Atrial septal defect pathophysiology: Difference between revisions
| Line 8: | Line 8: | ||
==Pathophysiology== | ==Pathophysiology== | ||
===Left-Sided Versus Right-Sided Pressures=== | ===Left-Sided Versus Right-Sided Pressures=== | ||
In unaffected individuals, the chambers of the left side of the heart make up a higher pressure system than the chambers of the right side of the heart. This is because the [[left ventricle]] has to produce enough pressure to pump blood throughout the entire body, while the [[right ventricle]] only has to produce enough pressure to pump blood to the [[lung]]s. | In unaffected individuals, the chambers of the left side of the [[heart]] make up a higher pressure system than the chambers of the right side of the heart. This is because the [[left ventricle]] has to produce enough pressure to pump blood throughout the entire body, while the [[right ventricle]] only has to produce enough pressure to pump blood to the [[lung]]s. | ||
===Calculation of the Pulmonary to Systemic Flow Ratios=== | ===Calculation of the Pulmonary to Systemic Flow Ratios=== | ||
Revision as of 17:07, 8 January 2013
|
Atrial Septal Defect Microchapters | |
|
Treatment | |
|---|---|
|
Surgery | |
|
| |
|
Special Scenarios | |
|
Case Studies | |
|
Atrial septal defect pathophysiology On the Web | |
|
American Roentgen Ray Society Images of Atrial septal defect pathophysiology | |
|
Risk calculators and risk factors for Atrial septal defect pathophysiology | |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Priyamvada Singh, M.B.B.S. [2]; Assistant Editor(s)-In-Chief: Kristin Feeney, B.S. [3]
Overview
In a normal heart, the typical path of blood flow is to flow from right-to-left allowing for blood to leave the deoxygenated right system and become oxygenated in the left system. In patients with an atrial septal defect, the typical path of blood flow is disrupted by the septal opening. This results in blood shunting from left-to-right. The severity of circulatory complications depends largely on the size of the defect. The larger the defect between the septal walls, the greater the amount of mixing between deoxygenated and oxygenated blood. Flow from the left atrium into the right atrium increases flow through the pulmonary circuit increasing the load on the right ventricle and slowly injuring the pulmonary vasculature over time.
Pathophysiology
Left-Sided Versus Right-Sided Pressures
In unaffected individuals, the chambers of the left side of the heart make up a higher pressure system than the chambers of the right side of the heart. This is because the left ventricle has to produce enough pressure to pump blood throughout the entire body, while the right ventricle only has to produce enough pressure to pump blood to the lungs.
Calculation of the Pulmonary to Systemic Flow Ratios
In the case of a large ASD (>9 mm), which may result in a clinically significant left-to-right shunt, blood will shunt from the left atrium to the right atrium causing excessive mixing of the blood between the two atria. In a hemodynamically significant ASD, Qp is the pulmonary flow and Qs is the systemic flow and the Qp:Qs > 1.5:1). If the Qp:Qs is > 1.5:1, then the patient is often symptomatic, and a repair of the ASD may be indicated. This extra blood from the left atrium may cause a volume overload of both the right atrium and the right ventricle, which if left untreated, can result in enlargement of the right side of the heart and ultimately right-sided heart failure.
Impact of Changes in Left Ventricular Loading Conditions
Any process that increases the pressure in the left ventricle can cause worsening of the left-to-right shunt. This includes hypertension, which increases the pressure that the left ventricle has to generate in order to open the aortic valve during ventricular systole, and coronary artery disease which increases the stiffness of the left ventricle, thereby increasing the filling pressure of the left ventricle during ventricular diastole.
Right Heart Failure As a Consequence of Left Right Shunting
The right ventricle will have to push out more blood than the left ventricle due to the left-to-right shunt. This constant overload of the right side of the heart will cause an overload of the entire pulmonary vasculature. Eventually the pulmonary vasculature will develop pulmonary hypertension as a result of the extra blood flow through the lungs.
The resulting pulmonary hypertension will cause the right ventricle to face increased pressure or increased afterload in addition to the increased preload (higher volume coming into the right side of the heart) as a result of the shunted blood flowing from the left atrium into the right atrium. The right ventricle will be forced to generate higher pressures to try to overcome the pulmonary hypertension. This may lead to right ventricular failure (dilatation and decreased systolic function of the right ventricle). Eventually the right-sided pressures may exceed left-sided pressures.
Equalization of Left and Right Atrial Pressures
When the pressure in the right atrium rises to the level in the left atrium, there will no longer be a pressure gradient between these heart chambers, and the left-to-right shunt will diminish or cease.
Development of Right-to-Left Shunting or Eisenmenger's Syndrome
If left uncorrected, the pressure in the right side of the heart will be greater than the left side of the heart. This will cause the pressure in the right atrium to be higher than the pressure in the left atrium. This will reverse the pressure gradient across the ASD, and the shunt will reverse; a right-to-left shunt will exist. This phenomenon is known as Eisenmenger's syndrome. Once right-to-left shunting occurs, a portion of the oxygen-poor blood will get shunted to the left side of the heart and ejected to the peripheral vascular system. This will cause signs of cyanosis. once Eisenmenger's syndrome develops, the patient can no longer benefit from surgery to correct the defect.
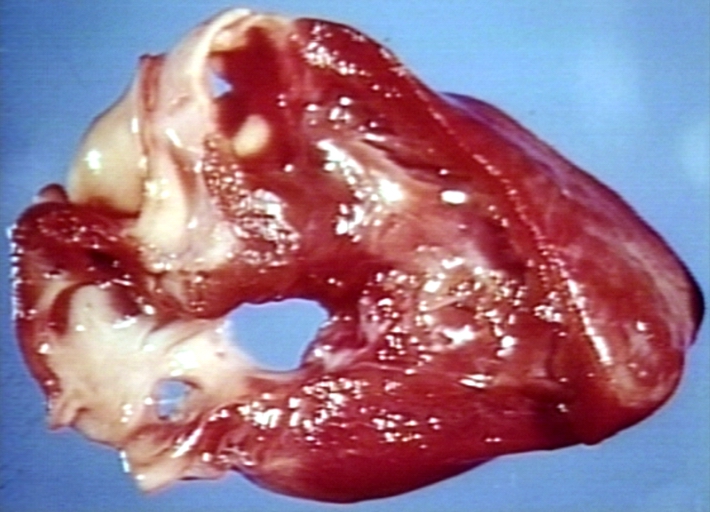
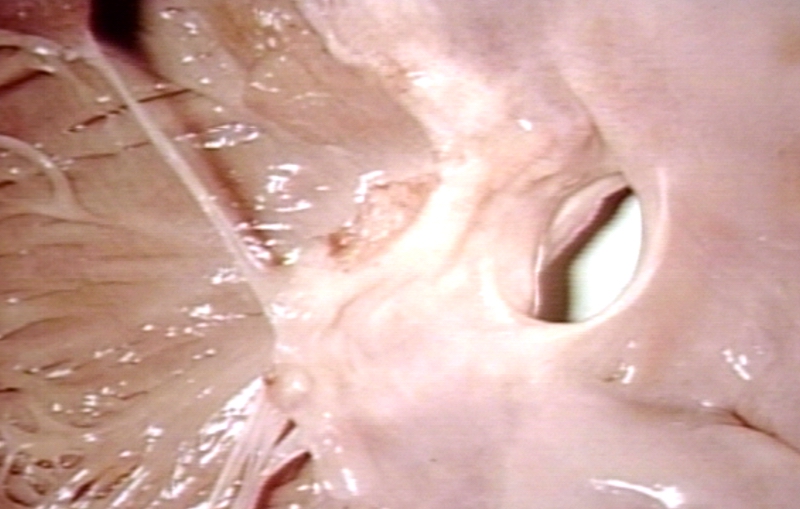
Gross Pathology
-
Atrial Septal Defect, Septum Primum; View from Right Atrium (a 4 month old baby)
-
Atrial Septal Defect, Septum Primum; Also Cleft in Anterior Cusp of Mitral Valve
Associated Conditions
Secundum ASD is seen in Holt-Oram Syndrome with obvious limb malformations.