Autoimmune hepatitis pathophysiology
|
Autoimmune hepatitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Autoimmune hepatitis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Autoimmune hepatitis pathophysiology |
|
Risk calculators and risk factors for Autoimmune hepatitis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Manpreet Kaur, MD [2]
Overview
Autoimmune hepatitis is a chronic disease characterized by inflammation of the liver which results from the combination of genetic predisposition and environmental triggers. The genetic predisposition is related to the defect in HLA haplotypes B8, B14, DR3, DR4, and Dw3, complement system, and T-cell level. The environmental factors involved are viruses like Rubella, Epstein-Barr, Hepatitis A, B, and C have molecular mimicry of viral sequences to host proteins and drugs like oxyphenisatin, methyldopa, nitrofurantoin, diclofenac, interferon, minocycline, and atorvastatin causes autoimmune hepatitis.
Pathophysiology
Autoimmune hepatitis is a chronic disease characterized by inflammation of the liver which results from the combination of genetic predisposition and environmental triggers
Normal physiology of liver:[1][2][3][4][5]
- Liver is known to be an organ with special innate immune features.
- Liver has distinct cellular composition with predominance of Kupffer cells (KCs), natural killer (NK) cells and natural killer T (NKT).
- Liver is constantly exposed to microbial products,(toxic) environmental substances and food antigens from the portal stream draining the intestine, the liver plays an important role in the induction and maintenance of immune tolerance.
- Liver is a target of adverse immune reactions in chronic inflammatory liver diseases like autoimmune hepatitis (AIH), primary biliary cirrhosis (PBC) and primary sclerosing cholangitis (PSC).
Various factors involved in pathogenesis of autoimmune hepatitis
Autoimmune hepatitis is a chronic idiopathic disease that occurs as a result of an environmental factor that triggers a series of T-cell–mediated events directed at liver antigens in a genetically predisposed host.
Genetic factors
- The genetic predisposition is related to the defect in HLA haplotypes B8, B14, DR3, DR4, and Dw3, complement system, and T-cell level.
- HLA-DR3 positive patients are usually younger and less responsive to medical therapy.
- HLA-DR4 patients usually develop extrahepatic manifestations of their disease.
- There is a partial deficiency of complement component C4 which results in failure to remove viruses.
- There are low levels of T lymphocytes that express the CD8 marker and a specific defect in a subpopulation of T cells that controls the immune response to specific liver cell membrane antigens.[6]
Environmental factors:
Various environmental factors involved are:
- Viruses like rubella, Epstein-Barr, hepatitis A, B, and C have molecular mimicry of viral sequences to host proteins.
- Drugs like oxyphenisatin, methyldopa, nitrofurantoin, diclofenac, interferon, minocycline, and atorvastatin causes autoimmune hepatitis.
- An environmental agents triggered the autoimmune response against liver antigens leads to necroinflammatory liver damage, fibrosis, and cirrhosis.
Pathogenesis
Mechanism of Autoreactivity:[7][8][9][10]
- Autoimmune hepatitis is caused by a cell-mediated immunologic attack.
- There is abnormal position of human leukocyte antigen (HLA) class II on the surface of liver cells which is caused by genetic and environmental triggers.
- This further leads to the exposure of normal liver cell membrane constituents to antigen-presenting cells(APC).
- APC further interacts with helper T-cell at the ligand-ligand levels leads to activation helper T-cells.
- Helper T-cells activation is followed by differentiation of helper T-cells into helper T cell 1 (TH 1) or helper T cell 2 (TH 2).
- TH 1 secretes interleukin 2 (IL-2) and interferon gamma, which activate macrophages.
- TH 2 cells produce interleukins 4, 5, and 10, which activate autoantibody production by B cells.
- Normally TH 1 and TH 2 cells antagonize each other.
- Failure of autoantigen recognition leads to autoimmune attack.
- The action of cytotoxic lymphocytes that are stimulated by IL-2, complement activation, natural killer lymphocytes, or reaction of autoantibodies with liver-specific antigens causes injury to liver.
Genetics
- Genes deletion involved in the pathogenesis of autoimmune hepatitis include C4A gene.
- Autoimmune hepatitis have an abnormality in the MHC locus on chromosome 6.
Associated Conditions
Associated conditions due to the AH:
- Chronic autoimmune thyroiditis
- Hyperthyroidism (Graves’ disease)
- Ulcerative colitis
- Hemolytic anemia
- Idiopathic thrombocytopenia
- Diabetes mellitus
- Diabetes insipidus
- Celiac disease
- Polymyositis
- Myasthenia gravis
- Pulmonary fibrosis
- Pericarditis
- Glomerulonephritis
- Acute lichenoid pityriasis
- Febrile panniculitis
- Hypereosinophilic syndrome
- Sjogren’s syndrome
- Mixed connective tissue disease
Gross Pathology
- On gross pathology, diffuse whitish-gray plaque without nodularity are demonstrated in autoimmune hepatitis.
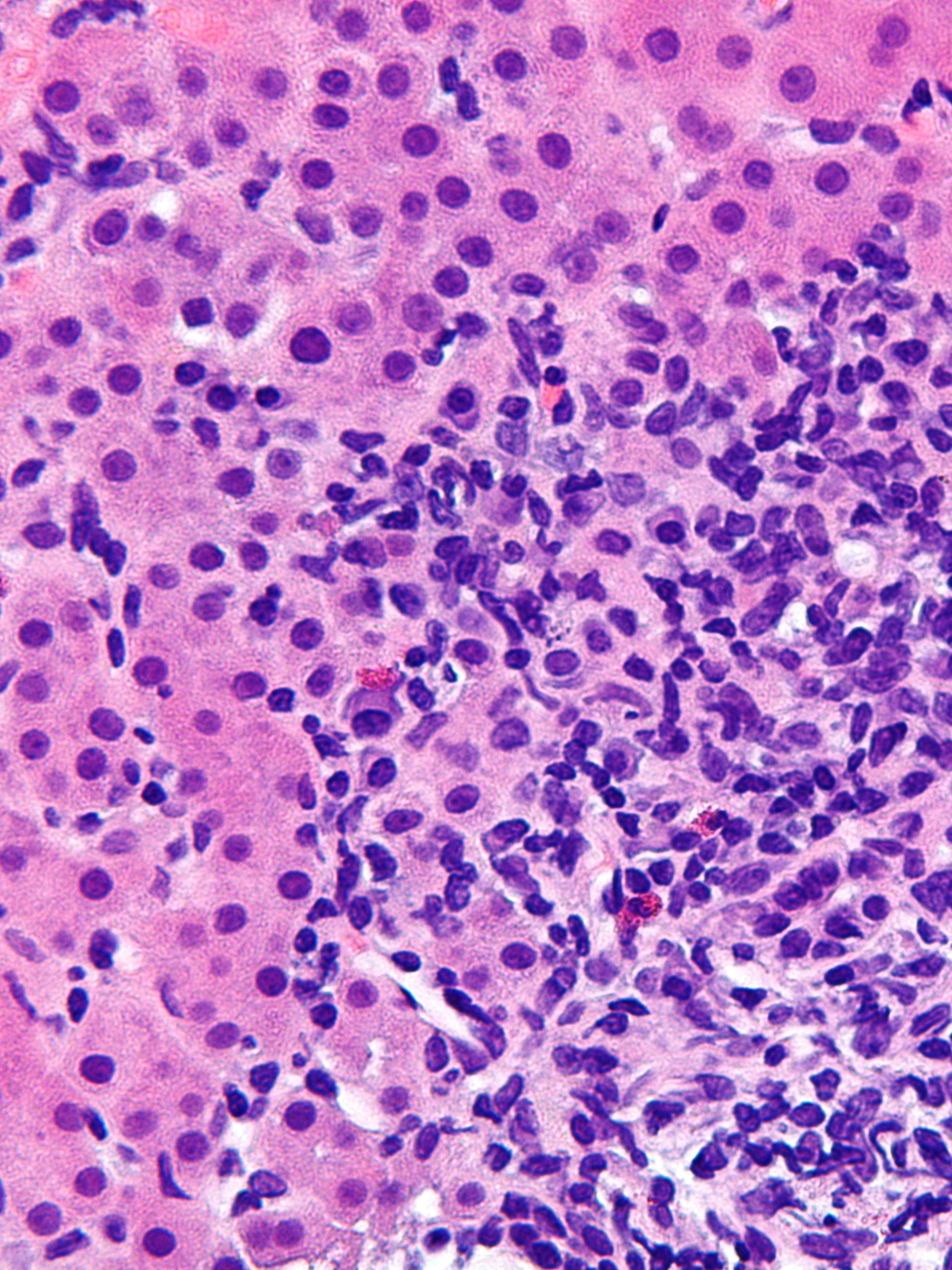
Microscopic Pathology
Microscopic histopathologic features are:[11][12]
- A portal and periportal infiltrate of mononuclear cells.
- The infiltrate crosses the limiting plate that forms the portal triad and invades the surrounding lobule.
- The periportal infiltrate is occasionally referred to as piecemeal necrosis and generally spares the biliary tree.
- Emperipolesis: apparent engulfment of lymphocytes by hepatocytes.
- Hepatocyte rosette formation.
- Variable fibrosis.
References
- ↑ Seki S, Habu Y, Kawamura T, Takeda K, Dobashi H, Ohkawa T, Hiraide H (2000). "The liver as a crucial organ in the first line of host defense: the roles of Kupffer cells, natural killer (NK) cells and NK1.1 Ag+ T cells in T helper 1 immune responses". Immunol. Rev. 174: 35–46. PMID 10807505.
- ↑ Selmi C, Mackay IR, Gershwin ME (2007). "The immunological milieu of the liver". Semin. Liver Dis. 27 (2): 129–39. doi:10.1055/s-2007-979466. PMID 17520513.
- ↑ Gao B, Jeong WI, Tian Z (2008). "Liver: An organ with predominant innate immunity". Hepatology. 47 (2): 729–36. doi:10.1002/hep.22034. PMID 18167066.
- ↑ Feld JJ, Heathcote EJ (2003). "Epidemiology of autoimmune liver disease". J. Gastroenterol. Hepatol. 18 (10): 1118–28. PMID 12974897.
- ↑ Corless JK, Middleton HM (1983). "Normal liver function. A basis for understanding hepatic disease". Arch. Intern. Med. 143 (12): 2291–4. PMID 6360063.
- ↑ Mattner J (2011). "Genetic susceptibility to autoimmune liver disease". World J Hepatol. 3 (1): 1–7. doi:10.4254/wjh.v3.i1.1. PMC 3035697. PMID 21307981.
- ↑ Liberal R, Longhi MS, Mieli-Vergani G, Vergani D (2011). "Pathogenesis of autoimmune hepatitis". Best Pract Res Clin Gastroenterol. 25 (6): 653–64. doi:10.1016/j.bpg.2011.09.009. PMID 22117632.
- ↑ McFarlane IG (1999). "Pathogenesis of autoimmune hepatitis". Biomed. Pharmacother. 53 (5–6): 255–63. doi:10.1016/S0753-3322(99)80096-1. PMID 10424247.
- ↑ Obermayer-Straub P, Strassburg CP, Manns MP (2000). "Autoimmune hepatitis". J. Hepatol. 32 (1 Suppl): 181–97. PMID 10728804.
- ↑ Vergani D, Choudhuri K, Bogdanos DP, Mieli-Vergani G (2002). "Pathogenesis of autoimmune hepatitis". Clin Liver Dis. 6 (3): 727–37. PMID 12362577.
- ↑ Dienes HP, Popper H, MAnns M, Baumann W, Thoenes W, Meyer Zum Büschenfelde KH (1989). "Histologic features in autoimmune hepatitis". Z Gastroenterol. 27 (6): 325–30. PMID 2505455.
- ↑ Tiniakos DG, Brain JG, Bury YA (2015). "Role of Histopathology in Autoimmune Hepatitis". Dig Dis. 33 Suppl 2: 53–64. doi:10.1159/000440747. PMID 26642062.
- ↑ https://commons.wikimedia.org/wiki