Autoimmune hepatitis: Difference between revisions
| Line 121: | Line 121: | ||
== Treatment == | == Treatment == | ||
===Recommendations for treatment of Autoimmune Hepatitis (DO NOT EDIT)=== | ===Recommendations for the treatment of Autoimmune Hepatitis (DO NOT EDIT)=== | ||
{{cquote| | {{cquote| | ||
# Immunosuppressive treatment based on serum aspartate aminotransferase (AST), serum alanine aminotransferase (ALT), serum gamma-globulin levels, and histological features | # Immunosuppressive treatment based on serum aspartate aminotransferase (AST), serum alanine aminotransferase (ALT), serum gamma-globulin levels, and histological features | ||
Revision as of 03:27, 7 September 2012
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Autoimmune hepatitis (AH) was first described in the 1950s and has had a variety of names including chronic active hepatitis, lupoid hepatitis, plasma cell hepatitis and autoimmune chronic active hepatitis. It is characterized by circulating autoantibodies and a high serum globulin level. It is important to distinguish AH from other forms of liver disease, as a large percentage of patients respond to therapy and therapy has been shown to delay transplantation, improve the quality of life as well as prolong survival. Lupoid hepatitis (also called Autoimmune hepatits) is an auto-immune disease which causes liver cirrhosis. It may be associated with systemic lupus erythematosus (SLE) or other connective tissue disorders. 60% of patients have chronic hepatitis that may mimic viral hepatitis, but without serologic evidence of a viral infection. The disease usually affects women and is strongly associated with anti-smooth muscle auto-antibodies. Autoimmune hepatitis is a condition in which the patient's own immune systems attacks the liver causing inflammation and liver cell death. The condition is chronic and progressive. Although the disease is chronic, many patients with autoimmune hepatitis present acutely ill with jaundice, fever and sometimes symptoms of severe hepatic dysfunction, a picture that resembles acute hepatitis.
"Autoimmune hepatitis usually occurs in women (70 %) between the ages of 15 and 40. Although the term "lupoid" hepatitis was originally used to describe this disease, patients with systemic lupus erythematosus do not have an increased incidence of autoimmune hepatitis and the two diseases are distint entities. Patients usually present with evidence of moderate to severe hepatitis with elevated serum ALT and AST activities in the setting of normal to marginally elevated alkaline phosphatase and gamma-glutamyltranspeptidase activities. The patient will sometimes present with jaundice, fever and right upper quadrant pain and occasionally systemic symptoms such as arthralgias, myalgias, polyserositits and thrombocytopenia. Some patients will present with mild liver dysfunction and have only laboratory abnormalities as their initial presentation. Others will present with severe hepatic dysfunction." [1]
Differential Diagnosis
Unfortunately, this histologic picture is not specific to AH:
- Autoimmune liver disease
- Primary biliary cirrhosis
- Primary sclerosing cholangitis
- Overlap syndrome
- Autoimmune cholangiopathy
- Chronic viral hepatitis
- Chronic hepatitis B
- Chronic hepatitis C
- Chronic hepatitis delta
- Chronic hepatitis due to other viruses
- Chronic drug-induced hepatitis
- Alpha-1 antitrypsin deficiency
- Wilson's disease
- Cholangiography related to the acquired immunodeficiency syndrome
- Granulomatous hepatitis
- Systemic lupus erythematosus
- Graft-versus-host disease
- Alcoholic steatohepatitis
- Nonalcoholic steatohepatitis
- Autoimmune liver disease
Classification
There are two basic forms of AH: type I (classic) and type II.
- Both are more common in women than men.
- Type II disease occurs in girls and young women, whereas type I disease is seen in all age groups.
Pathophysiology & Etiology
- Although still considered an idiopathic disease, AH is thought to result from a double-hit:
- An environmental stimulus triggers an autoimmune process directed against liver antigens in a genetically susceptible host.
- Most patients with AH have an abnormality in the MHC locus on chromosome 6.
- Additionally, there is evidence that loci that encode complement products, immunoglobulins and T-cell receptors play a role in the genetic predisposition to AH.
- As far as the environmental stimulus goes, postulated associations include the measles virus, hepatitis viruses as well as Epstein-Barr virus (EBV).
- Unfortunately, the relevant antigens and the mechanisms underlying the chronicity of inflammation remain undefined.
- The circulating antinuclear, anti-smooth muscle and antiactin antibodies are not organ specific, do not appear to have a role in the direct pathogenesis, and are thought to be just markers of disease.
- Recent attention has, however, focused on the asialoglycoprotein receptor (a liver specific membrane protein that may be the target for cellular toxicity).
- Defects in suppressor T-cell function are also thought to play a role in the pathogenesis of AH, resulting in the unmodulated production of IgG antibodies against normal hepatocyte membranes.
- The circulating antinuclear, anti-smooth muscle and antiactin antibodies are not organ specific, do not appear to have a role in the direct pathogenesis, and are thought to be just markers of disease.
Pathology
- A liver biopsy is essential for the diagnosis of AH. Histological features include:
- A portal and periportal infiltrate of mononuclear cells.
- The infiltrate crosses the limiting plate that forms the portal triad and invades the surrounding lobule.
- The periportal infiltrate is occasionally referred to as piecemeal necrosis, and generally spares the biliary tree.
- All cases, except the most mild, have some degree of ‘bridging fibrosis’ that connects the portal and central areas.
- Primary biliary cirrhosis (PBC) and Primary sclerosing cholangitis (PSC) tend to have either a paucity of, inflammation of, or damage to the bile ducts (or all three features).
- Cholangiography is often required to differentiate PSC from AH.
- The ‘overlap syndrome’ has the histologic features of AH in conjunction with the serologic features of PBC (anti-mitochondrial antibodies).
- A portal and periportal infiltrate of mononuclear cells.
Diagnosis
History and Symptoms
- Patients with AH can present anywhere in the spectrum from totally asymptomatic disease (only to be diagnosed when routine liver function tests (LFTs) are abnormal), to an acute, fulminant hepatitis.
- Patients can also present with a variety of constitutional symptoms such as malaise, fatiguability, anorexia, abdominal pain and pruritis.
- Small joint arthralgia is also a common complaint.
- Extrahepatic manifestations are generally due to the company that AH keeps:
- Chronic autoimmune thyroiditis
- Hyperthyroidism (Graves’ disease)
- Ulcerative colitis
- Hemolytic anemia
- Idiopathic thrombocytopenia
- Diabetes mellitus
- Diabetes insipidus
- Celiac disease
- Polymyositis
- Myasthenia gravis
- Pulmonary fibrosis
- Pericarditis
- Glomerulonephritis
- Acute lichenoid pityriasis
- Febrile panniculitis
- Hypereosinophilic syndrome
- Sjogren’s syndrome
- Mixed connective tissue disease
- Although PSC is generally thought to be the liver disease most commonly associated with uterine contractions (UC), AH and UC often coexist, with the liver disease predating the colonic disease.
- AH is also associated with hepatocellular carcinoma, though many patients who eventually develop hepatocellular carcinoma have also been found to have hepatitis C.
- The LFT abnormalities are generally that of a marked transaminitis with a milder increase in Total bilirubin, alkalen phosphatase and PT.
- Some patients, however, have more of a cholestatic picture.
- Unfortunately, the symptoms and degree of enzyme abnormalities do not necessarily correlate with the pathology.
- As above, however, most patients have at least some degree of cirrhosis at the time of initial biopsy.
- Hyperglobulinemia (usually gamma-globulin) is a characteristic feature of AH, though is not present in 100% of cases.
- Anti-actin antibodies are generally not tested for in most labs, despite the fact that they are more specific than the other tests for AH.
- An anti-smooth muscle Ab titer > 1:320, however, is generally thought to reflect the presence of anti-actin antibodies.
- In the spectrum of autoimmune disease ranging from organ-specific to non-organ-specific, AH falls somewhere in the middle, as the disease is often confined to the liver, but the antibodies are mostly nonspecific.
- A scoring system has been developed by the International Autoimmune Hepatitis Group in order to facilitate the diagnosis.
Diagnostic Findings
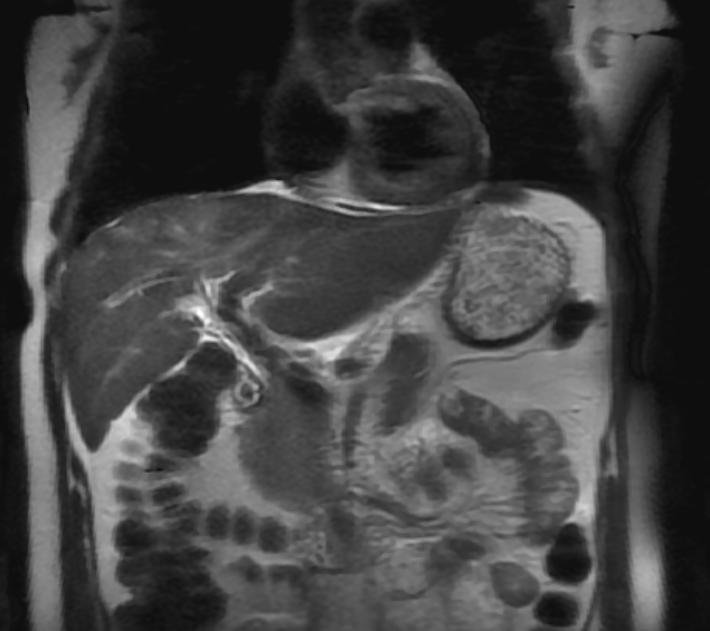
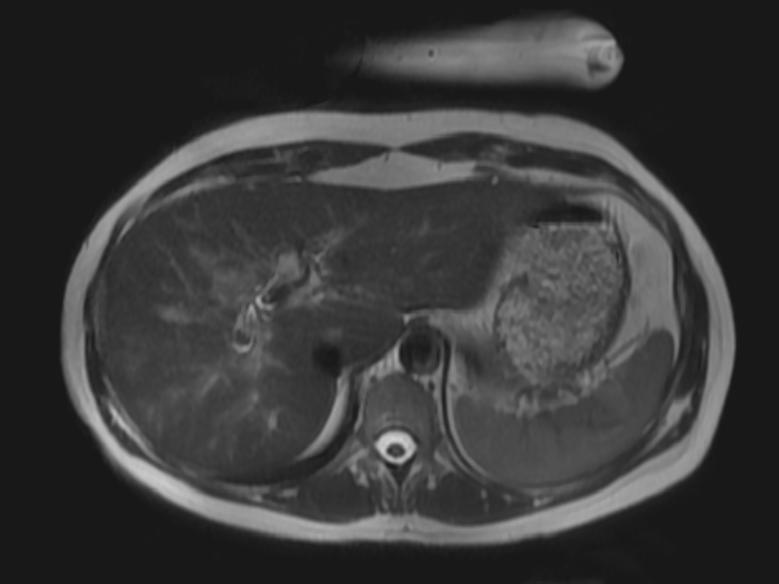
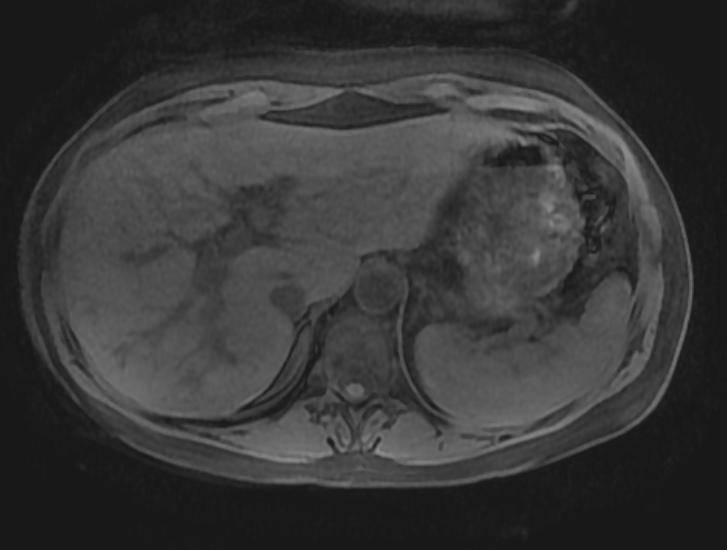
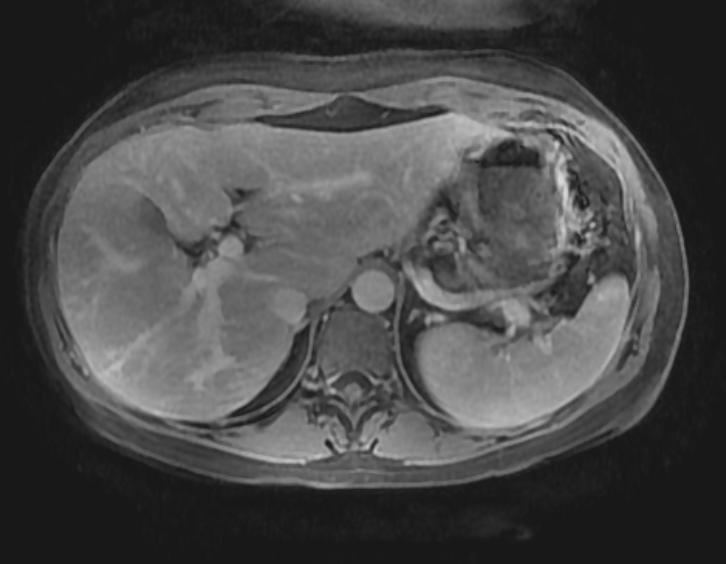
MRI
-
T2
-
T2
-
T1 fat sat
-
T1 fat sat post contrast
-
T1 fat sat post contrast
-
T1 fat sat post contrast
Risk Stratification and Prognosis
- The prognosis is generally thought to be inversely correlated with the histologic severity of disease.
- Approximately 50% of patients will remain in remission or have only mild disease when steroids are withdrawn after the initial therapy.
- Most patients, however, will require long-term maintenance therapy.
Treatment
Recommendations for the treatment of Autoimmune Hepatitis (DO NOT EDIT)
| “ |
|
” |
Acute Pharmacotherapies
- Despite our clear understanding of the pathogenesis and pathophysiology of AH, approximately 80 % of patients will have a good initial response to corticosteroids, with a ten-year survival rate approaching 90%.
- The decision to treat patients with only mild disease is often based on symptoms.
- Asymptomatic patients with mild inflammation on Bx can be observed with careful monitoring of histology.
- The goal of therapy is generally normalization of both transaminases and histology, and in general, most patients who are going to respond do so by 6 months.
- Unfortunately, the results with alternate-day or pulsed steroid regimens have been disappointing and daily regimens are preferred.
- Azathioprine can be used as a steroid-sparing agent.
- Additionally, some authors recommend using lower prednisone doses with the goal of partial suppression of disease, as opposed to higher doses of steroids with the goal being remission.
- For the 10 – 20% of patients who develop progressive disease despite steroids and/or azathioprine, cyclosporine and tacrolimus have recently been shown to induce remission.
- There are no firm guidelines concerning the tapering or discontinuation of therapy.
Transplantation
- Transplantation has also had impressive results with five-year survival rates between 92 and 100%, however AH can recur in the transplanted liver despite aggressive immunosuppression.
References
- ↑ Krawitt, E. L. 1996. Autoimmune hepatitis. New England Journal of Medicine. 334:897-903.
- Czaja, A.J., Autoimmune hepatitis: evolving concepts and treatment strategies, Dig Dis and Sciences 1995, 40: 435-456.
- Czaja, A.J., The variant forms of autoimmune hepatitis, Ann Intern Med 1996; 125: 588-598.
- Fernandes, N.F., et.al., Cyclosporine therapy in patients with steroid resistant autoimmune hepatitis, Am J Gastroenterol 1999; 94: 241-248.
- Krawitt, E.L., Autoimmune hepatitis, NEJM 1996, 334: 897-903.
- Krawitt, E.L., Treatment of autoimmune hepatitis, in UpToDate, June 23, 1998.
- Krawitt, E.L, Clinical manifestation and diagnosis of autoimmune hepatitis, in UpToDate, April 1, 1998.