Babesiosis medical therapy: Difference between revisions
No edit summary |
No edit summary |
||
| Line 17: | Line 17: | ||
::* Note (1): For overwhelming infection in asplenic patients and immunocompromised patients, treat for 6 or more weeks. | ::* Note (1): For overwhelming infection in asplenic patients and immunocompromised patients, treat for 6 or more weeks. | ||
::* Note (2): Consider transfusion if 10% parasitemia. | ::* Note (2): Consider transfusion if 10% parasitemia. | ||
==The best way to remove a tick== | |||
#Use fine-tipped tweezers or notched tick extractor, and protect your fingers with a tissue, paper towel, or latex gloves. Persons should avoid removing ticks with bare hands. | |||
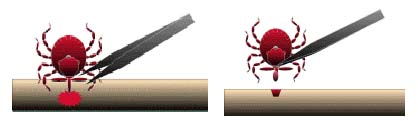
#Grasp the tick as close to the skin surface as possible and pull upward with steady, even pressure. Do not twist or jerk the tick; this may cause the mouthparts to break off and remain in the skin. (If this happens, remove mouthparts with tweezers. Consult your health care provider if illness occurs.) | |||
#After removing the tick, thoroughly disinfect the bite site and wash your hands with soap and water. | |||
[[Image:Tick removal process.jpg|250px|center|thumb|Tick removal process]] | |||
*Do not squeeze, crush, or puncture the body of the tick because its fluids may contain infectious organisms. Skin accidentally exposed to tick fluids can be disinfected with iodine scrub, rubbing alcohol, or water containing detergents. | |||
[[Image:Removal.jpg|250px|center|thumb|Removal of an embedded tick using fine-tipped tweezers]] | |||
*Save the tick for identification in case you become ill. This may help your doctor to make an accurate diagnosis. Place the tick in a sealable plastic bag and put it in your freezer. Write the date of the bite on a piece of paper with a pencil and place it in the bag. <ref name="Tick Removal CDC”> Tick Removal. Centers for Disease Control and Prevention (2015). http://www.cdc.gov/ticks/removing_a_tick.html Accessed on December 30, 2015</ref> | |||
==References== | ==References== | ||
Revision as of 17:26, 6 January 2016
|
Babesiosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Babesiosis medical therapy On the Web |
|
American Roentgen Ray Society Images of Babesiosis medical therapy |
|
Risk calculators and risk factors for Babesiosis medical therapy |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
The mainstay of therapy for babesiosis is antimicrobial therapy. Patients with mild or moderate disease are treated with a combination of Atovaquone and Azithromycin. Patients with severe disease are treated with either Clindamycin or Clindamycin and Quinine. In life-threatening cases, exchange transfusion is performed.
Medical Therapy
The traditional regimen of Quinine and Clindamycin is often poorly tolerated; recent evidence suggests that a regimen of Atovaquone and Azithromycin can be equally effective [1]. In life-threatening cases, exchange transfusion is performed. In this procedure, the infected red blood cells are removed and replaced with fresh ones.
Antimicrobial Regimen
- Treatment
- 1. Mild/moderate disease[2]
- Preferred regimen: Atovaquone 750 mg PO bid AND Azithromycin 600 mg PO qd for 7-10 days
- 2. Severe disease:
- Preferred regimen: Clindamycin 600 mg PO tid AND Quinine 650 mg PO tid for 7–10 days
- Preferred regimen: Clindamycin 1.2 g IV q12h
- Note (1): For overwhelming infection in asplenic patients and immunocompromised patients, treat for 6 or more weeks.
- Note (2): Consider transfusion if 10% parasitemia.
The best way to remove a tick
- Use fine-tipped tweezers or notched tick extractor, and protect your fingers with a tissue, paper towel, or latex gloves. Persons should avoid removing ticks with bare hands.
- Grasp the tick as close to the skin surface as possible and pull upward with steady, even pressure. Do not twist or jerk the tick; this may cause the mouthparts to break off and remain in the skin. (If this happens, remove mouthparts with tweezers. Consult your health care provider if illness occurs.)
- After removing the tick, thoroughly disinfect the bite site and wash your hands with soap and water.
- Do not squeeze, crush, or puncture the body of the tick because its fluids may contain infectious organisms. Skin accidentally exposed to tick fluids can be disinfected with iodine scrub, rubbing alcohol, or water containing detergents.

- Save the tick for identification in case you become ill. This may help your doctor to make an accurate diagnosis. Place the tick in a sealable plastic bag and put it in your freezer. Write the date of the bite on a piece of paper with a pencil and place it in the bag. [3]
References
- ↑ Krause P, Lepore T, Sikand V, Gadbaw J, Burke G, Telford S, Brassard P, Pearl D, Azlanzadeh J, Christianson D, McGrath D, Spielman A (2000). "Atovaquone and azithromycin for the treatment of babesiosis". N Engl J Med. 343 (20): 1454–8. PMID 11078770.
- ↑ Gilbert, David (2015). The Sanford guide to antimicrobial therapy. Sperryville, Va: Antimicrobial Therapy. ISBN 978-1930808843.
- ↑ Tick Removal. Centers for Disease Control and Prevention (2015). http://www.cdc.gov/ticks/removing_a_tick.html Accessed on December 30, 2015