks to appear. Recent research suggests this may be due to an autoimmune response caused by CO induced changes in the myelin sheath surrounding neurons.[7]
If hypoxia results in coma, the length of unconsciousness is often used as an indication of long term damage. In some cases coma can give the brain an opportunity to heal and regenerate,[8] but, in general, the longer a coma continues the greater the likelihood that the person will remain in a vegetative state until death.[1] Even if the patient wakes up, brain damage is likely to be significant enough to prevent a return to normal functioning.
The effects of long term comas are not limited to the comatose person. Long term coma can have significant impact on their families.[9] Families of coma victims often have idealized images of the outcome based on Hollywood movie depictions of coma.[10] Adjusting to the realities of ventilators, feeding tubes, bedsores and muscle wasting may be difficult.[11] Treatment decision often involve complex ethical choices and can strain family dynamics.[12]
See also
References
- ↑ 1.0 1.1 National Institute of Neurological Disorders and Stroke (February 8, 2007). "Cerebral Hypoxia Information Page". U.S. National Institutes of Health. Retrieved 2007-04-13.
- ↑ 2.0 2.1 Butterworth, Roger F. (1999). "Hypoxic Encephalopathy". In: Siegel, George J. et al. (eds.) Basic Neurochemistry: Molecular, Cellular and Medical Aspects, 6th edition, Philadelphia: Lippincott Williams & Wilkins. ISBN 039751820X. Freely available at National Center for Biotechnology Information Bookshelf. Retrieved on 2007-04-13.
- ↑ "Cerebral hypoxia". MedlinePlus Medical Encyclopedia. U.S. National Library of Medicine. 2007-04-05. Retrieved 2007-04-13.
- ↑ 4.0 4.1 Template:PDFlink. Maryland Institute for Emergency Medical Services Systems (2004). Retrieved on 2007-04-13.
- ↑ "Cerebral hypoxia". Health-cares.net. Retrieved 2007-04-13.
- ↑ 6.0 6.1 Richmond TS (May 1997). "Cerebral Resuscitation after Global Brain Ischemia". AACN Clinical Issues 8 (2). Retrieved on 2007-04-13. Free full text at the American Association of Critical-Care Nurses website.
- ↑ University Of Pennsylvania Medical Center (September 6, 2004). "Long-term Effects Of Carbon Monoxide Poisoning Are An Autoimmune Reaction". ScienceDaily. Retrieved 2007-04-13.
- ↑ Phillips, Helen (July 3, 2006). "'Rewired brain' revives patient after 19 years". New Scientist. Retrieved 2007-04-13.
- ↑ Mayo Clinic staff (May 17, 2006). "Coma: Coping skills". Mayo Clinic. Retrieved 2007-04-13.
- ↑ Wijdicks EFM, Wijdicks CA (2006). "The portrayal of coma in contemporary motion pictures". Neurology 66 (9): 1300–1303. PMID 16682658.
- ↑ Konig P et al (1992). "Psychological counseling of the family of patients with craniocerebral injuries (psychological family counseling of severely ill patients)". Zentralbl Neurochir 53 (2): 78–84. PMID 1636327.
- ↑ Montgomery V et al (2002). "The effect of severe traumatic brain injury on the family". J Trauma 52 (6): 1121–4. PMID 12045640.
Template:CNS diseases of the nervous system Template:Vascular diseases