Burn pathophysiology
|
Burn Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Burn pathophysiology On the Web |
|
American Roentgen Ray Society Images of Burn pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Eman Alademi, M.D.[2]
Overview
A burn is an injury caused by heat, cold, electricity, chemicals, light, radiation, or friction. Burns can be highly variable in terms of the tissue affected, the severity, and resultant complications. Muscle, bone, blood vessel, and epidermal tissue can all be damaged with subsequent pain due to profound injury to nerve endings. Depending on the location affected and the degree of severity, a burn victim may experience a wide number of potentially fatal complications including shock, infection, electrolyte imbalance and respiratory distress. Beyond physical complications, burns can also result in severe psychological and emotional distress due to scarring and deformity.
Pathophysiology
Burns is the result of damage to the skin involving the two main layers - the thin, outer epidermis and the thicker, deeper dermis by a temperatures greater than 44 °C (111 °F), leads to cell and tissue damage because of breaking down of the cells proteins then start losing their three-dimensional shape. Burn caused by[1][2]:
- Electrical injuries (can be deceiving with small entry and exit wounds, however, there may be extensive internal organ injury or associated traumatic injuries).
- Chemical injuries (divided into acid or alkali burns. Alkali burns tend to be more severe causing more penetration deeper into the skin by liquefying the skin (liquefaction necrosis) and acid burns penetrate less because they cause a coagulation injury (coagulation necrosis).
| • Obvious pattern from cigarettes, lighters, irons |
| • Burns to soles, palms, genitalia, buttocks, perineum |
| • Symmetrical burns of uniform depth |
| • No splash marks in a scald injury. A child falling into a bath will splash; one that is placed into it may not |
| • Restraint injuries on upper limbs |
| • Is there sparing of flexion creases—that is, was child in fetal position (position of protection) when burnt? Does this correlate to a “tide line” of scald—that is, if child is put into a fetal position, do the burns line up? |
| • “Doughnut sign,” an area of spared skin surrounded by scald. If a child is forcibly held down in a bath of hot water, the part in contact with the bottom of the bath will not burn, but the tissue around will |
| • Other signs of physical abuse—bruises of varied age, poorly kempt, lack of compliance with health care (such as no immunisations) |
Most burns are small and superficial causing only local injuries, However, burns can be larger and deeper, and patients can also have a systemic response to severe burns [5][6]
Local response
The three zones of a burn were described by Jackson in 1947.
Zone of coagulation—This occurs at the point of maximum damage. In this zone there is irreversible tissue loss due to coagulation of the constituent proteins.
Zone of stasis—The surrounding zone of stasis is characterized by decreased tissue perfusion. The tissue in this zone is potentially salvageable. The main aim of burns resuscitation is to increase tissue perfusion here and prevent any damage becoming irreversible. Additional insults—such as prolonged hypotension, infection, or edema—can convert this zone into an area of complete tissue loss.
Zone of hyperemia—In this outermost zone tissue perfusion is increased. The tissue here will invariably recover unless there is severe sepsis or prolonged hypoperfusion.
These three zones of a burn are three dimensional, and loss of tissue in the zone of stasis will lead to the wound deepening as well as widening.
Systemic response
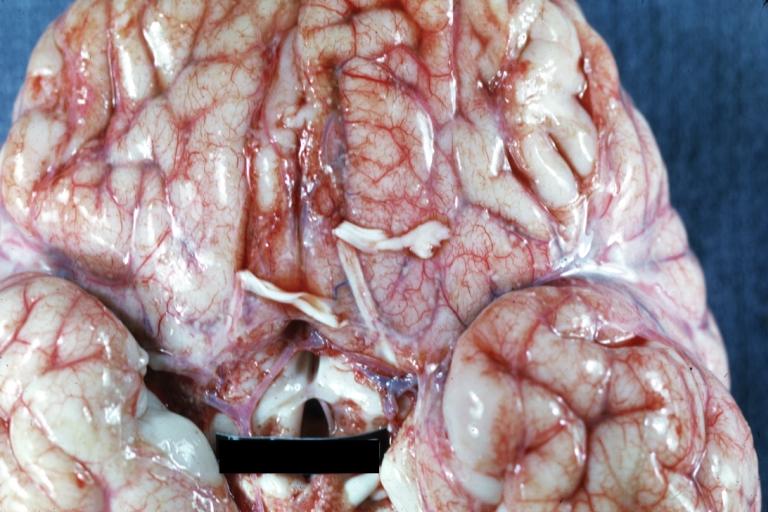
The increase of the catecholamines and cortisol,or The release of cytokines and other inflammatory mediators at the site of injury has a systemic effect once the burn reaches 30% of total body surface area and the site of injury lead to:
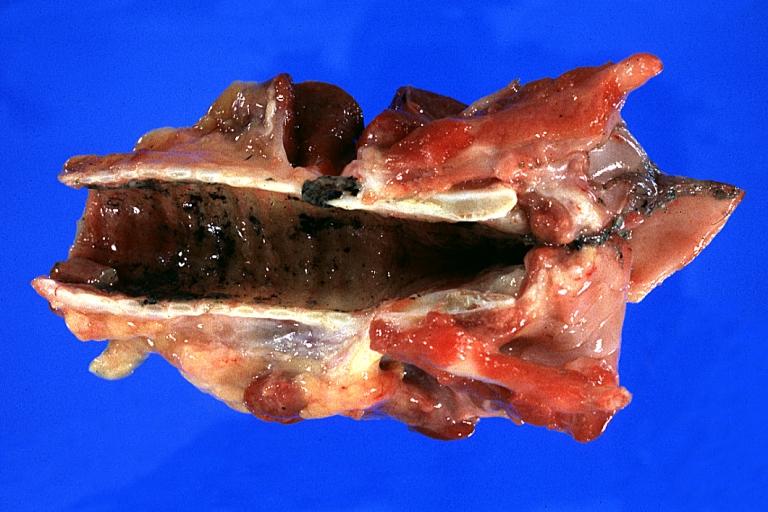
- Cardiovascular system changes—Capillary permeability is increased, leading to loss of intravascular proteins and fluids into the interstitial compartment. Peripheral and splanchnic vasoconstriction occurs. Myocardial contractility is decreased, possibly due to release of tumor necrosis factor α (TNFα). These change[7][8]s, coupled with fluid loss from the burn wound,[9] result in systemic hypotension and end organ hypoperfusion because of Increased levels of catecholamines. and a fast heart rate[10]
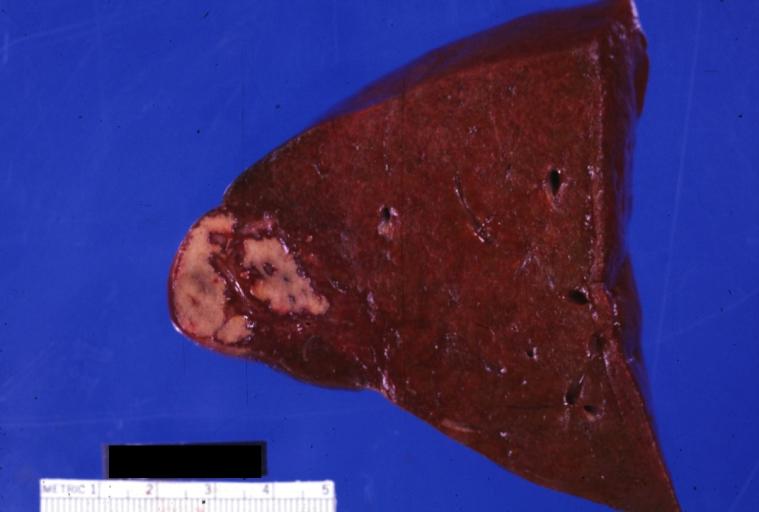
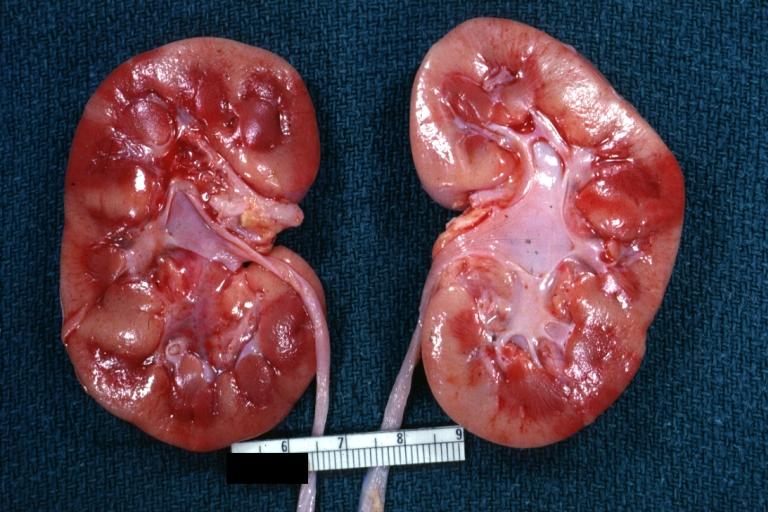
- Renal system changes—kidney failure because of the Poor blood flow to organs.[11]
- Respiratory system changes—Inflammatory mediators cause bronchoconstriction, and in severe burns adult respiratory distress syndrome can occur.
- Gastrointestinal system changes— stomach ulcers because of the Poor blood flow to organs.[12][13][14][15][16][17]
- Skin[18][19][20][21]
- Immune system changes—Non-specific down regulation of the immune response occurs, affecting both cell mediated and humeral pathway[22][23][24].[25][26]
- Metabolic changes—The basal metabolic rate increases up (hypermetabolic) to three times its original rate because of Increased levels of catecholamines and cortisol . This, coupled with splanchnic hypoperfusion, necessitates early and aggressive enteral feeding to decrease catabolism and maintain gut integrity. Immunological[27][28][29]
- Increased leakage of fluid from the capillaries, and subsequent tissue edema. This causes overall blood volume loss, with the remaining blood suffering significant plasma loss, making the blood more concentrated.[30]
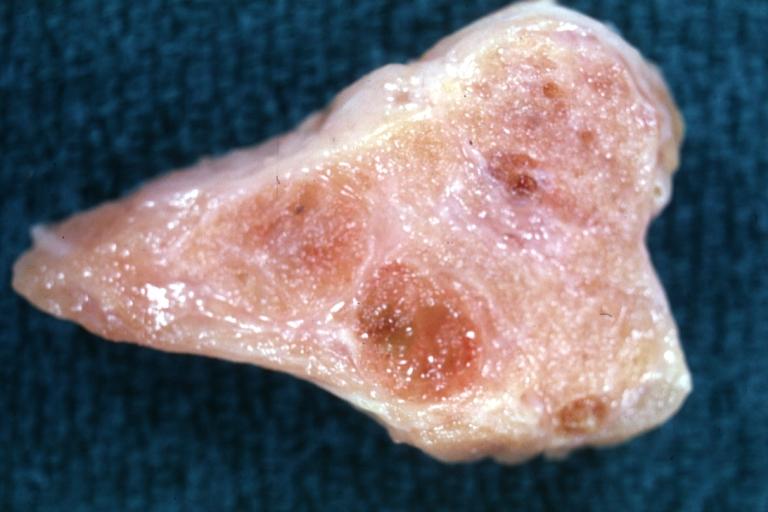
Gross Pathology
References
- ↑ Stiles K (July 2018). "Emergency management of burns: part 2". Emerg Nurse. 26 (2): 36–41. PMID 30095874.
- ↑ "Burn Evaluation And Management - StatPearls - NCBI Bookshelf".
- ↑ Hettiaratchy S, Dziewulski P (2004) ABC of burns: pathophysiology and types of burns. BMJ 328 (7453):1427-9. DOI:10.1136/bmj.328.7453.1427 PMID: 15191982 PMID: 15191982
- ↑ "Pathophysiology and Current Management of Burn Injury : Advances in Skin & Wound Care".
- ↑ "ABC of burns: Pathophysiology and types of burns".
- ↑ Rojas Y, Finnerty CC, Radhakrishnan RS, Herndon DN (December 2012). "Burns: an update on current pharmacotherapy". Expert Opin Pharmacother. 13 (17): 2485–94. doi:10.1517/14656566.2012.738195. PMC 3576016. PMID 23121414.
- ↑ Jeschke MG, Patsouris D, Stanojcic M, Abdullahi A, Rehou S, Pinto R; et al. (2015). "Pathophysiologic Response to Burns in the Elderly". EBioMedicine. 2 (10): 1536–48. doi:10.1016/j.ebiom.2015.07.040. PMC 4634201. PMID 26629550.
- ↑ Rehou S, Shahrokhi S, Thai J, Stanojcic M, Jeschke MG (2019). "Acute Phase Response in Critically Ill Elderly Burn Patients". Crit Care Med. 47 (2): 201–209. doi:10.1097/CCM.0000000000003516. PMID 30371519.
- ↑ Van de Veire NR, De Backer J, Ascoop AK, Middernacht B, Velghe A, Sutter JD (2006). "Echocardiographically estimated left ventricular end-diastolic and right ventricular systolic pressure in normotensive healthy individuals". Int J Cardiovasc Imaging. 22 (5): 633–41. doi:10.1007/s10554-006-9082-y. PMID 16541230.
- ↑ Ogawa T, Spina RJ, Martin WH, Kohrt WM, Schechtman KB, Holloszy JO; et al. (1992). "Effects of aging, sex, and physical training on cardiovascular responses to exercise". Circulation. 86 (2): 494–503. doi:10.1161/01.cir.86.2.494. PMID 1638717.
- ↑ Nyengaard JR, Bendtsen TF (1992). "Glomerular number and size in relation to age, kidney weight, and body surface in normal man". Anat Rec. 232 (2): 194–201. doi:10.1002/ar.1092320205. PMID 1546799.
- ↑ Clayton NA, Nicholls CM, Blazquez K, Brownlow C, Maitz PK, Fisher OM; et al. (2018). "Dysphagia in older persons following severe burns: Burn location is irrelevant to risk of dysphagia and its complications in patients over 75 years". Burns. 44 (8): 1997–2005. doi:10.1016/j.burns.2018.07.010. PMID 30107942.
- ↑ Pablo AM, Izaga MA, Alday LA (2003). "Assessment of nutritional status on hospital admission: nutritional scores". Eur J Clin Nutr. 57 (7): 824–31. doi:10.1038/sj.ejcn.1601616. PMID 12821882.
- ↑ Gariballa SE, Sinclair AJ (1998). "Nutrition, ageing and ill health". Br J Nutr. 80 (1): 7–23. doi:10.1017/s000711459800172x. PMID 9797639.
- ↑ Jeschke MG, Patsouris D, Stanojcic M, Abdullahi A, Rehou S, Pinto R; et al. (2015). "Pathophysiologic Response to Burns in the Elderly". EBioMedicine. 2 (10): 1536–48. doi:10.1016/j.ebiom.2015.07.040. PMC 4634201. PMID 26629550.
- ↑ Rosenfeld RM, Schwartz SR, Cannon CR, Roland PS, Simon GR, Kumar KA; et al. (2014). "Clinical practice guideline: acute otitis externa". Otolaryngol Head Neck Surg. 150 (1 Suppl): S1–S24. doi:10.1177/0194599813517083. PMID 24491310.
- ↑ Okaya T, Blanchard J, Schuster R, Kuboki S, Husted T, Caldwell CC; et al. (2005). "Age-dependent responses to hepatic ischemia/reperfusion injury". Shock. 24 (5): 421–7. doi:10.1097/01.shk.0000181282.14050.11. PMID 16247327.
- ↑ Goodson WH, Hunt TK (1979). "Wound healing and aging". J Invest Dermatol. 73 (1): 88–91. doi:10.1111/1523-1747.ep12532775. PMID 448182.
- ↑ Gosain A, DiPietro LA (2004). "Aging and wound healing". World J Surg. 28 (3): 321–6. doi:10.1007/s00268-003-7397-6. PMID 14961191.
- ↑ Zouboulis CC, Makrantonaki E (2011). "Clinical aspects and molecular diagnostics of skin aging". Clin Dermatol. 29 (1): 3–14. doi:10.1016/j.clindermatol.2010.07.001. PMID 21146726.
- ↑ Farage MA, Miller KW, Elsner P, Maibach HI (2013). "Characteristics of the Aging Skin". Adv Wound Care (New Rochelle). 2 (1): 5–10. doi:10.1089/wound.2011.0356. PMC 3840548. PMID 24527317.
- ↑ Emami SA, Motevalian SA, Momeni M, Karimi H (2016). "The epidemiology of geriatric burns in Iran: A national burn registry-based study". Burns. 42 (5): 1128–1132. doi:10.1016/j.burns.2016.03.011. PMID 27126815.
- ↑ Fitzwater J, Purdue GF, Hunt JL, O'Keefe GE (2003). "The risk factors and time course of sepsis and organ dysfunction after burn trauma". J Trauma. 54 (5): 959–66. doi:10.1097/01.TA.0000029382.26295.AB. PMID 12777910.
- ↑ Frankel JH, Boe DM, Albright JM, O'Halloran EB, Carter SR, Davis CS; et al. (2018). "Age-related immune responses after burn and inhalation injury are associated with altered clinical outcomes". Exp Gerontol. 105: 78–86. doi:10.1016/j.exger.2017.10.022. PMC 5871535. PMID 29080833.
- ↑ Jagger A, Shimojima Y, Goronzy JJ, Weyand CM (2014). "Regulatory T cells and the immune aging process: a mini-review". Gerontology. 60 (2): 130–7. doi:10.1159/000355303. PMC 4878402. PMID 24296590.
- ↑ Franceschi C, Bonafè M, Valensin S, Olivieri F, De Luca M, Ottaviani E; et al. (2000). "Inflamm-aging. An evolutionary perspective on immunosenescence". Ann N Y Acad Sci. 908: 244–54. doi:10.1111/j.1749-6632.2000.tb06651.x. PMID 10911963.
- ↑ Ward J, Phillips G, Radotra I, Smailes S, Dziewulski P, Zhang J; et al. (2018). "Frailty: an independent predictor of burns mortality following in-patient admission". Burns. 44 (8): 1895–1902. doi:10.1016/j.burns.2018.09.022. PMID 30361081.
- ↑ Romanowski KS, Barsun A, Pamlieri TL, Greenhalgh DG, Sen S (2015). "Frailty score on admission predicts outcomes in elderly burn injury". J Burn Care Res. 36 (1): 1–6. doi:10.1097/BCR.0000000000000190. PMID 25383979.
- ↑ Herndon DN, Tompkins RG (2004). "Support of the metabolic response to burn injury". Lancet. 363 (9424): 1895–902. doi:10.1016/S0140-6736(04)16360-5. PMID 15183630.
- ↑ "Porth Pathophysiology: Concepts of Altered Health States - Charlotte Pooler - كتب Google".