Benign paroxysmal positional vertigo: Difference between revisions
m (Bot: Automated text replacement (-{{SIB}} + & -{{EH}} + & -{{EJ}} + & -{{Editor Help}} + & -{{Editor Join}} +)) |
Minu Velan (talk | contribs) |
||
| Line 39: | Line 39: | ||
==Diagnosis== | ==Diagnosis== | ||
The condition is diagnosed by performing the Dix-Hallpike maneuver which is diagnostic for the condition. The test involves a reorientation of the head to align the posterior canal (at its entrance to the ampulla) with the direction of gravity. This test stimulus is effective in provoking the symptoms in subjects suffering from archetypal BPPV. These symptoms are typically a short lived [[Vertigo (medical)|vertigo]], and observed [[nystagmus]]. | The condition is diagnosed by performing the Dix-Hallpike maneuver which is diagnostic for the condition. The test involves a reorientation of the head to align the posterior canal (at its entrance to the ampulla) with the direction of gravity. This test stimulus is effective in provoking the symptoms in subjects suffering from archetypal BPPV. These symptoms are typically a short lived [[Vertigo (medical)|vertigo]], and observed [[nystagmus]]. | ||
Dix-Hallpike Maneuver-Done by direct observation of eye movement or by using video goggles. Describe the test to patient. Ask patient to sit on the examination table, turn patient's head to 45 degree to the right side and check for nystagmus. Ask patient to lie down with head extended 45 degree and head extended below level of examination table or resting on examination table with 20 degree below horizontal using a pillow. Observe for nystagmus duration and character. If nystagmus present, it is BPPV on that side. After nystagmus disappeared, sit patient up, it should reverse when she sits. Repeat the test in the left side. | |||
==Treatment== | ==Treatment== | ||
Revision as of 11:12, 9 January 2015
| Benign paroxysmal positional vertigo | |
 | |
|---|---|
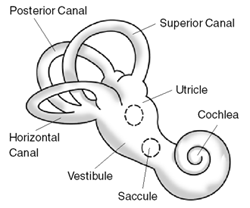
| Exterior of labyrinth. | |
| ICD-10 | H81.1 |
| ICD-9 | 386.11 |
| OMIM | 193007 |
| DiseasesDB | 1344 |
| eMedicine | ent/761 emerg/57 neuro/411 |
| MeSH | D014717 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Benign paroxysmal positional vertigo (BPPV) or "Benign paroxysmal vertigo" (BPV) is a condition caused by problems in the inner ear.
Cause
Within the labyrinth of the inner ear lie collections of calcium crystals known as otoconia. In patients, the otoconia are dislodged from their usual position within the utricle and they migrate over time into one of the semicircular canals (the posterior canal is most commonly affected due to its anatomical position). When the head is reoriented relative to gravity, the gravity-dependent movement of the heavier otoconial debris within the affected semicircular canal causes abnormal (pathological) fluid endolymph displacement and a resultant sensation of vertigo. This more common condition is known as canalithiasis.
In rare cases, the crystals themselves can adhere to a semicircular canal cupula rendering it heavier than the surrounding endolymph. Upon reorientation of the head relative to gravity, the cupula is weighted down by the dense particles thereby inducing an immediate and maintained excitation of semicircular canal afferents afferent nerve. This condition is termed cupulolithiasis.
Presentation
The primary symptom is the sudden onset of severe vertigo and nystagmus that occurs exclusively with head movement in the direction of the affected ear.
Patients often describe their first experience occurring while turning their head in bed.
The vertigo is brief in duration — 5 seconds to 30 seconds.
It is often associated with nausea.
Patients do not experience other neurological deficits such as numbness or weakness, and if these symptoms are present, a more concerning etiology such as posterior circulation stroke, must be considered.
Diagnosis
The condition is diagnosed by performing the Dix-Hallpike maneuver which is diagnostic for the condition. The test involves a reorientation of the head to align the posterior canal (at its entrance to the ampulla) with the direction of gravity. This test stimulus is effective in provoking the symptoms in subjects suffering from archetypal BPPV. These symptoms are typically a short lived vertigo, and observed nystagmus. Dix-Hallpike Maneuver-Done by direct observation of eye movement or by using video goggles. Describe the test to patient. Ask patient to sit on the examination table, turn patient's head to 45 degree to the right side and check for nystagmus. Ask patient to lie down with head extended 45 degree and head extended below level of examination table or resting on examination table with 20 degree below horizontal using a pillow. Observe for nystagmus duration and character. If nystagmus present, it is BPPV on that side. After nystagmus disappeared, sit patient up, it should reverse when she sits. Repeat the test in the left side.
Treatment
The treatment of choice for this condition is the Epley canalith repositional maneuver which is effective in approximately 80% of patients[2]. The treatment employs gravity to move the calcium build-up that causes the condition).[1] The particle repositioning maneuver (Epley Maneuver) can be performed during a clinic visit by specially trained otolaryngologists, neurologists, chiropractors, physical therapists, or audiologists. The maneuver is relatively simple but few general health practitioners know how to perform it.
Treatment may also be achieved with the use of a device such as "The DizzyFIX", a device that enables patients and health practitioners to guide themselves through the particle repositioning maneuver[3]. The maneuver can be conducted at home and repeated as often as needed. Other devices, such as a head over heels "rotational chair", are also available at some tertiary care centers [2]
The Epley maneuver (particle repositioning) does not address the actual presence of the particles (otoconia), rather it changes their location. The maneuver moves these particles from areas in the inner ear which cause symptoms, such as vertigo, and repositions them into areas where they do not cause these problems.
Meclizine is a commonly prescribed medication, but is ultimately ineffective for this condition, other than masking the dizziness. Other sedative medications help mask the symptoms associated with BPPV but do not affect the disease process or resolution rate. Serc is available in some countries and is commonly prescribed but again it is likely ineffective. Particle repositioning remains the current gold standard treatment for most cases of BPPV.
Surgical treatments, such as a semi-circular canal occlusion, do exist for BPPV but carry the same risk as any neurosurgical procedure. Surgery is reserved for severe and persistent cases which fail particle repositioning and medical therapy.
See also
References
- ↑ von Brevern M, Seelig T, Radtke A; et al. (2006). "Short-term efficacy of Epley's maneuver: a double-blind randomised trial". J Neurol Neurosurg Psychiatr. 77: 980&ndash, 82.
- ↑ Furman JM, Cass SP, Briggs BC. (1998). "Treatment of benign positional vertigo
using heels-over-head rotation". Ann Otol Rhinol Laryngol. 107:: 1046&ndash, 53. line feed character in
|title=at position 39 (help)
External links
- VEDA Vestibular Disorder Association webpage concerning BPPV
- MayoClinic
- UCSD
- Biomechanical Modeling and Simulations
- Chicago Dizziness and Hearing
- BPPV Test Complete an on-line Dizziness Handicap Inventory (DHI)
- Dizzytimes.com Online Community for Sufferers of Vertigo and Dizziness
Template:Diseases of the ear and mastoid process
de:Benigner paroxysmaler Lagerungsschwindel no:Benign paroksysmal posisjonsvertigo