Avelumab: Difference between revisions
No edit summary |
No edit summary |
||
| Line 351: | Line 351: | ||
|PK=(Description) | |PK=(Description) | ||
|nonClinToxic=(Description) | |nonClinToxic=(Description) | ||
|clinicalStudies====== | |clinicalStudies======Metastatic Merkel Cell Carcinoma===== | ||
( | *The efficacy and safety of BAVENCIO was demonstrated in the JAVELIN Merkel 200 trial (NCT02155647), an open-label, single-arm, multi-center study conducted in patients with histologically confirmed metastatic MCC whose disease had progressed on or after chemotherapy administered for distant metastatic disease. The trial excluded patients with autoimmune disease; medical conditions requiring systemic immunosuppression; prior organ or allogeneic stem cell transplantation; prior treatment with anti-PD-1, anti-PD-L1, or anti-CTLA-4 antibodies; CNS metastases; infection with HIV, hepatitis B, or hepatitis C; or ECOG performance score ≥ 2. | ||
*Patients received BAVENCIO 10 mg/kg as an intravenous infusion over 60 minutes every 2 weeks until disease progression or unacceptable toxicity. Patients with radiological disease progression not associated with significant clinical deterioration, defined as no new or worsening symptoms, no change in performance status for greater than 2 weeks, and no need for salvage therapy, could continue treatment. Tumor response assessments were performed every 6 weeks. The major efficacy outcome measures were confirmed overall response rate (ORR) according to Response Evaluation Criteria in Solid Tumors (RECIST) v1.1 as assessed by a blinded independent central review committee (IRC) and IRC-assessed duration of response. The efficacy analysis was conducted when the last patient enrolled had completed 12 months of follow-up. | |||
( | *A total of 88 patients were enrolled. Baseline patient characteristics were a median age of 73 years (range: 33 to 88), 74% of patients were male, 92% were White, and the ECOG performance score was 0 (56%) or 1 (44%). Seventy-five percent of patients were 65 years or older, 35% were 75 or older, and 3% were 85 or older. Sixty-five percent of patients were reported to have had one prior anti-cancer therapy for metastatic MCC and 35% had two or more prior therapies. Fifty-three percent of patients had visceral metastases. All patients had tumor samples evaluated for PD-L1 expression; of these, 66% were PD-L1-positive (≥ 1% of tumor cells), 18% were PD-L1 negative, and 16% had non-evaluable results by an investigational immunohistochemistry assay. Archival tumor samples were evaluated for Merkel cell polyomavirus (MCV) using an investigational assay; of the 77 patients with evaluable results, 52% had evidence of MCV. | ||
===== | *Efficacy results are presented in Table 6. Responses were observed in patients regardless of tumor PD-L1 expression or presence of MCV. | ||
[[image:Avelumab_Clinical_Studies_Table_1.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | |||
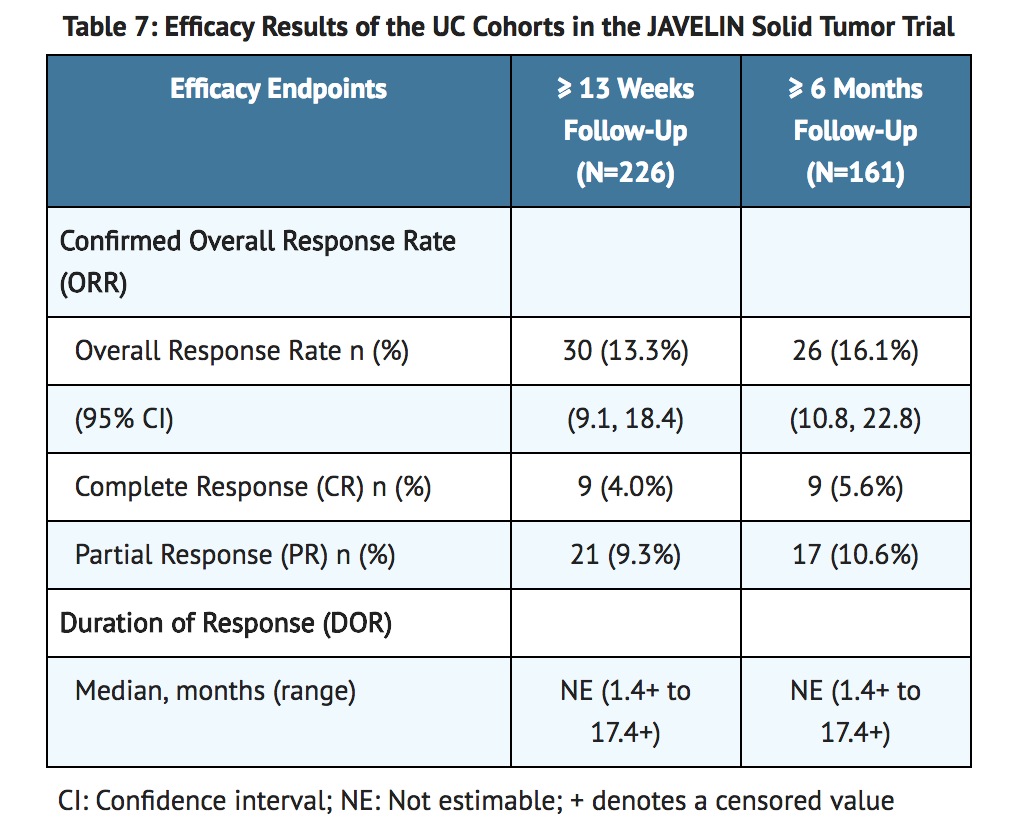
=====Locally Advanced or Metastatic Urothelial Carcinoma===== | |||
*The efficacy and safety of BAVENCIO was demonstrated in the UC cohorts of the JAVELIN Solid Tumor trial, an open-label, single-arm, multi-center study that included 242 patients with locally advanced or metastatic urothelial carcinoma (UC) with disease progression on or after platinum-containing chemotherapy or who had disease progression within 12 months of treatment with a platinum-containing neoadjuvant or adjuvant chemotherapy regimen. Patients with active or history of central nervous system metastasis; other malignancies within the last 5 years; organ transplant; conditions requiring therapeutic immune suppression; or active infection with HIV, hepatitis B, or hepatitis C were excluded. Patients with autoimmune disease, other than type 1 diabetes, vitiligo, psoriasis, or thyroid disease that did not require immunosuppressive treatment, were excluded. Patients were included regardless of their PD-L1 status. | |||
*Patients received BAVENCIO at a dose of 10 mg/kg intravenously every 2 weeks until radiographic or clinical progression or unacceptable toxicity. Tumor response assessments were performed every 6 weeks. Efficacy outcome measures included confirmed overall response rate (ORR), as assessed by an Independent Endpoint Review Committee (IERC) using Response Evaluation Criteria in Solid Tumors (RECIST) v1.1, and duration of response (DOR). Efficacy was evaluated in patients who were followed for a minimum of both 13 weeks and 6 months at the time of data cut-off. | |||
*Baseline demographic and disease characteristics for the 226 patients with a minimum of 13 weeks of follow-up were median age 68 years (range: 30 to 89), 72% male, 80% White, and 34% and 66% of patients had an ECOG performance status 0 and 1, respectively. Forty-four percent of patients had non-bladder urothelial carcinoma including 23% of patients with upper tract disease, and 83% of patients had visceral metastases (baseline target and/or non-target lesions present outside of the lymph nodes). Nine (4%) patients had disease progression following prior platinum-containing neoadjuvant or adjuvant therapy only. Forty-seven percent of patients only received prior cisplatin-based regimens, 32% received only prior carboplatin-based regimens, and 20% received both cisplatin and carboplatin-based regimens. At baseline, 17% of patients had a hemoglobin < 10 g/dL and 34% of patients had liver metastases. | |||
*Efficacy results are presented in Table 7. The median time to response was 2.0 months (range: 1.3 to 11.0) among patients followed for either ≥ 13 weeks or ≥ 6 months. Using a clinical trial assay to assess PD-L1 staining, with 16% of patients not evaluable, there were no clear differences in response rates based on PD-L1 tumor expression. Among the total 30 responding patients followed for ≥ 13 weeks, 22 patients (73%) had an ongoing response of 6 months or longer and 4 patients (13%) had ongoing responses of 12 months or longer. Among the total 26 responding patients followed for ≥ 6 months, 22 patients (85%) had ongoing responses of 6 months or longer and 4 patients (15%) had ongoing responses of 12 months or longer. | |||
[[image:Avelumab_Clinical_Studies_Table_2.png|none|thumb|400px|This image is provided by the National Library of Medicine.]] | |||
|howSupplied=*BAVENCIO (avelumab) Injection is a sterile, preservative-free, and clear, colorless to slightly yellow solution for intravenous infusion supplied as a single-dose vial of 200 mg/10 mL (20 mg/mL), individually packed into a carton (NDC 44087-3535-1). | |howSupplied=*BAVENCIO (avelumab) Injection is a sterile, preservative-free, and clear, colorless to slightly yellow solution for intravenous infusion supplied as a single-dose vial of 200 mg/10 mL (20 mg/mL), individually packed into a carton (NDC 44087-3535-1). | ||
Revision as of 16:12, 27 June 2018
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Yashasvi Aryaputra[2];
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Avelumab is a Acetylcholine release inhibitor, Adrenergic receptor agonist that is FDA approved for the (type of indication of drug) of a list of indications, separated by commas.. Common adverse reactions include a list of adverse reactions, separated by commas..
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Condition 1
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Condition 2
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Non–Guideline-Supported Use
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Condition 3
- Dosing Information
- (Dosage)
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
Condition 1
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Condition 2
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Non–Guideline-Supported Use
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Condition 3
- Dosing Information
- (Dosage)
Contraindications
- None
Warnings
Immune-Mediated Pneumonitis
- BAVENCIO can cause immune-mediated pneumonitis, including fatal cases. Monitor patients for signs and symptoms of pneumonitis and evaluate patients with suspected pneumonitis with radiographic imaging. Administer corticosteroids (initial dose of 1 to 2 mg/kg/day prednisone or equivalent, followed by a corticosteroid taper) for Grade 2 or greater pneumonitis. Withhold BAVENCIO for moderate (Grade 2) pneumonitis, and permanently discontinue for severe (Grade 3), life-threatening (Grade 4), or recurrent moderate (Grade 2) pneumonitis.
- Pneumonitis occurred in 1.2% (21/1738) of patients receiving BAVENCIO including one (0.1%) patient with Grade 5, one (0.1%) with Grade 4, and five (0.3%) with Grade 3 pneumonitis. Immune-mediated pneumonitis led to permanent discontinuation of BAVENCIO in 0.3% (6/1738) of patients. Among the 21 patients with immune-mediated pneumonitis, the median time to onset was 2.5 months (range: 3 days to 11 months) and the median duration of pneumonitis was 7 weeks (range: 4 days to 4+ months). All 21 patients were treated with systemic corticosteroids; 17 (81%) of the 21 patients received high-dose corticosteroids for a median of 8 days (range: 1 day to 2.3 months). Resolution of pneumonitis occurred in 12 (57%) of the 21 patients at the time of data cut-off.
Immune-Mediated Hepatitis
- BAVENCIO can cause immune-mediated hepatitis including fatal cases. Monitor patients for abnormal liver tests prior to and periodically during treatment. Administer corticosteroids (initial dose of 1 to 2 mg/kg/day prednisone or equivalent, followed by a corticosteroid taper) for Grade 2 or greater hepatitis. Withhold BAVENCIO for moderate (Grade 2) immune-mediated hepatitis until resolution and permanently discontinue for severe (Grade 3) or life-threatening (Grade 4) immune-mediated hepatitis.
- Immune-mediated hepatitis occurred in 0.9% (16/1738) of patients receiving BAVENCIO including two (0.1%) patients with Grade 5 and 11 (0.6 %) patients with Grade 3 immune-mediated hepatitis. Immune-mediated hepatitis led to permanent discontinuation of BAVENCIO in 0.5% (9/1738) of patients. Among the 16 patients with immune-mediated hepatitis, the median time to onset was 3.2 months (range: 1 week to 15 months), and the median duration of hepatitis was 2.5 months (range: 1 day to 7.4+ months). All 16 patients were treated with corticosteroids; 15 (94%) of the 16 patients received high-dose corticosteroids for a median of 14 days (range: 1 day to 2.5 months). Resolution of hepatitis occurred in nine (56%) of the 16 patients at the time of data cut-off.
Immune-Mediated Colitis
- BAVENCIO can cause immune-mediated colitis. Monitor patients for signs and symptoms of colitis. Administer corticosteroids (initial dose of 1 to 2 mg/kg/day prednisone or equivalent followed by a corticosteroid taper) for Grade 2 or greater colitis. Withhold BAVENCIO for moderate or severe (Grade 2 or 3) colitis until resolution. Permanently discontinue BAVENCIO for life-threatening (Grade 4) or for recurrent (Grade 3) colitis upon re-initiation of BAVENCIO.
- Immune-mediated colitis occurred in 1.5% (26/1738) of patients receiving BAVENCIO including seven (0.4%) patients with Grade 3 colitis. Immune-mediated colitis led to permanent discontinuation of BAVENCIO in 0.5% (9/1738) of patients. Among the 26 patients with immune-mediated colitis, the median time to onset was 2.1 months (range: 2 days to 11 months) and the median duration of colitis was 6 weeks (range: 1 day to 14+ months). All 26 patients were treated with corticosteroids; 15 (58%) of the 26 patients received high-dose corticosteroids for a median of 19 days (range: 1 day to 2.3 months). Resolution of colitis occurred in 18 (70%) of the patients at the time of data cut-off.
Immune-Mediated Endocrinopathies
Adrenal Insufficiency
- Monitor patients for signs and symptoms of adrenal insufficiency during and after treatment. Administer corticosteroids as appropriate for adrenal insufficiency. Withhold BAVENCIO for severe (Grade 3) or life-threatening (Grade 4) adrenal insufficiency.
- Adrenal insufficiency occurred in 0.5% (8/1738) of patients receiving BAVENCIO including one patient (0.1%) with Grade 3 adrenal insufficiency. Immune-mediated adrenal insufficiency led to permanent discontinuation of BAVENCIO in 0.1% (2/1738) of patients. Among the 8 patients with immune-mediated adrenal insufficiency, the median time to onset was 2.5 months (range: 1 day to 8 months). All eight patients were treated with corticosteroids; four (50%) of the eight patients received high-dose corticosteroids for a median of 1 day (range: 1 day to 24 days).
Thyroid Disorders (Hypothyroidism/Hyperthyroidism)
- BAVENCIO can cause immune-mediated thyroid disorders. Thyroid disorders can occur at any time during treatment. Monitor patients for changes in thyroid function at the start of treatment, periodically during treatment, and as indicated based on clinical evaluation. Manage hypothyroidism with hormone-replacement therapy. Initiate medical management for control of hyperthyroidism. Withhold BAVENCIO for severe (Grade 3) or life-threatening (Grade 4) thyroid disorders.
- Immune-mediated thyroid disorders occurred in 6% (98/1738) of patients receiving BAVENCIO including 3 (0.2%) Grade 3 immune-mediated thyroid disorders. Immune-mediated thyroid disorders led to discontinuation of BAVENCIO in 0.1% (2/1738) of patients. Hypothyroidism occurred in 90 (5%) patients; hyperthyroidism in seven (0.4%) patients; and thyroiditis in four (0.2%) patients treated with BAVENCIO. Among the 98 patients with immune-mediated thyroid disorders, the median time to onset was 2.8 months (range: 2 weeks to 13 months) and the median duration was not estimable (range: 6 days to more than 26 months). Immune-mediated thyroid disorders resolved in seven (7%) of the 98 patients.
Type 1 Diabetes Mellitus
- BAVENCIO can cause type 1 diabetes mellitus, including diabetic ketoacidosis. Monitor patients for hyperglycemia or other signs and symptoms of diabetes. Withhold BAVENCIO and administer anti-hyperglycemics or insulin in patients with severe or life-threatening (Grade ≥ 3) hyperglycemia. Resume treatment with BAVENCIO when metabolic control is achieved on insulin replacement or anti-hyperglycemics.
- Type 1 diabetes mellitus without an alternative etiology occurred in 0.1% (2/1738) of patients including two cases of Grade 3 hyperglycemia that led to permanent discontinuation of BAVENCIO.
Immune-Mediated Nephritis and Renal Dysfunction
- BAVENCIO can cause immune-mediated nephritis. Monitor patients for elevated serum creatinine prior to and periodically during treatment. Administer corticosteroids (initial dose of 1 to 2 mg/kg/day prednisone or equivalent followed by a corticosteroid taper) for Grade 2 or greater nephritis. Withhold BAVENCIO for moderate (Grade 2) or severe (Grade 3) nephritis until resolution to ≤ Grade 1. Permanently discontinue BAVENCIO for life-threatening (Grade 4) nephritis.
- Immune-mediated nephritis occurred in 0.1% (1/1738) of patients receiving BAVENCIO; BAVENCIO was permanently discontinued in this patient.
Other Immune-Mediated Adverse Reactions
- BAVENCIO can result in severe and fatal immune-mediated adverse reactions. These immune-mediated reactions may involve any organ system. Most immune-mediated reactions initially manifest during treatment with BAVENCIO; however, immune-mediated adverse reactions can occur after discontinuation of BAVENCIO.
- For suspected immune-mediated adverse reactions, evaluate to confirm or rule out an immune-mediated adverse reaction and to exclude other causes. Depending upon the severity of the adverse reaction, withhold or permanently discontinue BAVENCIO, administer high dose corticosteroids, and if appropriate, initiate hormone replacement therapy. Upon improvement to Grade 1 or less, initiate corticosteroid taper. Resume BAVENCIO when the immune-mediated adverse reaction remains at Grade 1 or less following corticosteroid taper. Permanently discontinue BAVENCIO for any severe (Grade 3) immune-mediated adverse reaction that recurs and for any life-threatening immune-mediated adverse reaction.
- The following clinically significant, immune-mediated adverse reactions occurred at an incidence of less than 1% of 1738 patients treated with BAVENCIO for each of the following adverse reactions: immune-mediated myocarditis including fatal cases, immune-mediated myositis, psoriasis, arthritis, exfoliative dermatitis, erythema multiforme, pemphigoid, hypopituitarism, uveitis, Guillain-Barré syndrome, and systemic inflammatory response. The following clinically significant, immune-mediated adverse reactions have been reported with other products in this class: bullous dermatitis, Stevens Johnson Syndrome (SJS)/toxic epidermal necrolysis (TEN), pancreatitis, rhabdomyolysis, myasthenia gravis, histiocytic necrotizing lymphadenitis, demyelination, vasculitis, hemolytic anemia, hypophysitis, iritis, and encephalitis.
Infusion-Related Reactions
- BAVENCIO can cause severe or life-threatening infusion-related reactions. Premedicate with antihistamine and acetaminophen prior to the first 4 infusions. Monitor patients for signs and symptoms of infusion-related reactions including pyrexia, chills, flushing, hypotension, dyspnea, wheezing, back pain, abdominal pain, and urticaria. Interrupt or slow the rate of infusion for mild or moderate infusion-related reactions. Stop the infusion and permanently discontinue BAVENCIO for severe (Grade 3) or life-threatening (Grade 4) infusion-related reactions.
- Infusion-related reactions occurred in 25% (439/1738) of patients treated with BAVENCIO including three (0.2%) Grade 4 and nine (0.5%) Grade 3 infusion-related reactions. Ninety-three percent (1615/1738) of patients received premedication with antihistamine and acetaminophen. Eleven (92%) of the 12 patients with Grade ≥ 3 reactions were treated with intravenous corticosteroids. Fourteen percent of patients (252/1738) had infusion-related reactions that occurred after the BAVENCIO infusion was completed.
Embryo-Fetal Toxicity
- Based on its mechanism of action, BAVENCIO can cause fetal harm when administered to a pregnant woman. Animal studies have demonstrated that inhibition of the PD-1/PD-L1 pathway can lead to increased risk of immune-mediated rejection of the developing fetus resulting in fetal death. If this drug is used during pregnancy, or if the patient becomes pregnant while taking BAVENCIO, inform the patient of the potential risk to a fetus. Advise females of childbearing potential to use effective contraception during treatment with BAVENCIO and for at least one month after the last dose of BAVENCIO.
Adverse Reactions
Clinical Trials Experience
Central Nervous System
- (list/description of adverse reactions)
Cardiovascular
- (list/description of adverse reactions)
Respiratory
- (list/description of adverse reactions)
Gastrointestinal
- (list/description of adverse reactions)
Hypersensitive Reactions
- (list/description of adverse reactions)
Miscellaneous
- (list/description of adverse reactions)
Condition 2
Central Nervous System
- (list/description of adverse reactions)
Cardiovascular
- (list/description of adverse reactions)
Respiratory
- (list/description of adverse reactions)
Gastrointestinal
- (list/description of adverse reactions)
Hypersensitive Reactions
- (list/description of adverse reactions)
Miscellaneous
- (list/description of adverse reactions)
Postmarketing Experience
(Description)
Drug Interactions
- Drug 1
- Drug 2
- Drug 3
- Drug 4
- Drug 5
Drug 1
(Description)
Drug 2
(Description)
Drug 3
(Description)
Drug 4
(Description)
Drug 5
(Description)
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA):
(Description)
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Avelumab in women who are pregnant.
Labor and Delivery
(Description)
Nursing Mothers
(Description)g
Pediatric Use
(Description)
Geriatic Use
(Description)
Gender
(Description)
Race
(Description)
Renal Impairment
(Description)
Hepatic Impairment
(Description)
Females of Reproductive Potential and Males
(Description)
Immunocompromised Patients
(Description)
Others
(Description)
Administration and Monitoring
Administration
(Oral/Intravenous/etc)
Monitoring
Condition 1
(Description regarding monitoring, from Warnings section)
Condition 2
(Description regarding monitoring, from Warnings section)
Condition 3
(Description regarding monitoring, from Warnings section)
IV Compatibility
There is limited information regarding the compatibility of Avelumab and IV administrations.
Overdosage
Acute Overdose
Signs and Symptoms
(Description)
Management
(Description)
Chronic Overdose
Signs and Symptoms
(Description)
Management
(Description)
Pharmacology
Avelumab
| |
| Systematic (IUPAC) name | |
| ? | |
| Identifiers | |
| CAS number | ? |
| ATC code | ? |
| PubChem | ? |
| Chemical data | |
| Formula | ? |
| Mol. mass | ? |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status | |
| Routes | ? |
Mechanism of Action
(Description)
Structure
(Description with picture)
Pharmacodynamics
(Description)
Pharmacokinetics
(Description)
Nonclinical Toxicology
(Description)
Clinical Studies
Metastatic Merkel Cell Carcinoma
- The efficacy and safety of BAVENCIO was demonstrated in the JAVELIN Merkel 200 trial (NCT02155647), an open-label, single-arm, multi-center study conducted in patients with histologically confirmed metastatic MCC whose disease had progressed on or after chemotherapy administered for distant metastatic disease. The trial excluded patients with autoimmune disease; medical conditions requiring systemic immunosuppression; prior organ or allogeneic stem cell transplantation; prior treatment with anti-PD-1, anti-PD-L1, or anti-CTLA-4 antibodies; CNS metastases; infection with HIV, hepatitis B, or hepatitis C; or ECOG performance score ≥ 2.
- Patients received BAVENCIO 10 mg/kg as an intravenous infusion over 60 minutes every 2 weeks until disease progression or unacceptable toxicity. Patients with radiological disease progression not associated with significant clinical deterioration, defined as no new or worsening symptoms, no change in performance status for greater than 2 weeks, and no need for salvage therapy, could continue treatment. Tumor response assessments were performed every 6 weeks. The major efficacy outcome measures were confirmed overall response rate (ORR) according to Response Evaluation Criteria in Solid Tumors (RECIST) v1.1 as assessed by a blinded independent central review committee (IRC) and IRC-assessed duration of response. The efficacy analysis was conducted when the last patient enrolled had completed 12 months of follow-up.
- A total of 88 patients were enrolled. Baseline patient characteristics were a median age of 73 years (range: 33 to 88), 74% of patients were male, 92% were White, and the ECOG performance score was 0 (56%) or 1 (44%). Seventy-five percent of patients were 65 years or older, 35% were 75 or older, and 3% were 85 or older. Sixty-five percent of patients were reported to have had one prior anti-cancer therapy for metastatic MCC and 35% had two or more prior therapies. Fifty-three percent of patients had visceral metastases. All patients had tumor samples evaluated for PD-L1 expression; of these, 66% were PD-L1-positive (≥ 1% of tumor cells), 18% were PD-L1 negative, and 16% had non-evaluable results by an investigational immunohistochemistry assay. Archival tumor samples were evaluated for Merkel cell polyomavirus (MCV) using an investigational assay; of the 77 patients with evaluable results, 52% had evidence of MCV.
- Efficacy results are presented in Table 6. Responses were observed in patients regardless of tumor PD-L1 expression or presence of MCV.

Locally Advanced or Metastatic Urothelial Carcinoma
- The efficacy and safety of BAVENCIO was demonstrated in the UC cohorts of the JAVELIN Solid Tumor trial, an open-label, single-arm, multi-center study that included 242 patients with locally advanced or metastatic urothelial carcinoma (UC) with disease progression on or after platinum-containing chemotherapy or who had disease progression within 12 months of treatment with a platinum-containing neoadjuvant or adjuvant chemotherapy regimen. Patients with active or history of central nervous system metastasis; other malignancies within the last 5 years; organ transplant; conditions requiring therapeutic immune suppression; or active infection with HIV, hepatitis B, or hepatitis C were excluded. Patients with autoimmune disease, other than type 1 diabetes, vitiligo, psoriasis, or thyroid disease that did not require immunosuppressive treatment, were excluded. Patients were included regardless of their PD-L1 status.
- Patients received BAVENCIO at a dose of 10 mg/kg intravenously every 2 weeks until radiographic or clinical progression or unacceptable toxicity. Tumor response assessments were performed every 6 weeks. Efficacy outcome measures included confirmed overall response rate (ORR), as assessed by an Independent Endpoint Review Committee (IERC) using Response Evaluation Criteria in Solid Tumors (RECIST) v1.1, and duration of response (DOR). Efficacy was evaluated in patients who were followed for a minimum of both 13 weeks and 6 months at the time of data cut-off.
- Baseline demographic and disease characteristics for the 226 patients with a minimum of 13 weeks of follow-up were median age 68 years (range: 30 to 89), 72% male, 80% White, and 34% and 66% of patients had an ECOG performance status 0 and 1, respectively. Forty-four percent of patients had non-bladder urothelial carcinoma including 23% of patients with upper tract disease, and 83% of patients had visceral metastases (baseline target and/or non-target lesions present outside of the lymph nodes). Nine (4%) patients had disease progression following prior platinum-containing neoadjuvant or adjuvant therapy only. Forty-seven percent of patients only received prior cisplatin-based regimens, 32% received only prior carboplatin-based regimens, and 20% received both cisplatin and carboplatin-based regimens. At baseline, 17% of patients had a hemoglobin < 10 g/dL and 34% of patients had liver metastases.
- Efficacy results are presented in Table 7. The median time to response was 2.0 months (range: 1.3 to 11.0) among patients followed for either ≥ 13 weeks or ≥ 6 months. Using a clinical trial assay to assess PD-L1 staining, with 16% of patients not evaluable, there were no clear differences in response rates based on PD-L1 tumor expression. Among the total 30 responding patients followed for ≥ 13 weeks, 22 patients (73%) had an ongoing response of 6 months or longer and 4 patients (13%) had ongoing responses of 12 months or longer. Among the total 26 responding patients followed for ≥ 6 months, 22 patients (85%) had ongoing responses of 6 months or longer and 4 patients (15%) had ongoing responses of 12 months or longer.
How Supplied
- BAVENCIO (avelumab) Injection is a sterile, preservative-free, and clear, colorless to slightly yellow solution for intravenous infusion supplied as a single-dose vial of 200 mg/10 mL (20 mg/mL), individually packed into a carton (NDC 44087-3535-1).
Storage
- Store refrigerated at 36°F to 46°F (2°C to 8°C) in original package to protect from light.
- Do not freeze or shake the vial.
- The vial stopper is not made with natural rubber latex.
Images
Drug Images
{{#ask: Page Name::Avelumab |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel

{{#ask: Label Page::Avelumab |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Immune-Mediated Adverse Reactions
Inform patients of the risk of immune-mediated adverse reactions requiring corticosteroids or hormone replacement therapy, including, but not limited to:
- Pneumonitis: Advise patients to contact their healthcare provider immediately for new or worsening cough, chest pain, or shortness of breath.
- Hepatitis: Advise patients to contact their healthcare provider immediately for jaundice, severe nausea or vomiting, pain on the right side of abdomen, lethargy, or easy bruising or bleeding.
- Colitis: Advise patients to contact their healthcare provider immediately for diarrhea or severe abdominal pain.
- Endocrinopathies: Advise patients to contact their healthcare provider immediately for signs or symptoms of adrenal insufficiency, hypothyroidism, hyperthyroidism, and diabetes mellitus.
- Nephritis and Renal Dysfunction: Advise patients to contact their healthcare provider immediately for signs or symptoms of nephritis including decreased urine output, blood in urine, swelling in ankles, loss of appetite, and any other symptoms of renal dysfunction.
Infusion-Related Reactions
- Advise patients to contact their healthcare provider immediately for signs or symptoms of potential infusion-related reactions.
Embryo-Fetal Toxicity
- Advise females of reproductive potential that BAVENCIO can cause fetal harm. Instruct females of reproductive potential to use highly effective contraception during and for at least one month after the last dose of BAVENCIO.
Lactation
- Advise nursing mothers not to breastfeed while taking BAVENCIO and for at least one month after the final dose.
Precautions with Alcohol
Alcohol-Avelumab interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
- Bavencio
Look-Alike Drug Names
There is limited information regarding Avelumab Look-Alike Drug Names in the drug label.
Drug Shortage Status
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.