Bell's palsy
| Bell's palsy | |
 | |
|---|---|
| ICD-10 | G51.0 |
| ICD-9 | 351.0 |
| DiseasesDB | 1303 |
| MedlinePlus | 000773 |
| eMedicine | emerg/56 |
| MeSH | D020330 |
|
WikiDoc Resources for Bell's palsy |
|
Articles |
|---|
|
Most recent articles on Bell's palsy Most cited articles on Bell's palsy |
|
Media |
|
Powerpoint slides on Bell's palsy |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Bell's palsy at Clinical Trials.gov Clinical Trials on Bell's palsy at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Bell's palsy
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Bell's palsy Discussion groups on Bell's palsy Patient Handouts on Bell's palsy Directions to Hospitals Treating Bell's palsy Risk calculators and risk factors for Bell's palsy
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Bell's palsy |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For patient information click here
Editor-in-Chief: Gilbert Dagher, M.D.
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [1] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
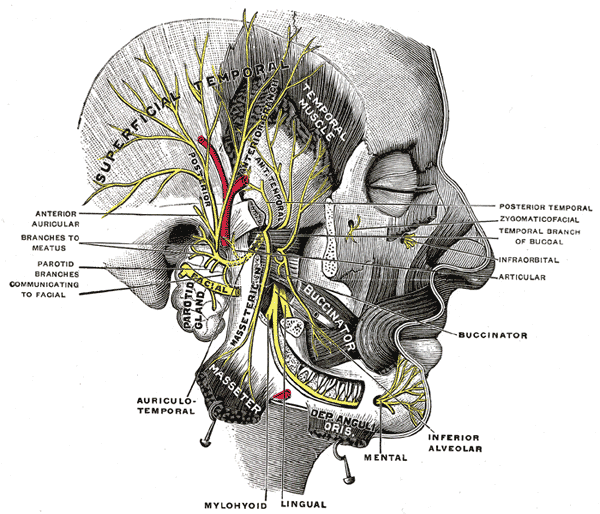
Bell's palsy (or facial palsy) is characterised by facial drooping on the affected half, due to malfunction of the facial nerve (VII cranial nerve), which controls the muscles of the face. Named after Scottish anatomist Charles Bell, who first described it, Bell's palsy is the most common acute mononeuropathy (disease involving only one nerve), and is the most common cause of acute facial nerve paralysis. The paralysis is of the infranuclear/lower motor neuron type. Bell’s palsy affects about 40,000 people in the United States every year. It affects approximately 1 person in 65 during a lifetime. Until recently, its cause was unknown in most cases, but it has now been related to both Lyme disease and Herpes Zoster.
Epidemiology
The annual incidence rate of Bell's Palsy is between 13 and 34 cases per 100,000 population. There is no race, geographic, or gender predilection. The risk is three times greater during pregnancy, especially in the third trimester or in the first postpartum week. Its is to note that diabetes is present in about 5 to 10 percent of patients.
Etiology
Many cases are likely due to Herpes Simplex Virus (HSV) reactivation
Infectious causes
- Herpes simplex virus activation is the likely cause of Bell's Palsy in most cases.
- Herpes Zoster may be the second most common associated viral infection.
- Cytomegalovirus
- Epstein Barr virus
- Adenovirus
- Rubella virus
- Mumps
- Influenza B
- Coxsackievirus
- Rickettsial infection
- Ehrlichiosis
Non-infectious causes
- Inactivated intranasal influenza vaccine that was introduced and since withdrawn from the market in Switzerland
- Genetic predisposition in some cases
- Ischemia of the facial nerve
- Tumors and compression of the facial nerve
- Temporal bone fracture
- Systemic Lupus Erythematosus (SLE)
- Sarcoidosis
Histopathology
- The facial nerve has a thickened, edematous perineurium with a diffuse infiltrate of inflammatory cells between nerve bundles and around intraneural blood vessels.
- The appearance similar to that found with Herpes Zoster infection, consistent with an inflammatory and possibly an infectious cause
Peripheral versus central lesions
- Sparing of the forehead muscles is suggestive of a central (upper motor neuron) lesion because of bilateral innervation to this area.
- However, it does not exclude a peripheral site of pathology in all cases.
History and Symptoms
Sudden onset, usually over hours, of unilateral facial paralysis(maximal symptoms by 48 hours)
- Eyebrow sagging with inability to close the affected eye
- Nasolabial fold flattening with mouth drawn to the non affected side
- Inability to wrinkle forehead (peripheral lesion)
- May be associated with ear pain, impaired taste sensation on the anterior two-thirds of the tongue, decreased tearing, and hyperacusis
Diagnostic Tests
- Electrodiagnostic studies help determine the prognosis, and imaging studies can define potential surgical causes of facial palsy.
- These tests are not necessary in all patients.
- Patients with a typical lesion that is incomplete and recovers do not need further study.
- Electrodiagnostic studies (EMG, or motor nerve conduction study) and Imaging (CT, or MRI) are warranted if the physical signs are atypical, there is slow progression beyond three weeks, or if there is no improvement at six months.
- Screening blood studies for underlying systemic disease or infection should also be considered in these cases.
- No test provides prognostic information sufficiently early as to be used for determining who should or should not be treated
Differential Diagnosis
Lyme Disease
- Facial nerve palsy is the most common cranial neuropathy associated with Lyme meningitis.
- Screening for antibodies to B.burgdorferi not recommended among patients with seventh nerve palsy with no additional manifestations of Lyme disease.
- Findings suggestive of possible Lyme disease include the development of facial palsy in a young patient, heart block, arthritis, vertigo, and hearing loss.
HIV
- HIV infection rarely causes facial palsy.
- Onset at the time of sero-conversion when a CSF lymphocytosis is usually present.
- In the later stages when cellular immunity wanes, the facial palsy is typically due to another infection such as Zoster, chronic demyelinating polyradiculopathy, or meningeal lymphomatosis.
Melkersson-Rosenthal Syndrome
- Facial paralysis, episodic facial swelling, and a fissured tongue, typically beginning in adolescence, with recurrent episodes of facial palsy.
- Incomplete forms of this syndrome outnumber those with the classic triad.
- The cause is unknown, and treatment unproven.
Other Entities
- Bacterial infection of the middle ear (otitis media)
- Cholesteatoma, or tumors should be suspected if the onset of facial palsy is gradual.
- Sarcoidosis, especially in patients with bilateral facial palsy.
- Sjogren's syndrome is an unusual cause.
Risk Stratification and Prognosis
- The House-Brackmann grading system was devised both as a clinical indicator of severity and also an objective record of progress.
- Clinically incomplete lesions tend to recover.
- The natural history without treatment was described in a study of 1011 patients in 1982:
-67% had incomplete paralysis, with 94% rate of return to normal function -33% had complete paralysis, with 60% rate of return to normal function -By 3 weeks, 71% had complete recovery, 13% had slight sequelae , and 16% had residual weakness
- Herpes zoster is associated with more severe paresis and worse prognosis compared with "idiopathic" Bell's palsy.
- There is a favorable prognosis if some recovery is seen within the first 21 days of onset.
- In severe lesions that recover, the outgrowth of new axons from the injury site may be disorganized and misdirected.
- On blinking there is twitching of the angle of the mouth, and on smiling the eye may close or wink.
- With misdirected autonomic fibers, a salivary stimulus may result in excess lacrimation, the syndrome of "crocodile tears."
- Recurrent attacks of on either the ipsilateral or contralateral side have been observed in 7 to 15% of patients.
Treatment
Eye care
In severe cases, the cornea may be at risk because of poor eyelid closure and reduced tearing, which may result in drying and abrasion.
- The risk for blindness due to corneal trauma is significant, especially if there is 5th nerve concomitant damage.
- The use of artificial tears, every hour while awake, and ophthalmic ointments at night is recommeneded.
- Protective glasses or goggles during the day.
- Patches can be used at night, but tape should not be placed directly on the eyelid since the patch could slip and abrade the cornea.
- Rarely tarsorrhaphy or temporary implantation of a gold weight into the upper lid acn be used to close the eye and protect the cornea.
Glucocorticoid and Antiviral Therapy
The mainstay of pharmacologic therapy is early short-term oral glucocorticoid treatment
- It is established as effective by randomized controlled trials: Prednisone 1mg/kg up to 60mg PO daily for 10 days
- The suspicion that Bell's palsy is caused by herpes simplex virus in most patients led to trials of antiviral therapy
- Compared with placebo, these trials found no benefit for antiviral therapy alone.
- The data is conflicting with regard to the possibility of additional benefit when antiviral agents are administered with glucocorticoids.
- In a meta-analysis involving 18 trials and 2786 patients, treatment with glucocorticoids alone was associated with a reduced risk of unfavorable recovery (relative risk [RR] 0.69, 95% CI 0.55-0.87), while treatment with antiviral agents alone was not (RR 1.14, 95% CI 0.80-1.62).
- In a pooled data from eight trials, the same meta-analysis found a trend towards a reduced risk of unfavorable recovery for combined antiviral and glucocorticoid treatment compared with glucocorticoid treatment alone; however, the outcome barely missed statistical significance (RR 0.75, 95% CI 0.56-1.0).
- In a second meta-analysis of six trials and 1145 patients, there was no significant benefit of combined antiviral and glucocorticoid treatment for achieving at least partial facial muscle recovery (odds ratio 1.5, 95% CI 0.83-2.69).
- Neither excludes the possibility of marginal benefit when antiviral therapy is combined with glucocorticoids.
- Some authorities recommend antiviral therapy for severe complete lesions.
- Acyclovir 2000-4000 mg/24 h PO divided 5 times a day for 7-10 d
- Valcyclovir 1000-3000 mg/24 h PO for 5 d
Bell’s Palsy-induced Blepharospasm
Blepharospasm associated with Bell's palsy has been rarely reported
- So far, seven patients previously reported: all women.
- In five of the seven patients, blepharospasm appeared within a month after the onset of Bell’s palsy.
Possible mechanisms
- The majority of patients with blepharospasm have a high incidence of local ocular symptoms prior to or at the onset of blepharospasm, such as blepharitis, conjunctivitis, dry eyes or photophobia.
- Chronically disturbed sensory inputs to the central nervous system due to lagophthalmos and corneal irritation may contribute to the generation of blepharospasm.
- In patients with Bell’s palsy, there is an enhanced blink reflex secondary to inputs from the paralyzed side compared which those of the non-paralyzed side.
- Abnormal afferent input from the paralyzed side contributes to the abnormal sensitization of the blink reflex, thus facilitating the induction of abnormal facial motor outputs such as blepharospasm.
- It is unclear why Bell’s palsy-induced blepharospasm is extremely rare.
References
Additional Resources
- Sullivan FM, Swan IRC, Donnan PT, et al. Early treatment with prednisolone or acyclovir in Bell's palsy. N Engl J Med 2007;357:1598-1607.
- "The Merck Manual"
- New England Journal of Medicine, Sept. 2004
- Lambert, Michael. (2007-03-05) "Bell's Palsy." (Website.) Emedicine. Retrieved on 2007-09-27.
External links
- managment and treatment of facial paralysis
- Bell's Palsy Information Site, has a FAQ
- Bell's Palsy and Pregnancy
- Bell's Palsy Patient Info - Neurology Channel
- Living with Facial Palsy, a site for parents of children with Facial Palsy
- Links to pictures of Bells palsy (Hardin MD/Univ of Iowa)
- Bell's Palsy Association
Template:SIB Template:PNS diseases of the nervous system
ar:شلل العصب الوجهي ca:Paràlisi de Bell de:Fazialislähmung nl:Aangezichtsverlamming van Bell fi:Bellin halvaus Template:WH Template:WikiDoc Sources