Bronchoalveolar carcinoma
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Historical Perspective
- [Disease name] was first discovered by [scientist name], a [nationality + occupation], in [year] during/following [event].
- In [year], [gene] mutations were first identified in the pathogenesis of [disease name].
- In [year], the first [discovery] was developed by [scientist] to treat/diagnose [disease name].
Classification
- Bronchoalveolar Carcinoma may be classified according to pathology into fo subtypes/groups:
- Pathology of lung adenocarcinomas according to previous 2004 WHO and current IASLC/ATS/ERS classifications[1]
| 2004 WHO classification |
| Mixed subtype |
| Acinar |
| Papillary |
| BAC |
| Non mucinous |
| Mucinous |
| Mixed |
| Solid adenocarcinoma |
| Colloid |
| Fetal |
| Mucinous cystadenocarcinoma |
| Signet-ring |
| Clear-cell |
| Major changes in the new IASLC/ATS/ERS classification |
| Discontinuation of the term BAC |
| Discontinuation of the mixed subtype |
| Comprehensive pathologic subtyping in 5% increments and classification of adenocarcinomas according to the predominant subtype |
| Introduction of AIS and MIA as new entities |
| Introduction of micropapillary adenocarcinoma as a predominant subtype |
| Introduction of lepidic predominant adenocarcinoma and lepidic growth as new terminologies |
| Exclusion of signet-ring and clear cell adenocarcinomas |
| IASLC/ATS/ERS classification |
| Pre-invasive lesions |
| Atypical adenomatous hyperplasia |
| AIS |
| Non-mucinous |
| Mucinous |
| Mixed |
| MIA |
| Non-mucinous |
| Mucinous |
| Mixed |
| Invasive adenocarcinomas |
| Lepidic predominant |
| Acinar predominant |
| Papillary predominant |
| Micropapillary predominant |
| Solid predominant with mucin production |
| Variants of invasive adenocarcinomas |
| IMA |
| Colloid |
| Fetal |
| Enteric |
WHO, World Health Organization; IASLC, International Association for the Study of Lung Cancer; ATS, American Thoracic Society; ERS, European Respiratory Society; BAC, bronchioloalveolar carcinoma; AIS, adenocarcinoma in situ; MIA, minimally invasive adenocarcinoma; IMA, invasive mucinous adenocarcinoma.
Pathophysiology
- The pathogenesis of [disease name] is characterized by [feature1], [feature2], and [feature3].
- The [gene name] gene/Mutation in [gene name] has been associated with the development of [disease name], involving the [molecular pathway] pathway.
- On gross pathology, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
- On microscopic histopathological analysis, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
Clinical Features
Differentiating [disease name] from other Diseases
- [Disease name] must be differentiated from other diseases that cause [clinical feature 1], [clinical feature 2], and [clinical feature 3], such as:
- [Differential dx1]
- [Differential dx2]
- [Differential dx3]
Epidemiology and Demographics
- The prevalence of [disease name] is approximately [number or range] per 100,000 individuals worldwide.
- In [year], the incidence of [disease name] was estimated to be [number or range] cases per 100,000 individuals in [location].
Age
- Patients of all age groups may develop [disease name].
- [Disease name] is more commonly observed among patients aged [age range] years old.
- [Disease name] is more commonly observed among [elderly patients/young patients/children].
Gender
- [Disease name] affects men and women equally.
- [Gender 1] are more commonly affected with [disease name] than [gender 2].
- The [gender 1] to [Gender 2] ratio is approximately [number > 1] to 1.
Race
- There is no racial predilection for [disease name].
- [Disease name] usually affects individuals of the [race 1] race.
- [Race 2] individuals are less likely to develop [disease name].
Risk Factors
- Common risk factors in the development of [disease name] are [risk factor 1], [risk factor 2], [risk factor 3], and [risk factor 4].
Natural History, Complications and Prognosis
- The majority of patients with [disease name] remain asymptomatic for [duration/years].
- Early clinical features include [manifestation 1], [manifestation 2], and [manifestation 3].
- If left untreated, [#%] of patients with [disease name] may progress to develop [manifestation 1], [manifestation 2], and [manifestation 3].
- Common complications of [disease name] include [complication 1], [complication 2], and [complication 3].
- Prognosis is generally [excellent/good/poor], and the [1/5/10year mortality/survival rate] of patients with [disease name] is approximately [#%].
Diagnosis
Diagnostic Criteria
- The diagnosis of [disease name] is made when at least [number] of the following [number] diagnostic criteria are met:
- [criterion 1]
- [criterion 2]
- [criterion 3]
- [criterion 4]
Symptoms
- [Disease name] is usually asymptomatic.
- Symptoms of [disease name] may include the following:
- [symptom 1]
- [symptom 2]
- [symptom 3]
- [symptom 4]
- [symptom 5]
- [symptom 6]
Physical Examination
- Patients with [disease name] usually appear [general appearance].
- Physical examination may be remarkable for:
- [finding 1]
- [finding 2]
- [finding 3]
- [finding 4]
- [finding 5]
- [finding 6]
Laboratory Findings
- There are no specific laboratory findings associated with [disease name].
- A [positive/negative] [test name] is diagnostic of [disease name].
- An [elevated/reduced] concentration of [serum/blood/urinary/CSF/other] [lab test] is diagnostic of [disease name].
- Other laboratory findings consistent with the diagnosis of [disease name] include [abnormal test 1], [abnormal test 2], and [abnormal test 3].
Imaging Findings
- There are no [imaging study] findings associated with [disease name].
- [Imaging study 1] is the imaging modality of choice for [disease name].
- On [imaging study 1], [disease name] is characterized by [finding 1], [finding 2], and [finding 3].
- [Imaging study 2] may demonstrate [finding 1], [finding 2], and [finding 3].
-
CXR- Bronchoalveolar Carcinoma
-
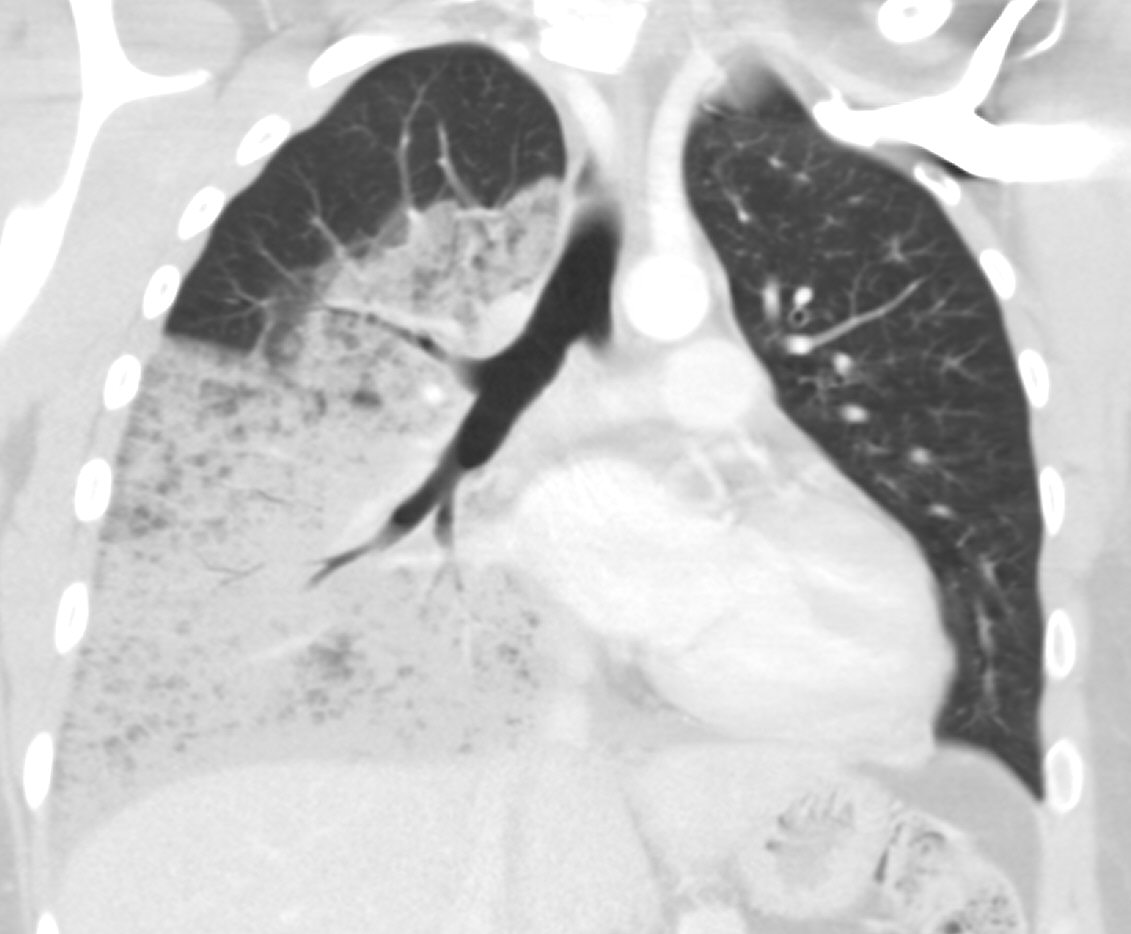
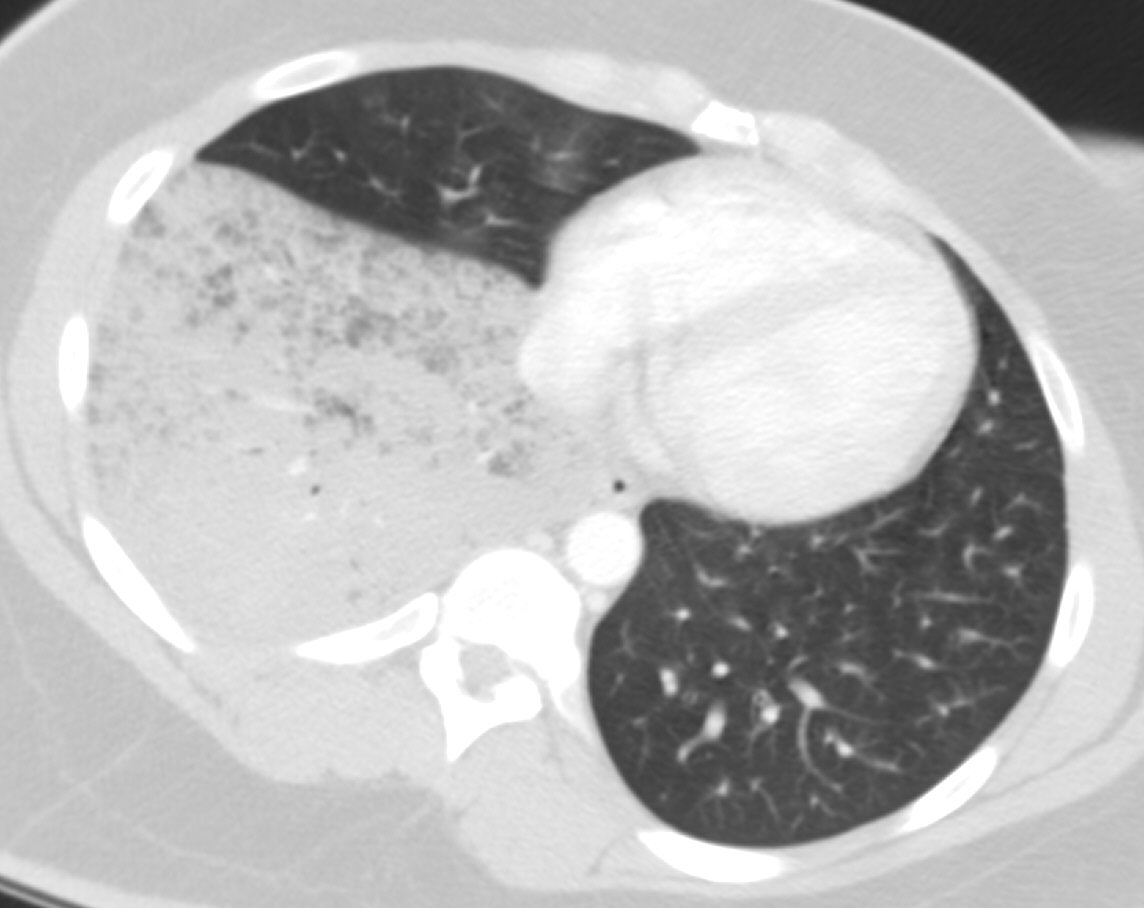
CT SCAN: Bronchoalveolar Carcinoma
-
CT SCAN: Bronchoalveolar Carcinoma
Other Diagnostic Studies
- [Disease name] may also be diagnosed using [diagnostic study name].
- Findings on [diagnostic study name] include [finding 1], [finding 2], and [finding 3].
Treatment
Medical Therapy
- There is no treatment for [disease name]; the mainstay of therapy is supportive care.
- The mainstay of therapy for [disease name] is [medical therapy 1] and [medical therapy 2].
- [Medical therapy 1] acts by [mechanism of action 1].
- Response to [medical therapy 1] can be monitored with [test/physical finding/imaging] every [frequency/duration].
Surgery
- Surgery is the mainstay of therapy for [disease name].
- [Surgical procedure] in conjunction with [chemotherapy/radiation] is the most common approach to the treatment of [disease name].
- [Surgical procedure] can only be performed for patients with [disease stage] [disease name].
Prevention
- There are no primary preventive measures available for [disease name].
- Effective measures for the primary prevention of [disease name] include [measure1], [measure2], and [measure3].
- Once diagnosed and successfully treated, patients with [disease name] are followed-up every [duration]. Follow-up testing includes [test 1], [test 2], and [test 3].
References
- ↑ . doi:10.3978/j.issn.2072-1439.2014.01.27. Missing or empty
|title=(help)