Bronchiolitis medical therapy: Difference between revisions
m (Bot: Removing from Primary care) |
|||
| (68 intermediate revisions by 15 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{CMG}} | |||
{{CMG}}; {{AE}} {{Alonso}} | |||
{{Bronchiolitis}} | {{Bronchiolitis}} | ||
== | ==Overview== | ||
The primary mode of treatment for bronchiolitis is supportive management. Supportive therapy includes frequent, small feeding and [[oxygen therapy]]. In severe cases, [[infants]] may require [[intravenous fluids]] and food via a [[Nasogastric tube|nasogastric tube]]. In severe cases, [[mechanical ventilation]] or the use of [[continuous positive airway pressure]] ([[CPAP]]) might be necessary. [[Prophylaxis]] is indicated in [[infants]] with [[hemodynamically]] significant [[heart disease]] and [[Premature birth|preterm infants]] who require >21% [[oxygen]] for at least the first 28 days of life. The drug of choice for [[prophylaxis]] is [[palivizumab]]. | |||
==Medical Therapy== | |||
Recommendations for the treatment of bronchiolitis are based on the 2006 American Academy of Pediatrics Practice Guidelines for the Diagnosis and Management of Bronchiolitis.<ref name="pmid17015575">{{cite journal| author=American Academy of Pediatrics Subcommittee on Diagnosis and Management of Bronchiolitis| title=Diagnosis and management of bronchiolitis. | journal=Pediatrics | year= 2006 | volume= 118 | issue= 4 | pages= 1774-93 | pmid=17015575 | doi=10.1542/peds.2006-2223 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17015575 }} </ref><ref name="pmid25349312">{{cite journal| author=Ralston SL, Lieberthal AS, Meissner HC, Alverson BK, Baley JE, Gadomski AM et al.| title=Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. | journal=Pediatrics | year= 2014 | volume= 134 | issue= 5 | pages= e1474-502 | pmid=25349312 | doi=10.1542/peds.2014-2742 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25349312 }} </ref> | |||
== | ===Prophylaxis=== | ||
*Indications for prophylaxis: | |||
**The first year of life during [[RSV]] season in infants with hemodynamically significant [[heart disease]]. | |||
**The first year of life during [[RSV]] season in preterm infants < 32 weeks 0 days gestation who require > 21% oxygen for at least the first 28 days of life. | |||
* Preferred regimen: [[Palivizumab]] 15 mg/kg IM monthly for 5 months. | |||
===Oxygen | ===Oxygen Therapy=== | ||
* | *Supplemental [[oxygen therapy]] must be used to maintain [[oxygen saturation]] above (SpO<sub>2</sub>) 90% in patients with previous normal SpO<sub>2</sub>. | ||
*It is recommended to closely monitor | :*Infants with persistent [[respiratory distress]] who do not respond to supplemental [[oxygen therapy]] should be treated with nasal [[continuous positive airway pressure]] (CPAP) or tracheal intubation.<ref name="pmid19209271">{{cite journal| author=Wright M, Mullett CJ, Piedimonte G| title=Pharmacological management of acute bronchiolitis. | journal=Ther Clin Risk Manag | year= 2008 | volume= 4 | issue= 5 | pages= 895-903 | pmid=19209271 | doi= | pmc=PMC2621418 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19209271 }} </ref> | ||
*It is strongly recommended | *It is recommended to closely monitor SpO<sub>2</sub> if the patient's clinical status does not improve. | ||
*It is strongly recommended to closely monitor SpO<sub>2</sub> while gradually decreasing [[oxygen therapy]] in high-risk patients ([[congenital heart disease]] with significant hemodynamic changes, [[COPD|chronic lung disease]], or [[premature infants]]). | |||
=== | ===Bronchodilators=== | ||
*There is no evidence that supports the routine use of | *There is no evidence that supports the routine use of [[bronchodilators]] for bronchiolitis. | ||
*Benefits were observed in outpatient trials, | :*Several clinical trials have been performed to assess the efficacy of [[albuterol]] treatment, which did not demonstrate significant changes in the course of the [[disease]]. | ||
*Avoid the use of anticholinergic agents or | :*The use of racemic [[epinephrine]] has not been demonstrated to be effective for the long term improvement of the disease; however, one RCT showed improvement in the SpO<sub>2</sub> in the first hour after [[nebulization]].<ref name="pmid8285776">{{cite journal| author=Kristjánsson S, Lødrup Carlsen KC, Wennergren G, Strannegård IL, Carlsen KH| title=Nebulised racemic adrenaline in the treatment of acute bronchiolitis in infants and toddlers. | journal=Arch Dis Child | year= 1993 | volume= 69 | issue= 6 | pages= 650-4 | pmid=8285776 | doi= | pmc=PMC1029646 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8285776 }} </ref> | ||
:*One study proved that [[Nebulization|nebulized]] l-[[epinephrine]] is more effective than [[albuterol]] to prevent hospitalization in patients with [[bronchiolitis]].<ref name="pmid11435244">{{cite journal| author=Numa AH, Williams GD, Dakin CJ| title=The effect of nebulized epinephrine on respiratory mechanics and gas exchange in bronchiolitis. | journal=Am J Respir Crit Care Med | year= 2001 | volume= 164 | issue= 1 | pages= 86-91 | pmid=11435244 | doi=10.1164/ajrccm.164.1.2008090 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11435244 }} </ref> | |||
*Benefits were observed only in outpatient trials, the use of [[Bronchodilators]] did not show improvements in hospitalized patients regarding the length of stay or duration of the illness. | |||
*Avoid the use of [[anticholinergic]] agents or [[leukotriene]] inhibitors, as there is no evidence that proves their benefit. | |||
===Corticosteroids=== | ===Corticosteroids=== | ||
* | *Regular use of [[corticosteroids]] (either systemic or inhaled) is not recommended, as clinical trials have shown no benefit in the length of stay, [[Oxygen saturation|blood oxygen saturation]] level, [[respiratory rate]] or revisit and readmission. | ||
*Special cases, such as patients with family history of [[asthma]] or [[atopy]] and/or previous [[atopic dermatitis]], could benefit from the use of [[corticosteroid]] therapy.<ref name="pmid19209271">{{cite journal| author=Wright M, Mullett CJ, Piedimonte G| title=Pharmacological management of acute bronchiolitis. | journal=Ther Clin Risk Manag | year= 2008 | volume= 4 | issue= 5 | pages= 895-903 | pmid=19209271 | doi= | pmc=PMC2621418 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19209271 }} </ref> | |||
===Antiviral | ===Antiviral Therapy=== | ||
* | *[[Ribavirin]] should not be used regularly for the treatment of bronchiolitis. Several RCTs (randomized control trials) have demonstrated that the use of [[ribavirin]] does not improve the course of the disease or reduce the need for [[oxygen therapy]] or length of stay. | ||
*Patients with severe disease or risk of severe disease (immunocompromised patients and patients with | *Patients with severe disease or risk of severe disease ([[immunocompromised]] patients and patients with [[congenital heart disease]] with significant hemodynamic changes or [[COPD|chronic lung disease]]) may benefit from the use of [[ribavirin]]. | ||
=== | ===Antibiotic Therapy=== | ||
*RCT showed no benefit in antibiotic treatment for | *Randomized clinical trials (RCT) showed no benefit in [[antibiotic treatment]] for bronchiolitis if there is no concomitant [[bacterial infection]]. | ||
* | *[[Urinary tract infection]] and [[Otitis media classification#Acute Otitis Media|acute otitis media]] ([[AOM]]) are the most common causes of secondary [[bacterial infections]] in patients with bronchiolitis. The treatment for [[bacterial infections]] should not differ in patients with bronchiolitis than in those without bronchiolitis. | ||
*[[Otitis media classification#Acute Otitis Media|Acute otitis media]] is a common [[infection]] associated with bronchiolitis. Though [[RSV]] can cause [[AOM]], clinical findings are usually similar to those in bacterial infections; therefore it should be managed as a [[bacterial infection]]. Click [[Otitis media medical therapy#Acute Otitis Media|here]] for a complete therapeutic approach to [[AOM]]. | |||
*Acute otitis media is a common infection associated with | |||
===Fluid Therapy=== | |||
| | *[[Hydration]] and [[ingestion]] capacity of [[oral]] [[fluids]] must be evaluated in order to determine the need for [[Hydration|intravenous hydration]]. | ||
*[[Fluid]] therapy should be restricted to patients who present with signs of severe [[respiratory distress]] (60-70 breaths per minute, [[intercostal]] [[retraction]], [[sternal]] retraction and/or prolonged [[Wheezing|expiratory wheezing]]), as these patients will have increased risk of food [[aspiration]]. | |||
*[[Fever]] and [[tachypnea]] increase the insensible losses; therefore, IV fluid therapy must be calculated accordingly.<ref name="pmid19209271">{{cite journal| author=Wright M, Mullett CJ, Piedimonte G| title=Pharmacological management of acute bronchiolitis. | journal=Ther Clin Risk Manag | year= 2008 | volume= 4 | issue= 5 | pages= 895-903 | pmid=19209271 | doi= | pmc=PMC2621418 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19209271 }} </ref> | |||
</ | |||
===Respiratory Physical Therapy=== | |||
*It has been demonstrated that the use of respiratory physical therapy doesn't improve clinical signs or symptoms in patients with bronchiolitis. | |||
*Nasal clearance could produce temporary relief; however, deep [[pharynx]] [[aspiration]] has not shown efficacy in relieving signs and symptoms. | |||
* | |||
* | |||
=== | ===Hypertonic Saline=== | ||
* | * Nebulized hypertonic [[saline]] (HS) may reduce the length of stay among inpatients (see [http://www.wikidoc.org/index.php/File:Nebulised_hypertonic_saline_solution_for_reducing_length_of_stay_in_acute_bronchiolitis_in_children.png Forest plot]).<ref>GitHub Contributors. Hypertonic Saline for Bronchiolitis: a living systematic review. GitHub. Available at http://openmetaanalysis.github.io/Hypertonic-Saline-for-Bronchiolitis/. Accessed November 20, 2014.</ref> However, the quality of evidence is low due to the imprecision of results and the substantial heterogeneity or inconsistency of results. | ||
* Nebulized hypertonic [[saline]] may reduce the rate of admission among outpatients according to a [[systematic review]]. In this review, the relative risk reduction from hypertonic [[saline]] was 0.77. In populations similar to those in this review which had a rate of admission of 25% without treatment, the number needed to treat is 14. However, the quality of evidence is low due to imprecision of results and likely publication bias. (see [http://www.wikidoc.org/index.php/File:Nebulised_hypertonic_saline_solution_for_reducing_length_of_stay_in_acute_bronchiolitis_in_children.png Forest plot])<ref>openMetaAnalysis Contributors. Hypertonic Saline for Bronchiolitis: a living systematic review. GitHub. Available at http://openmetaanalysis.github.io/Hypertonic-Saline-for-Bronchiolitis/. Accessed November 20, 2014.</ref> | |||
* Shown below is the Forest plot depicting the different trials that evaluated the administration of nebulized hypertonic [[saline]] solution for the reduction of length of stay in acute bronchiolitis among children. | |||
[[Image:Nebulised_hypertonic_saline_solution_for_reducing_length_of_stay_in_acute_bronchiolitis_in_children.png|left|500px]] | |||
* <br style="clear:left" />Shown below is the Forest plot depicting the different trials that evaluated the administration of nebulized hypertonic [[saline]] solution for the reduction of the rate of hospitalization in acute bronchiolitis among children. | |||
[[Image:Nebulised_hypertonic_saline_solution_for_reducing_rate_of_hospitalization_in_acute_bronchiolitis_in_children.png|left|500px]] | |||
<br style="clear:left" /> | |||
===Pulmonary Surfactant=== | |||
*[[Pulmonary surfactant]] has been proven to contain [[protein]] components [[Pulmonary surfactant#Proteins|A]] and [[Pulmonary surfactant#Proteins|D]], which enhance the elimination of [[viruses]] and [[bacteria]] by the [[immune system]].<ref name="pmid19209271">{{cite journal| author=Wright M, Mullett CJ, Piedimonte G| title=Pharmacological management of acute bronchiolitis. | journal=Ther Clin Risk Manag | year= 2008 | volume= 4 | issue= 5 | pages= 895-903 | pmid=19209271 | doi= | pmc=PMC2621418 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19209271 }} </ref> | |||
*[[Pulmonary surfactant#Proteins|Protein D]] is related to the production of [[free radicals]] by the [[Macrophage|macrophages]] in the [[alveoli]]. | |||
: | *A meta-analysis demonstrated a significant reduction in duration of [[ICU]] stay and in the need for [[mechanical ventilation]] with the use of [[surfactant]] against a [[placebo]] or non-[[surfactant]] in patients using [[Mechanical ventilation|mechanical ventilators]] due to [[viral]] bronchiolitis.<ref name="pmid16856080">{{cite journal| author=Ventre K, Haroon M, Davison C| title=Surfactant therapy for bronchiolitis in critically ill infants. | journal=Cochrane Database Syst Rev | year= 2006 | volume= | issue= 3 | pages= CD005150 | pmid=16856080 | doi=10.1002/14651858.CD005150.pub2 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16856080 }} </ref> | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category: | {{WikiDoc Help Menu}} | ||
[[Category: | {{WikiDoc Sources}} | ||
[[Category: | |||
[[Category:Disease]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Pulmonology]] | |||
[[Category:Pediatrics]] | [[Category:Pediatrics]] | ||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
[[Category:Infectious disease]] | |||
Latest revision as of 20:44, 29 July 2020
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alonso Alvarado, M.D. [2]
|
Bronchiolitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Bronchiolitis medical therapy On the Web |
|
American Roentgen Ray Society Images of Bronchiolitis medical therapy |
|
Risk calculators and risk factors for Bronchiolitis medical therapy |
Overview
The primary mode of treatment for bronchiolitis is supportive management. Supportive therapy includes frequent, small feeding and oxygen therapy. In severe cases, infants may require intravenous fluids and food via a nasogastric tube. In severe cases, mechanical ventilation or the use of continuous positive airway pressure (CPAP) might be necessary. Prophylaxis is indicated in infants with hemodynamically significant heart disease and preterm infants who require >21% oxygen for at least the first 28 days of life. The drug of choice for prophylaxis is palivizumab.
Medical Therapy
Recommendations for the treatment of bronchiolitis are based on the 2006 American Academy of Pediatrics Practice Guidelines for the Diagnosis and Management of Bronchiolitis.[1][2]
Prophylaxis
- Indications for prophylaxis:
- The first year of life during RSV season in infants with hemodynamically significant heart disease.
- The first year of life during RSV season in preterm infants < 32 weeks 0 days gestation who require > 21% oxygen for at least the first 28 days of life.
- Preferred regimen: Palivizumab 15 mg/kg IM monthly for 5 months.
Oxygen Therapy
- Supplemental oxygen therapy must be used to maintain oxygen saturation above (SpO2) 90% in patients with previous normal SpO2.
- Infants with persistent respiratory distress who do not respond to supplemental oxygen therapy should be treated with nasal continuous positive airway pressure (CPAP) or tracheal intubation.[3]
- It is recommended to closely monitor SpO2 if the patient's clinical status does not improve.
- It is strongly recommended to closely monitor SpO2 while gradually decreasing oxygen therapy in high-risk patients (congenital heart disease with significant hemodynamic changes, chronic lung disease, or premature infants).
Bronchodilators
- There is no evidence that supports the routine use of bronchodilators for bronchiolitis.
- Several clinical trials have been performed to assess the efficacy of albuterol treatment, which did not demonstrate significant changes in the course of the disease.
- The use of racemic epinephrine has not been demonstrated to be effective for the long term improvement of the disease; however, one RCT showed improvement in the SpO2 in the first hour after nebulization.[4]
- One study proved that nebulized l-epinephrine is more effective than albuterol to prevent hospitalization in patients with bronchiolitis.[5]
- Benefits were observed only in outpatient trials, the use of Bronchodilators did not show improvements in hospitalized patients regarding the length of stay or duration of the illness.
- Avoid the use of anticholinergic agents or leukotriene inhibitors, as there is no evidence that proves their benefit.
Corticosteroids
- Regular use of corticosteroids (either systemic or inhaled) is not recommended, as clinical trials have shown no benefit in the length of stay, blood oxygen saturation level, respiratory rate or revisit and readmission.
- Special cases, such as patients with family history of asthma or atopy and/or previous atopic dermatitis, could benefit from the use of corticosteroid therapy.[3]
Antiviral Therapy
- Ribavirin should not be used regularly for the treatment of bronchiolitis. Several RCTs (randomized control trials) have demonstrated that the use of ribavirin does not improve the course of the disease or reduce the need for oxygen therapy or length of stay.
- Patients with severe disease or risk of severe disease (immunocompromised patients and patients with congenital heart disease with significant hemodynamic changes or chronic lung disease) may benefit from the use of ribavirin.
Antibiotic Therapy
- Randomized clinical trials (RCT) showed no benefit in antibiotic treatment for bronchiolitis if there is no concomitant bacterial infection.
- Urinary tract infection and acute otitis media (AOM) are the most common causes of secondary bacterial infections in patients with bronchiolitis. The treatment for bacterial infections should not differ in patients with bronchiolitis than in those without bronchiolitis.
- Acute otitis media is a common infection associated with bronchiolitis. Though RSV can cause AOM, clinical findings are usually similar to those in bacterial infections; therefore it should be managed as a bacterial infection. Click here for a complete therapeutic approach to AOM.
Fluid Therapy
- Hydration and ingestion capacity of oral fluids must be evaluated in order to determine the need for intravenous hydration.
- Fluid therapy should be restricted to patients who present with signs of severe respiratory distress (60-70 breaths per minute, intercostal retraction, sternal retraction and/or prolonged expiratory wheezing), as these patients will have increased risk of food aspiration.
- Fever and tachypnea increase the insensible losses; therefore, IV fluid therapy must be calculated accordingly.[3]
Respiratory Physical Therapy
- It has been demonstrated that the use of respiratory physical therapy doesn't improve clinical signs or symptoms in patients with bronchiolitis.
- Nasal clearance could produce temporary relief; however, deep pharynx aspiration has not shown efficacy in relieving signs and symptoms.
Hypertonic Saline
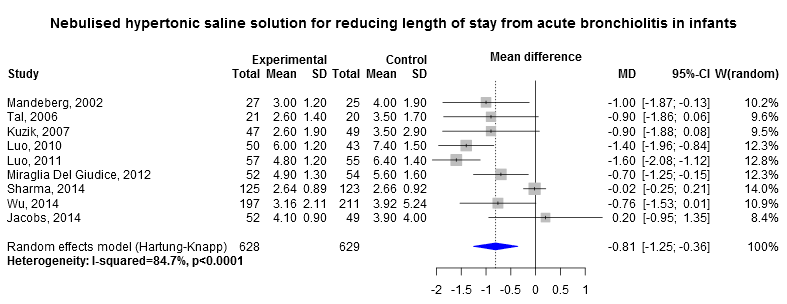
- Nebulized hypertonic saline (HS) may reduce the length of stay among inpatients (see Forest plot).[6] However, the quality of evidence is low due to the imprecision of results and the substantial heterogeneity or inconsistency of results.
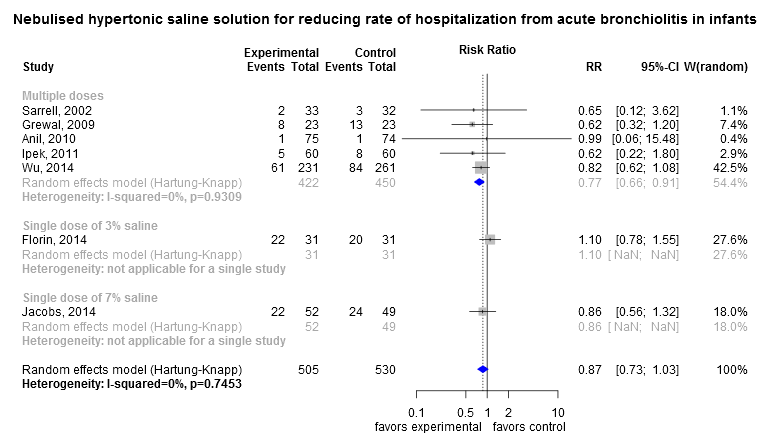
- Nebulized hypertonic saline may reduce the rate of admission among outpatients according to a systematic review. In this review, the relative risk reduction from hypertonic saline was 0.77. In populations similar to those in this review which had a rate of admission of 25% without treatment, the number needed to treat is 14. However, the quality of evidence is low due to imprecision of results and likely publication bias. (see Forest plot)[7]
- Shown below is the Forest plot depicting the different trials that evaluated the administration of nebulized hypertonic saline solution for the reduction of length of stay in acute bronchiolitis among children.
Shown below is the Forest plot depicting the different trials that evaluated the administration of nebulized hypertonic saline solution for the reduction of the rate of hospitalization in acute bronchiolitis among children.
Pulmonary Surfactant
- Pulmonary surfactant has been proven to contain protein components A and D, which enhance the elimination of viruses and bacteria by the immune system.[3]
- Protein D is related to the production of free radicals by the macrophages in the alveoli.
- A meta-analysis demonstrated a significant reduction in duration of ICU stay and in the need for mechanical ventilation with the use of surfactant against a placebo or non-surfactant in patients using mechanical ventilators due to viral bronchiolitis.[8]
References
- ↑ American Academy of Pediatrics Subcommittee on Diagnosis and Management of Bronchiolitis (2006). "Diagnosis and management of bronchiolitis". Pediatrics. 118 (4): 1774–93. doi:10.1542/peds.2006-2223. PMID 17015575.
- ↑ Ralston SL, Lieberthal AS, Meissner HC, Alverson BK, Baley JE, Gadomski AM; et al. (2014). "Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis". Pediatrics. 134 (5): e1474–502. doi:10.1542/peds.2014-2742. PMID 25349312.
- ↑ 3.0 3.1 3.2 3.3 Wright M, Mullett CJ, Piedimonte G (2008). "Pharmacological management of acute bronchiolitis". Ther Clin Risk Manag. 4 (5): 895–903. PMC 2621418. PMID 19209271.
- ↑ Kristjánsson S, Lødrup Carlsen KC, Wennergren G, Strannegård IL, Carlsen KH (1993). "Nebulised racemic adrenaline in the treatment of acute bronchiolitis in infants and toddlers". Arch Dis Child. 69 (6): 650–4. PMC 1029646. PMID 8285776.
- ↑ Numa AH, Williams GD, Dakin CJ (2001). "The effect of nebulized epinephrine on respiratory mechanics and gas exchange in bronchiolitis". Am J Respir Crit Care Med. 164 (1): 86–91. doi:10.1164/ajrccm.164.1.2008090. PMID 11435244.
- ↑ GitHub Contributors. Hypertonic Saline for Bronchiolitis: a living systematic review. GitHub. Available at http://openmetaanalysis.github.io/Hypertonic-Saline-for-Bronchiolitis/. Accessed November 20, 2014.
- ↑ openMetaAnalysis Contributors. Hypertonic Saline for Bronchiolitis: a living systematic review. GitHub. Available at http://openmetaanalysis.github.io/Hypertonic-Saline-for-Bronchiolitis/. Accessed November 20, 2014.
- ↑ Ventre K, Haroon M, Davison C (2006). "Surfactant therapy for bronchiolitis in critically ill infants". Cochrane Database Syst Rev (3): CD005150. doi:10.1002/14651858.CD005150.pub2. PMID 16856080.