Asthma
| Asthma | ||
| ICD-10 | J45 | |
|---|---|---|
| ICD-9 | 493 | |
| OMIM | 600807 | |
| DiseasesDB | 1006 | |
| MedlinePlus | 000141 | |
| MeSH | C08.127.108 | |
|
WikiDoc Resources for Asthma |
|
Articles |
|---|
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Asthma at Clinical Trials.gov Clinical Trials on Asthma at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Asthma
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Directions to Hospitals Treating Asthma Risk calculators and risk factors for Asthma
|
|
Healthcare Provider Resources |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For patient information click here
Editor-in-Chief: C. Michael Gibson, M.S., M.D.; Philip Marcus, M.D., M.P.H. [1], Division of Pulmonary Medicine St. Francis Hospital-The Heart Center, Roslyn, NY
Overview
Asthma is a chronic illness involving the respiratory system in which the airway occasionally constricts, becomes inflamed, and is lined with excessive amounts of mucus, often in response to one or more triggers. These episodes may be triggered by such things as exposure to an environmental stimulant (or allergen), cold air, warm air, moist air, exercise or exertion, or emotional stress. In children, the most common triggers are viral illnesses such as those that cause the common cold.[1] This airway narrowing causes symptoms such as wheezing, shortness of breath, chest tightness, and coughing. The airway constriction responds to bronchodilators. Between episodes, most patients feel well but can have mild symptoms and they may remain short of breath after exercise for longer periods of time than the unaffected individual. The symptoms of asthma, which can range from mild to life threatening, can usually be controlled with a combination of drugs and environmental changes.
Public attention in the developed world has recently focused on asthma because of its rapidly increasing prevalence, affecting up to one in four urban children.[2]
History
The word 'asthma' is derived from the Ancient Greek aazein, meaning "sharp breath." The word first appears in Homer's Iliad;[3] Hippocrates was the first to use it in reference to the medical condition, in 450 BC. Hippocrates thought that the spasms associated with asthma were more likely to occur in tailors, anglers, and metalworkers. Six centuries later, Galen wrote much about asthma, noting that it was caused by partial or complete bronchial obstruction. In 1190 AD, Moses Maimonides, an influential medieval rabbi, philosopher, and physician, wrote a treatise on asthma, describing its prevention, diagnosis, and treatment.[4] In the 17th century, Bernardino Ramazzini noted a connection between asthma and organic dust. The use of bronchodilators started in 1901, but it was not until the 1960s that the inflammatory component of asthma was recognized, and anti-inflammatory medications were added to the regimens.
Epidemiology
More than 6% of children in the United States have been diagnosed with asthma, a 75% increase in recent decades. The rate soars to 40% among some populations of urban children.
Asthma is usually diagnosed in childhood. The risk factors for asthma include:
- a personal or family history of asthma or atopy;
- triggers (see Pathophysiology above);
- premature birth or low birth weight;
- viral respiratory infection in early childhood;
- maternal smoking;
- being male, for asthma in prepubertal children; and
- being female, for persistence of asthma into adulthood.
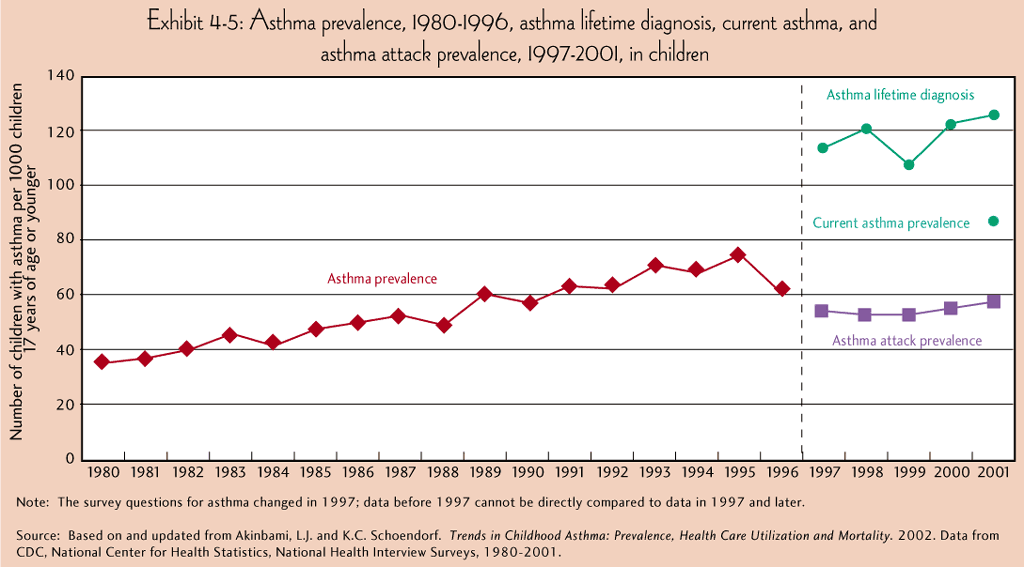
There is a reduced occurrence of asthma in people who were breast-fed as babies. Current research suggests that the prevalence of childhood asthma has been increasing. According to the Centers for Disease Control and Prevention's National Health Interview Surveys, some 9% of US children below 18 years of age had asthma in 2001, compared with just 3.6% in 1980 (see figure). The World Health Organization (WHO) reports that some 8% of the Swiss population suffers from asthma today, compared with just 2% some 25–30 years ago.[5] Although asthma is more common in affluent countries, it is by no means a problem restricted to the affluent; the WHO estimate that there are between 15 and 20 million asthmatics in India. In the U.S., urban residents, Hispanics, and African Americans are affected more than the population as a whole. Globally, asthma is responsible for around 180,000 deaths annually.[5]
On the remote South Atlantic island Tristan da Cunha, 50% of the population are asthmatics due to heredity transmission of a mutation in the gene CC16.
Socioeconomic factors
The incidence of asthma is higher among low-income populations within a society (it is not more common in developed countries than developing countries [2]), which in the western world are disproportionately ethnic minorities, and more likely to live near industrial areas. Additionally, asthma has been strongly associated with the presence of cockroaches in living quarters, which is more likely in such neighborhoods.[6]
Asthma incidence and quality of treatment varies among different racial groups, though this may be due to correlations with income (and thus affordability of health care) and geography. For example, Black Americans are less likely to receive outpatient treatment for asthma despite having a higher prevalence of the disease. They are much more likely to have emergency room visits or hospitalization for asthma, and are three times as likely to die from an asthma attack compared to whites. The prevalence of "severe persistent" asthma is also greater in low-income communities compared with communities with better access to treatment.[7][8]
Asthma and athletics
Asthma appears to be more prevalent in athletes than in the general population. One survey of participants in the 1996 Summer Olympic Games, in Atlanta, Georgia, U.S., showed that 15% had been diagnosed with asthma, and that 10% were on asthma medication. [9] These statistics have been questioned on at least two bases. Athletes with mild asthma may be more likely to be diagnosed with the condition than non-athletes, because even subtle symptoms may interfere with their performance and lead to pursuit of a diagnosis. It has also been suggested that some professional athletes who do not suffer from asthma claim to do so in order to obtain special permits to use certain performance-enhancing drugs.
There appears to be a relatively high incidence of asthma in sports such as cycling, mountain biking, and long-distance running, and a relatively lower incidence in weightlifting and diving. It is unclear how much of these disparities are from the effects of training in the sport, and from self-selection of sports that may appear to minimize the triggering of asthma.[9][10]
In addition, there exists a variant of asthma called exercise-induced asthma that shares many features with allergic asthma. It may occur either independently, or concurrent with the latter. Exercise studies may be helpful in diagnosing and assessing this condition.
Differential diagnosis
Before diagnosing someone as asthmatic, alternative possibilities should be considered. A clinician taking a history should check whether the patient is using any known bronchoconstrictors (substances that cause narrowing of the airways, e.g., certain anti-inflammatory agents or beta-blockers).
Chronic obstructive pulmonary disease, which closely resembles asthma, is correlated with more exposure to cigarette smoke, an older patient, less symptom reversibility after bronchodilator administration (as measured by spirometry), and decreased likelihood of family history of atopy.
Pulmonary aspiration, whether direct due to dysphagia (swallowing disorder) or indirect (due to acid reflux), can show similar symptoms to asthma. However, with aspiration, fevers might also indicate aspiration pneumonia. Direct aspiration (dysphagia) can be diagnosed by performing a Modified Barium Swallow test and treated with feeding therapy by a qualified speech therapist. If the aspiration is indirect (from acid reflux) then treatment directed at this is indicated.
A majority of children who are asthma sufferers have an identifiable allergy trigger. Specifically, in a 2004 study, 71% had positive test results for more than 1 allergen, and 42% had positive test results for more than 3 allergens.[11]
The majority of these triggers can often be identified from the history; for instance, asthmatics with hay fever or pollen allergy will have seasonal symptoms, those with allergies to pets may experience an abatement of symptoms when away from home, and those with occupational asthma may improve during leave from work. Occasionally, allergy tests are warranted and, if positive, may help in identifying avoidable symptom triggers.
After a pulmonary function test has been carried out, radiological tests, such as a chest X-ray or CT scan, may be required to exclude the possibility of other lung diseases. In some people, asthma may be triggered by gastroesophageal reflux disease, which can be treated with suitable antacids. Very occasionally, specialized tests after inhalation of methacholine — or, even less commonly, histamine — may be performed.
Asthma is categorized by the United States National Heart, Lung and Blood Institute as falling into one of four categories: intermittent, mild persistent, moderate persistent and severe persistent. The diagnosis of "severe persistent asthma" occurs when symptoms are continual with frequent exacerbations and frequent nighttime symptoms, result in limited physical activity and when lung function as measured by PEV or FEV1 tests is less than 60% predicted with PEF variability greater than 30%.
Cause
Asthma is caused by a complex interaction of environmental and genetic factors that researchers do not yet fully understand.[12] These factors can also influence how severe a person’s asthma is and how well they respond to medication.[13] As with other complex diseases, many environmental and genetic factors have been suggested as causes of asthma, but not all studies posing such claims have been verified by further studies. In addition, as researchers detangle the complex causes of asthma, it is becoming more evident that certain environmental and genetic factors may affect asthma only when combined.
Environmental
Many environmental risk factors have been associated with asthma development and morbidity in children, but a few stand out as well-replicated or that have a meta-analysis of several studies to support their direct association.
Environmental tobacco smoke, especially maternal cigarette smoking, is associated with high risk of asthma prevalence and asthma morbidity, wheeze, and respiratory infections.[14] Poor air quality, from traffic pollution or high ozone levels, has been repeatedly associated with increased asthma morbidity and has a suggested association with asthma development that needs further research.[14][15]
Caesarean sections have been associated with asthma when compared with vaginal birth; a meta-analysis found a 20% increase in asthma prevalence in children delivered by Cesarean section compared to those who were not. It was proposed that this is due to modified bacterial exposure during Cesarean section compared with vaginal birth, which modifies the immune system (as described by the hygiene hypothesis).[16]
Psychological stress, has long been suspected of being an asthma trigger, but only in recent decades has convincing scientific evidence substantiated this hypothesis. Rather than stress directly causing the asthma symptoms, it is thought that stress modulates the immune system to increase the magnitude of the airway inflammatory response to allergens and irritants.[14][17]
Viral respiratory infections at an early age, along with siblings and day care exposure, may be protective against asthma, although there have been controversial results, and this protection may depend on genetic context.[14][18][19] Antibiotic use early in life has been linked to development of asthma in several examples; it is thought that antibiotics make one susceptible to development of asthma because they modify gut flora, and thus the immune system (as described by the hygiene hypothesis).[20] The hygiene hypothesis is an hypothesis about the cause of asthma and other allergic disease, and is supported by epidemiologic data for asthma. For example, asthma prevalence has been increasing in developed countries along with increased use of antibiotics, c-sections, and cleaning products.[20][16][21] All of these things may negatively affect exposure to beneficial bacteria and other immune system modulators that are important during development, and thus may cause increased risk for asthma and allergy.
Genetic
Over 100 genes have been associated with asthma in at least one genetic association study.[22] However, such studies must be repeated to ensure the findings are not due to chance. Through the end of 2005, 25 genes had been associated with asthma in six or more separate populations:[22]
Template:Multicol-break
Template:Multicol-break
Template:Multicol-break
Template:Multicol-break
Template:Multicol-end Many of these genes are related to the immune system or to modulating inflammation. However, even among this list of highly replicated genes associated with asthma, the results have not been consistent among all of the populations that have been tested.[22] This indicates that these genes are not associated with asthma under every condition, and that researchers need to do further investigation to figure out the complex interactions that cause asthma. One theory is that asthma is a collection of several diseases, and that genes might have a role in only subsets of asthma. For example, one group of genetic differences (single nucleotide polymorphisms in 17q21) was associated with asthma that develops in childhood.[23] Gene-environment InteractionsResearch suggests that some genetic variants may only cause asthma when they are combined with specific environmental exposures, and otherwise may not be risk factors for asthma.[12] The genetic trait, CD14 single nucleotide polymorphism (SNP) C-159T and exposure to endotoxin (a bacterial product) are a well-replicated example of a gene-environment interaction that is associated with asthma. Endotoxin exposure varies from person to person and can come from several environmental sources, including environmental tobacco smoke, dogs, and farms. Researchers have found that risk for asthma changes based on a person’s genotype at CD14 C-159T and level of endotoxin exposure.[24]
Pathophysiology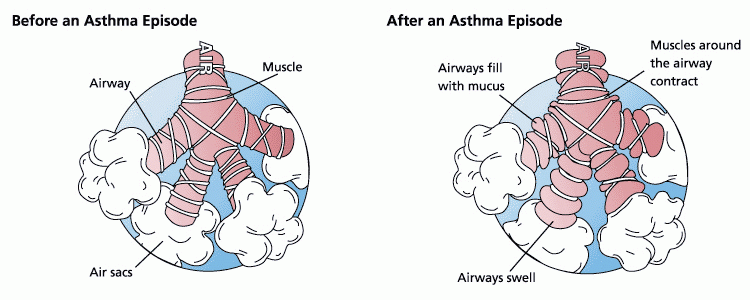 BronchoconstrictionDuring an asthma episode, inflamed airways react to environmental triggers such as smoke, dust, or pollen. The airways narrow and produce excess mucus, making it difficult to breathe. In essence, asthma is the result of an immune response in the bronchial airways.[25] The airways of asthmatics are "hypersensitive" to certain triggers, also known as stimuli (see below). In response to exposure to these triggers, the bronchi (large airways) contract into spasm (an "asthma attack"). Inflammation soon follows, leading to a further narrowing of the airways and excessive mucus production, which leads to coughing and other breathing difficulties. Stimuli
Bronchial inflammationThe mechanisms behind allergic asthma—i.e., asthma resulting from an immune response to inhaled allergens—are the best understood of the causal factors. In both asthmatics and non-asthmatics, inhaled allergens that find their way to the inner airways are ingested by a type of cell known as antigen presenting cells, or APCs. APCs then "present" pieces of the allergen to other immune system cells. In most people, these other immune cells (TH0 cells) "check" and usually ignore the allergen molecules. In asthmatics, however, these cells transform into a different type of cell (TH2), for reasons that are not well understood. The resultant TH2 cells activate an important arm of the immune system, known as the humoral immune system. The humoral immune system produces antibodies against the inhaled allergen. Later, when an asthmatic inhales the same allergen, these antibodies "recognize" it and activate a humoral response. Inflammation results: chemicals are produced that cause the airways to constrict and release more mucus, and the cell-mediated arm of the immune system is activated. The inflammatory response is responsible for the clinical manifestations of an asthma attack. The following section describes this complex series of events in more detail. PathogenesisThe fundamental problem in asthma appears to be immunological: young children in the early stages of asthma show signs of excessive inflammation in their airways. Epidemiological findings give clues as to the pathogenesis: the incidence of asthma seems to be increasing worldwide, and asthma is now very much more common in affluent countries. In 1968 Andor Szentivanyi first described The Beta Adrenergic Theory of Asthma; in which blockage of the Beta-2 receptors of pulmonary smooth muscle cells causes asthma.[29] Szentivanyi's Beta Adrenergic Theory is a citation classic[30] and has been cited more times than any other article in the history of the Journal of Allergy. In 1995 Szentivanyi and colleagues demonstrated that IgE blocks beta-2 receptors.[31] Since overproduction of IgE is central to all atopic diseases, this was a watershed moment in the world of allergy.[32] The Beta-Adrenergic Theory has been cited in the scholarship of such noted investigators as Richard F. Lockey (former President of the American Academy of Allergy, Asthma, and Immunology),[33] Charles Reed (Chief of Allergy at Mayo Medical School),[34] and Craig Venter (Human Genome Project).[35] Many studies have linked asthma, bronchitis, and acute respiratory illnesses to air quality experienced by children.[36] One of the largest of these studies is the California Children's Health Study.[15] From the press release [3] This study showed that children in the high ozone communities who played three or more sports developed asthma at a rate three times higher than those in the low ozone communities. Because participation in some sports can result in a child drawing up to 17 times the “normal” amount of air into the lungs, young athletes are more likely to develop asthma. Note that concentrations of ozone have risen steadily in Europe since 1870. [4] Another theory of pathogenesis is that asthma is a disease of hygiene. In nature, babies are exposed to bacteria and other antigens soon after birth, "switching on" the TH1 lymphocyte cells of the immune system that deal with bacterial infection. If this stimulus is insufficient, as it may be in modern, clean environments, then TH2 cells predominate, and asthma and other allergic diseases may develop. This "hygiene hypothesis" may explain the increase in asthma in affluent populations. The TH2 lymphocytes and eosinophil cells that protect us against parasites and other infectious agents are the same cells responsible for the allergic reaction. Charcot-Leyden crystals are formed when crystalline material in eosinophils coalesce. These crystals are significant in sputum samples of people with asthma. In the developed world, the parasites that eosinophils are programmed to combat are now rarely encountered, but the immune response remains and is wrongly triggered in some individuals by certain allergens. It has been postulated that some forms of asthma may be related to infection, in particular by Chlamydia pneumoniae.[18] This issue remains controversial, as the relationship is not borne out by meta-analysis of the research.[19] The correlation seems to be not with the onset, but rather with accelerated loss of lung function in adults with new onset of non-atopic asthma.[37] One possible explanation is that some asthmatics may have altered immune response that facilitates long-term chlamydia pneumonia infection.[38] The response to targeting with macrolide antibiotics has been investigated, but the temporary benefit reported in some studies may reflect just their anti-inflammatory activities rather than their antimicrobic action.[19] One group of researchers suggested that, in part, asthma has a neurogenic paroxysmal component,[39] and that several anti-eleptic drugs have an effect. However only one paper[40] has been published as listed by PubMed and its conclusions criticized.[41] A study conducted by the National Jewish Medical and Research Center concluded that overweight and obesity are associated with a dose-dependent increase in the odds of incident asthma in men and women, suggesting asthma incidence could be reduced by interventions targeting overweight and obesity. [42] Asthma and sleep apneaIt is recognized with increasing frequency, that patients who have both obstructive sleep apnea (OSA) and bronchial asthma, often improve tremendously when the sleep apnea is diagnosed and treated.[43] CPAP is not effective in patients with nocturnal asthma only.[44] Asthma and gastro-esophageal reflux diseaseIf gastro-esophageal reflux disease is present, the patient may have repetitive episodes of acid aspiration, which results in airway inflammation and "irritant-induced" asthma. GERD may be common in difficult-to-control asthma, but generally speaking, treating it does not seem to affect the asthma.[45] Signs and symptomsIn some individuals asthma is characterized by chronic respiratory impairment. In others it is an intermittent illness marked by episodic symptoms that may result from a number of triggering events, including upper respiratory infection, stress, airborne allergens, air pollutants (such as smoke or traffic fumes), or exercise. Some or all of the following symptoms may be present in those with asthma: dyspnea, wheezing, stridor, coughing, an inability for physical exertion. Some asthmatics that have severe shortness of breath and tightening of the lungs never wheeze or have stridor and their symptoms may be confused with a COPD-type disease. An acute exacerbation of asthma is referred to as an asthma attack. The clinical hallmarks of an attack are shortness of breath (dyspnea) and either wheezing or stridor.[46] Although the former is "often regarded as the sine qua non of asthma,[46] some patients present primarily with coughing, and in the late stages of an attack, air motion may be so impaired that no wheezing may be heard. When present the cough may sometimes produce clear sputum. The onset may be sudden, with a sense of constriction in the chest, breathing becomes difficult, and wheezing occurs (primarily upon expiration, but can be in both respiratory phases). Signs of an asthmatic episode include wheezing, rapid breathing (tachypnea), prolonged expiration, a rapid heart rate (tachycardia), rhonchus lung sounds (audible through a stethoscope), and over-inflation of the chest. During a serious asthma attack, the accessory muscles of respiration (sternocleidomastoid and scalene muscles of the neck) may be used, shown as in-drawing of tissues between the ribs and above the sternum and clavicles, and the presence of a paradoxical pulse (a pulse that is weaker during inhalation and stronger during exhalation). During very severe attacks, an asthma sufferer can turn blue from lack of oxygen, and can experience chest pain or even loss of consciousness. Just before loss of consciousness, there is a chance that the patient will feel numbness in the limbs and palms may start to sweat. Feet may become icy cold. Severe asthma attacks, which may not be responsive to standard treatments (status asthmaticus), are life-threatening and may lead to respiratory arrest and death. Despite the severity of symptoms during an asthmatic episode, between attacks an asthmatic may show few or even no signs of the disease.[47] DiagnosisAsthma is defined simply as reversible airway obstruction. Reversibility occurs either spontaneously or with treatment. The basic measurement is peak flow rates and the following diagnostic criteria are used by the British Thoracic Society:[48]
In many cases, a physician can diagnose asthma on the basis of typical findings in a patient's clinical history and examination. Asthma is strongly suspected if a patient suffers from eczema or other allergic conditions—suggesting a general atopic constitution—or has a family history of asthma. While measurement of airway function is possible for adults, most new cases are diagnosed in children who are unable to perform such tests. Diagnosis in children is based on a careful compilation and analysis of the patient's medical history and subsequent improvement with an inhaled bronchodilator medication. In adults, diagnosis can be made with a peak flow meter (which tests airway restriction), looking at both the diurnal variation and any reversibility following inhaled bronchodilator medication. Testing peak flow at rest (or baseline) and after exercise can be helpful, especially in young asthmatics who may experience only exercise-induced asthma. If the diagnosis is in doubt, a more formal lung function test may be conducted. Once a diagnosis of asthma is made, a patient can use peak flow meter testing to monitor the severity of the disease. In the Emergency Department doctors may use a capnography PMID 16187465 which measures the amount of exhaled carbon dioxide along with pulse oximetry which shows the amount of oxygen dissolved in the blood, to determine the severity of an asthma attack as well as the response to treatment. TreatmentThere is no cure for asthma. Doctors have only found ways to prevent attacks and relieve the symptoms such as tightness of the chest and trouble breathing. The most effective treatment for asthma is identifying triggers, such as pets or aspirin, and limiting or eliminating exposure to them. Desensitization to allergens has been shown to be a treatment option for certain patients.[49] As is common with respiratory disease, smoking is believed to adversely affect asthmatics in several ways, including an increased severity of symptoms, a more rapid decline of lung function, and decreased response to preventive medications.[50] Automobile emissions are considered an even more significant cause and aggravating factor. [5] Asthmatics who smoke or who live near traffic [6] typically require additional medications to help control their disease. Furthermore, exposure of both non-smokers and smokers to wood smoke, gas stove fumes and second-hand smoke is detrimental, resulting in more severe asthma, more emergency room visits, and more asthma-related hospital admissions.[51] Smoking cessation and avoidance of second-hand smoke is strongly encouraged in asthmatics.[52] The specific medical treatment recommended to patients with asthma depends on the severity of their illness and the frequency of their symptoms. Specific treatments for asthma are broadly classified as relievers, preventers and emergency treatment. The Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma (EPR-2)[52] of the U.S. National Asthma Education and Prevention Program, and the British Guideline on the Management of Asthma[53] are broadly used and supported by many doctors. On August 29, 2007 the final Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma was officially released. Bronchodilators are recommended for short-term relief in all patients. For those who experience occasional attacks, no other medication is needed. For those with mild persistent disease (more than two attacks a week), low-dose inhaled glucocorticoids or alternatively, an oral leukotriene modifier, a mast-cell stabilizer, or theophylline may be administered. For those who suffer daily attacks, a higher dose of glucocorticoid in conjunction with a long-acting inhaled β-2 agonist may be prescribed; alternatively, a leukotriene modifier or theophylline may substitute for the β-2 agonist. In severe asthmatics, oral glucocorticoids may be added to these treatments during severe attacks. For those in whom exercise can trigger an asthma attack (exercise-induced asthma), higher levels of ventilation and cold, dry air tend to exacerbate attacks. For this reason, activities in which a patient breathes large amounts of cold air, such as skiing and running, tend to be worse for asthmatics, whereas swimming in an indoor, heated pool, with warm, humid air, is less likely to provoke a response.[46] Researchers at Harvard Medical School (HMS) have come up with convincing evidence that the answer to what causes asthma lies in a special type of natural "killer" cell. This finding means that physicians may not be treating asthma sufferers with the right kinds of drugs. For example, natural killer T cells seem to be resistant to the corticosteroids in widely used inhalers.[54] Relief medicationSymptomatic control of episodes of wheezing and shortness of breath is generally achieved with fast-acting bronchodilators. These are typically provided in pocket-sized, metered-dose inhalers (MDIs). In young sufferers, who may have difficulty with the coordination necessary to use inhalers, or those with a poor ability to hold their breath for 10 seconds after inhaler use (generally the elderly), an asthma spacer (see top image) is used. The spacer is a plastic cylinder that mixes the medication with air in a simple tube, making it easier for patients to receive a full dose of the drug and allows for the active agent to be dispersed into smaller, more fully inhaled bits. A nebulizer which provides a larger, continuous dose can also be used. Nebulizers work by vaporizing a dose of medication in a saline solution into a steady stream of foggy vapour, which the patient inhales continuously until the full dosage is administered. There is no clear evidence, however, that they are more effective than inhalers used with a spacer. Nebulizers may be helpful to some patients experiencing a severe attack. Such patients may not be able to inhale deeply, so regular inhalers may not deliver medication deeply into the lungs, even on repeated attempts. Since a nebulizer delivers the medication continuously, it is thought that the first few inhalations may relax the airways enough to allow the following inhalations to draw in more medication. Relievers include:
Prevention medicationCurrent treatment protocols recommend prevention medications such as an inhaled corticosteroid, which helps to suppress inflammation and reduces the swelling of the lining of the airways, in anyone who has frequent (greater than twice a week) need of relievers or who has severe symptoms. If symptoms persist, additional preventive drugs are added until the asthma is controlled. With the proper use of prevention drugs, asthmatics can avoid the complications that result from overuse of relief medications. Asthmatics sometimes stop taking their preventive medication when they feel fine and have no problems breathing. This often results in further attacks, and no long-term improvement. Preventive agents include the following.
Additionally, the antidepressant tianeptine has shown significant efficacy in children with asthma. Long-acting β2-agonists Long-acting bronchodilators (LABD) are similar in structure to short-acting selective beta2-adrenoceptor agonists, but have much longer sidechains resulting in a 12-hour effect, and are used to give a smoothed symptomatic relief (used morning and night). While patients report improved symptom control, these drugs do not replace the need for routine preventers, and their slow onset means the short-acting dilators may still be required. In November of 2005, the American FDA released a health advisory alerting the public to findings that show the use of long-acting β2-agonists could lead to a worsening of symptoms, and in some cases death.[58] Currently available long-acting beta2-adrenoceptor agonists include salmeterol, formoterol, bambuterol, and sustained-release oral albuterol. Combinations of inhaled steroids and long-acting bronchodilators are becoming more widespread; the most common combination currently in use is fluticasone/salmeterol (Advair in the United States, and Seretide in the United Kingdom). Another combination is budesonide/formoterol which is commercially known as symbicort. A recent meta-analysis of the roles of long-acting beta-agonists may indicate a danger to asthma patients. "These agents can improve symptoms through bronchodilation at the same time as increasing underlying inflammation and bronchial hyper-responsiveness, thus worsening asthma control without any warning of increased symptoms," said Shelley Salpeter in a Cornell study. The study goes on to say that "Three common asthma inhalers containing the drugs salmeterol or formoterol may be causing four out of five US asthma-related deaths per year and should be taken off the market".[59] This assertion has drawn criticism from many asthma specialists for being inaccurate. As Dr. Hal Nelson points out in a recent letter to the Annals of Internal Medicine, Dr. Salpeter has since tempered her comments regarding LABAs. Emergency treatmentWhen an asthma attack is unresponsive to a patient's usual medication, other treatments are available to the physician or hospital:[60]
Alternative and complementary medicineMany asthmatics, like those who suffer from other chronic disorders, use alternative treatments; surveys show that roughly 50% of asthma patients use some form of unconventional therapy.[62][63] There are little data to support the effectiveness of most of these therapies. A Cochrane systematic review of acupuncture for asthma found no evidence of efficacy.[64] A similar review of air ionisers found no evidence that they improve asthma symptoms or benefit lung function; this applied equally to positive and negative ion generators.[65] A study of "manual therapies" for asthma, including osteopathic, chiropractic, physiotherapeutic and respiratory therapeutic maneuvers, found there is insufficient evidence to support or refute their use in treating asthma;[66] these maneuvers include various osteopathic and chiropractic techniques to "increase movement in the rib cage and the spine to try and improve the working of the lungs and circulation"; chest tapping, shaking, vibration, and the use of "postures to help shift and cough up phlegm." On the other hand, one meta-analysis found that homeopathy has a potentially mild benefit in reducing symptom intensity;[67] however, the number of patients involved in the analysis was small, and subsequent studies have not supported this finding.[68] Several small trials have suggested some benefit from various yoga practices, ranging from integrated yoga programs[69] —"yogasanas, Pranayama, meditation, and kriyas"—to sahaja yoga,[70] a form of meditation. The Buteyko method, a Russian therapy based on breathing exercises, has been investigated. A randomized, controlled trial of just 39 patients in 1998 showed a substantial reduction in the need for beta-agonists and a 50% reduction in the need for inhaled steroids. Quality of life scores improved significantly as people were less afraid of their condition and more confident of the future. Lung function remained the same despite the decrease in medication.[71] A trial in New Zealand in 2000 showed an 85% reduction in the use of beta-agonist medication and a 50% reduction in inhaled steroid use after six months.[72] Given that some research has identified a negative association between helminth infection (hookworm) and asthma and hay fever,[73] some have suggested that hookworm infestation, although not medically sanctioned, would cure asthma. There is both anectdotal evidence[74] and peer-reviewed research to support this viewpoint. [75] Guaifenesin, an expectorant available over the counter, may have a small effect in managing thickened bronchial mucus. PrognosisThe prognosis for asthmatics is good; especially for children with mild disease. For asthmatics diagnosed during childhood, 54% will no longer carry the diagnosis after a decade. The extent of permanent lung damage in asthmatics is unclear. Airway remodelling is observed, but it is unknown whether these represent harmful or beneficial changes.[25] Although conclusions from studies are mixed, most studies show that early treatment with glucocorticoids prevents or ameliorates decline in lung function as measured by several parameters.[76] For those who continue to suffer from mild symptoms, corticosteroids can help most to live their lives with few disabilities. The mortality rate for asthma is low, with around 6000 deaths per year in a population of some 10 million patients in the United States.[46] Better control of the condition may help prevent some of these deaths. See also
References
External links
Template:Respiratory pathology Template:SIB ar:ربو zh-min-nan:He-ku ca:Asma cs:Astma cy:Asthma da:Astma de:Asthma bronchiale el:Άσθμα et:Bronhiaalastma eo:Astmo eu:Asma gl:Asma ko:천식 hr:Astma id:Asma ia:Asthma is:Astmi it:Asma he:אסתמה lt:Astma hu:Asztma mk:Астма nl:Astma no:Astma nn:Astma qu:Qharqayuy simple:Asthma sk:Astma sl:Astma sr:Астма su:Asma fi:Astma sv:Astma uk:Астма ur:دمہ wa:Coûtresse d' alinne |
- Pages with reference errors
- CS1 maint: Multiple names: authors list
- CS1 errors: dates
- CS1 maint: Explicit use of et al.
- Pages with citations using unsupported parameters
- CS1 maint: Extra text: editors list
- CS1 maint: Extra text
- Asthma
- Diseases
- Emergency medicine
- Pulmonology
- Intensive care medicine
- Mature chapter