Brucellosis
For patient information on this page, click here
Template:DiseaseDisorder infobox
|
Brucellosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Brucellosis On the Web |
|
American Roentgen Ray Society Images of Brucellosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Raviteja Guddeti, M.B.B.S. [2]
Keywords and synonyms: Mediterranean fever; continued fever; Cyprus fever; goat fever; Gibraltar fever; Crimean fever; mountain fever; Neapolitan fever; rock fever; slow fever; febris melitensis; febris undulans; Bruce's septicemia; melitensis septicemia; melitococcosis; Brucelliasis; milk sickness; undulant fever; Malta fever
Overview
Brucellosis is a zoonosis (infectious disease transmitted from animals to humans) caused by bacteria of the genus Brucella. It is primarily a disease of domestic animals (goats, pigs, cattle, dogs, etc) and humans and has a worldwide distribution, mostly now in developing countries.
History and nomenclature
The disease now called brucellosis, under the name "Mediterranean fever", first came to the attention of British medical officers in Malta during the Crimean War in the 1850s. The causal relationship between organism and disease was first established by Dr. David Bruce in 1887. [1]
In 1897 Danish veterinarian Bernhard Bang isolated Brucella abortus as the agent and the additional name Bang's disease was assigned. In modern usage "Bang's disease" is often shortened to just "bangs" when ranchers discuss the disease or vaccine.
Maltese doctor and archaeologist Sir Temi Zammit identified unpasteurized milk as the major source of the pathogen in 1905, and it has since become known as Malta Fever, or deni rqiq locally. In cattle this disease is also known as contagious abortion and infectious abortion.
The popular name "undulant fever" originates from the characteristic undulance (or "wave-like" nature) of the fever which rises and falls over weeks in untreated patients. In the 20th Century, this name, along with "brucellosis" (after Brucella, named for Dr Bruce), gradually replaced the 19th Century names "Mediterranean fever" and "Malta fever".
Pathophysiology
Brucellosis is an infectious disease caused by the bacteria of the genus Brucella. These bacteria are primarily passed among animals, and they cause disease in many different vertebrates. Various Brucella species affect sheep, goats, cattle, deer, elk, pigs, dogs, and several other animals. Humans become infected by coming in contact with animals or animal products that are contaminated with these bacteria.
Humans are generally infected in one of three ways: eating or drinking something that is contaminated with Brucella, breathing in the organism (inhalation), or having the bacteria enter the body through skin wounds. The most common way to be infected is by eating or drinking contaminated milk products. When sheep, goats, cows, or camels are infected, their milk is contaminated with the bacteria. If the milk is not pasteurized, these bacteria can be transmitted to persons who drink the milk or eat cheeses made it.
Can brucellosis be spread from person to person?
Direct person-to-person spread of brucellosis is extremely rare. Mothers who are breast-feeding may transmit the infection to their infants. Sexual transmission has also been reported. For both sexual and breast-feeding transmission, if the infant or person at risk is treated for brucellosis, their risk of becoming infected will probably be eliminated within 3 days. Although uncommon, transmission may also occur via contaminated tissue transplantation. [2]
Transmission and incubation

The disease is transmitted either through contaminated or untreated milk (and its derivates) or through direct contact with infected animals, which may include dogs, pigs, camels and ruminants, primarily sheep, goats, cattle, American Bison. This also includes contact with their carcasses. Parturition rests are extremely rich in highy virulent brucellae . Brucellae, along with leptospira have the unique property of penetrate through intact human skin, so infection by mere hand contact with infectious material is likely to occur.
The disease is now usually associated with the consumption of unpasteurized milk and soft cheeses made from the milk of infected animals and with occupational exposures of veterinarians and slaughterhouse workers. Some vaccines used in livestock, most notably B. abortus strain 19 also cause disease in humans if accidentally injected. Problems with vaccine induced cases in the United States declined after the release of the RB-51 strain developed in the 1990s and the relaxation of laws requiring vaccination of cattle in many states.
The incubation period of brucellosis is, usually, of one to three weeks, but some rare instances may take several months to surface.
Epidemiology and Demographics
Brucellosis is not very common in the United States, where 100 to 200 cases occur each year. But brucellosis can be very common in countries where animal disease control programs have not reduced the amount of disease among animals.
Although brucellosis can be found worldwide, it is more common in countries that do not have good standardized and effective public health and domestic animal health programs. Areas currently listed as high risk are the Mediterranean Basin (Portugal, Spain, Southern France, Italy, Greece, Turkey, North Africa), South and Central America, Eastern Europe, Asia, Africa, the Caribbean, and the Middle East. Unpasteurized cheeses, sometimes called "village cheeses," from these areas may represent a particular risk for tourists [3].
Risk Factors
Inhalation of Brucella organisms is not a common route of infection, but it can be a significant hazard for people in certain occupations, such as those working in laboratories where the organism is cultured. Inhalation is often responsible for a significant percentage of cases in abattoir employees. Contamination of skin wounds may be a problem for persons working in slaughterhouses or meat packing plants or for veterinarians. Hunters may be infected through skin wounds or by accidentally ingesting the bacteria after cleaning deer, elk, moose, or wild pigs that they have killed.
My dog has been diagnosed with brucellosis. Is that a risk for me?
B. canis is the species of Brucella species that can infect dogs. This species has occasionally been transmitted to humans, but the vast majority of dog infections do not result in human illness. Although veterinarians exposed to blood of infected animals are at risk, pet owners are not considered to be at risk for infection. This is partly because it is unlikely that they will come in contact with blood, semen, or placenta of the dog. The bacteria may be cleared from the animal within a few days of treatment; however re-infection is common and some animal body fluids may be infectious for weeks. Immunocompromised persons (cancer patients, HIV-infected individuals, or transplantation patients) should not handle dogs known to be infected with B. canis.
I am a veterinarian, and I recently accidentally jabbed myself with the animal vaccine (RB-51 or strain 19, or REV-1) while I was vaccinating cows (or sheep, goats). What do I need to do?
These are live vaccines, and strain 19 is known to cause disease in humans. Although we know less about the other vaccines, the recommendations are the same. You should see a health care provider. A baseline blood sample should be collected for testing for antibodies. We recommend that you take antibiotics (doxycycline and rifampin for strain 19 and REV-1, or doxycycline alone for RB-51) for 3 weeks. At the end of that time you should be rechecked and a second blood sample should be collected. (The sample can also be collected at 2 weeks.) The same recommendations hold true for spraying vaccine in the eyes (6 weeks of treatment in this case) or spraying onto open wounds on the skin [4] .
Natural history, Complications and Prognosis
The disease's sequelae are highly variable and may include granulomatous hepatitis, arthritis, spondylitis, anemia, leukopenia, thrombocytopenia, meningitis, uveitis, optic neuritis and endocarditis.
Diagnosis
Brucellosis is diagnosed in a laboratory by finding Brucella organisms in samples of blood or bone marrow. Also, blood tests can be done to detect antibodies against the bacteria. If this method is used, two blood samples should be collected 2 weeks apart [5].
Symptoms
Acute brucellosis may begin with mild flu-like symptoms, or symptoms such as:
- Abdominal pain
- Back pain
- Chills
- Excessive sweating
- Fatigue
- Fever
- Headache
- Joint pain
- Loss of appetite
- Weakness
- Weight loss
- depression
High fever spikes usually occur every afternoon. The name "undulant" fever is because the fever rises and falls in waves.
Other symptoms that may occur with this disease:
- Muscle pain
- Swollen glands
The illness may be chronic and last for years.
In first stage of the disease, septicaemia occurs and leads to the classic triad of undulant fevers, sweating (often with characteristic smell, likened to wet hay) and migratory arthralgia and myalgia. In blood tests, is characteristic the leukopenia and anemia, some elevation of AST and ALT and positivity of classic Bengal Rose and Huddleson reactions. This complex is, at least in Portugal known as the Malta fever. During episodes of Malta fever, melitococcemia (presence of brucellae in blood) can usually be demonstrated by means of blood culture in tryptose medium or Albini medium. If untreated, the disease can give origin to focalizations or become chronic. The focalizations of brucellosis occur usually in bones and joints and spondylodisciitis of lumbar spine accompanied by sacroiliitis is very characteristic of this disease. Orchitis is also frequent in men.
Laboratory Findings
- Complete blood count and differential count - leukopenia, anemia
- Liver function tests - elevation of AST and ALT
- Demonstration of the agent: blood cultures in tryptose broth, bone marrow cultures. The growth of brucellae is extremely slow (they can take until 2 months to grow) and the culture poses a risk to laboratory personnel due to high infectivity of brucellae.
- Demonstration of antibodies against the agent either with the classic Huddleson, Wright and/or Bengal Rose reactions, either with ELISA or the 2-mercaptoethanol assay for IgM antibodies associated with chronic disease
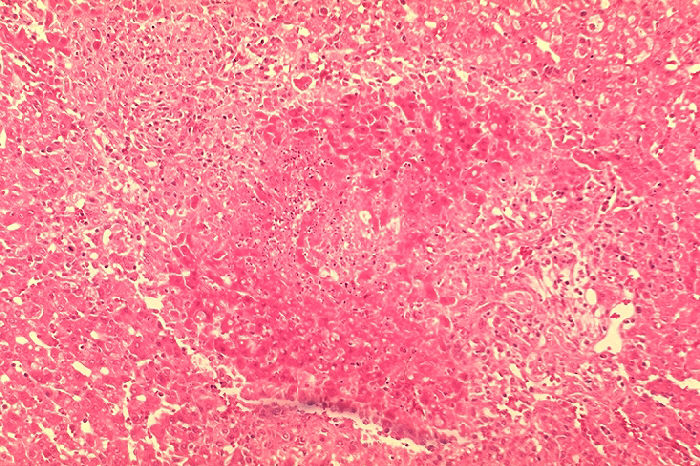
- Histologic evidence of granulomatous hepatitis (hepatic biopsy)
Imaging
X-ray
- Radiologic alterations in infected vertebrae : the Pedro Pons sign (preferential erosion of antero-superior corner of lumbar vertebrae) and marked osteophytosis are suspicious of brucellic spondylitis.
Treatment and prevention
Treatment can be difficult. Doctors can prescribe effective antibiotics. Usually, doxycycline and rifampin are used in combination for 6 weeks to prevent reoccuring infection. Depending on the timing of treatment and severity of illness, recovery may take a few weeks to several months. The use of more than one antibiotic is needed for several weeks, due to the fact that the bacteria incubates within cells. Mortality is low (<2%), and is usually associated with endocarditis [6].
The gold standard treatment for adults is daily intramuscular injections of streptomycin 1 g for 14 days and oral doxycycline 100 mg twice daily for 45 days (concurrently). Gentamicin 5 mg/kg by intramuscular injection once daily for 7 days is an acceptable substitute when streptomycin is not available or difficult to obtain.[7] Another widely used regimen is doxycycline plus rifampin twice daily for at least 6 weeks. This regimen has the advantage of oral administration. A triple therapy of doxycycline, together with rifampin and cotrimoxazole has been used succefully to treat neurobrucellosis. [8] Doxycycline is able to cross the blood-brain barrier, but requires the addition of two other drugs to prevent relapse. Ciprofloxacin and co-trimoxazole therapy is associated with an unacceptably high rate of relapse. In brucellic endocarditis surgery is required for an optimal outcome. Even with optimal antibrucellic therapy relapses still occur in 5-10 percent of patients with Malta fever. The main way of preventing brucellosis is by using fastidious hygiene in producing raw milk products, or by pasteurization of all milk that is to be ingested by human beings, either in its pure form or as a derivate, such as cheese. Experiments have shown that cotrimoxyzol and rifampin are both safe drugs to use in treatment of pregnant women who have Brucellosis.
Primary Prevention
To prevent brucellosis, unpasteurized milk, cheese, or ice cream should be avoided while traveling. IHunters and animal herdsman should use rubber gloves when handling viscera of animals. There is no vaccine available for humans.
Biological warfare
In 1954, B. suis became the first agent weaponized by the U.S. at its Pine Bluff Arsenal in Arkansas. Brucella species survive well in aerosols and resist drying. Brucella and all other remaining biological weapons in the US arsenal were destroyed in 1971-72 when the U.S. offensive biological weapons (BW) program was discontinued. [9]
The United States BW program focused on three agents of the Brucella group:
- Porcine Brucellosis (Agent US)
- Bovine Brucellosis (Agent AB)
- Caprina Brucellosis (Agent AM)
Agent US was in advanced development by the end of the Second World War. When the USAF wanted a biological warfare capability, the Chemical Corps offered agent US in the M114 bomblet, based after the 4-pound bursting bomblet developed for anthrax in the Second World War. Though the capability was developed, operational testing indicated that the weapon was less than desirable, and the USAF termed it an interim capability until replaced by a more effective biological weapon. The main drawbacks of the M114 with agent US was that it was incapacitating (the USAF wanted "killer" agents), the storage stability was too low to allow for storing at forward air bases, and the logistical requirements to neutralize a target were far higher than originally anticipated, requiring unreasonable logistical air support.
Agents US and AB had a median infective dose of 500 org/person, and AM was 300 org/person. The rate-of-action was believed to be 2 weeks, with a duration of action of several months. The lethality estimate was based on epidemiological information at 1 - 2%. AM was always believed to be a more virulent disease, and a 3% fatality rate was expected.
Historical names
In addition to "Malta Fever" and "undulant fever", the following obsolete names have previously been applied to brucellosis:
- Mediterranean fever
- continued fever
- Cyprus fever
- goat fever
- Gibraltar fever
- Crimean fever
- mountain fever
- Neapolitan fever
- rock fever
- slow fever
- febris melitensis
- febris undulans
- Bruce's septicemia
- melitensis septicemia
- melitococcosis
- Brucelliasis
- Milk Sickness
Acknowledgements
The content on this page was first contributed by: C. Michael Gibson, M.S., M.D.
List of contributors:
Pilar Almonacid
References
- ↑ Wilkinson, Lise (1993). "Brucellosis", In Kiple, Kenneth F. (ed.), The Cambridge World History of Human Disease, Cambridge: Cambridge University Press).
- ↑ http://www.cdc.gov/ncidod/dbmd/diseaseinfo/brucellosis_g.htm#whatis
- ↑ http://www.cdc.gov/ncidod/dbmd/diseaseinfo/brucellosis_g.htm#whatis
- ↑ http://www.cdc.gov/ncidod/dbmd/diseaseinfo/brucellosis_g.htm#whatis
- ↑ http://www.cdc.gov/ncidod/dbmd/diseaseinfo/brucellosis_g.htm#
- ↑ http://www.cdc.gov/ncidod/dbmd/diseaseinfo
- ↑ Roushan MRH, Mohraz M, Hajiahmadi M, Ramzani A, Valayati AA (2006). "Efficacy of gentamicin plus doxycycline versus streptomycin plus doxycycline in the treatment of brucellosis in humans". Clin Infect Dis. 42 (8): 1075&ndash, 80.
- ↑ McLean DR, Russell N, Khan MY (1992). "Neurobrucellosis: Clinical and therapeutic features". Clin Infect Dis. 15: 582&ndash, 90.
- ↑ Woods, Lt Col Jon B. (ed.) (April 2005). USAMRIID’s Medical Management of Biological Casualties Handbook (6th ed. ed.). U.S. Army Medical Institute of Infectious Diseases, Fort Detrick, Maryland. p. 53. External link in
|title=(help)
See also
- Swine brucellosis
- Florence Nightingale (She may have suffered from brucellosis in the Crimea.)
External links
- Prevention about Brucellosis from Center for Disease Control
- Template:WhoNamedIt
- Template:GPnotebook
- Template:FPnotebook
- Brucellosis in Dogs from The Pet Health Library
- Brucella from PATRIC
bs:Bruceloza
bg:Бруцелоза
de:Brucellose
et:Brutselloos
fa:تب مالت
hr:Bruceloza
it:Brucellosi
he:ברוצלוזיס
nl:Brucellose
sr:Бруцелоза
fi:Bruselloosi