Assisted reproductive technology: Difference between revisions
Ochuko Ajari (talk | contribs) No edit summary |
Ochuko Ajari (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{SI}} | {{SI}} | ||
{{CMG}} | |||
==Overview== | ==Overview== | ||
Latest revision as of 16:11, 5 November 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Assisted reproductive technology (ART) is a general term referring to methods used to achieve pregnancy by artificial or partially artificial means. It is reproductive technology used in infertility treatment, which is the only application routinely used today of reproductive technology. While there is no consensus on the definition, generally the process of intercourse is bypassed either by insemination (example IUI) or fertilization of the oocytes in the laboratory environment (i.e. in IVF).
Medical procedures
Most fertility medication are agents that stimulate the development of follicles in the ovary. Examples are gonadotropins and gonadotropin releasing hormone.
Manual procedures
To this category counts all forms of ART techniques that uses more substantial and forceful interventions than giving medication. In vitro fertilisation (IVF) and expansions of it (e.g. OCR, AZH, ICSI, ZIFT) are the most prevalent. However, there are also other manual ART, not necessarily dependent on IVF (e.g. PGD, GIFT, SSR).
In vitro fertilisation
In vitro fertilisation (IVF) is the technique of letting fertilisation of the male and female gametes (sperm and egg) occur outside the female body.
Expansions of IVF
The following are techniques that are involved in or requires in vitro fertilisation. On the other hand, in vitro fertilization doesn't necessarily involve each technique.
Transvaginal Ovum Retrieval (OCR)
This is the process whereby a small needle is inserted through the back of the vagina and guided via ultrasound into the ovarian follicles to collect the fluid that contains the eggs.
Assisted zona hatching (AZH)
Assisted zona hatching is performed shortly before the embryo is transferred to the uterus. A small opening is made in the outer layer surrounding the egg in order to help the embryo hatch out and aid in the implantation process of the growing embryo.
Intracytoplasmic Sperm Injection (ICSI)
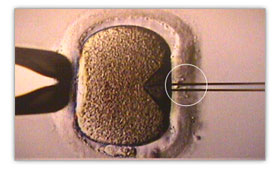
Intracytoplasmic sperm injection is beneficial in the case of male factor infertility where sperm counts are very low or failed fertilization occurred with previous IVF attempt(s). The ICSI procedure involves a single sperm carefully injected into the center of an egg using a microneedle.
Autologous Endometrial Coculture
Autologous endometrial coculture is a possible treatment for patients who have failed previous IVF attempts or who have poor embryo quality. The patient’s fertilized eggs are placed on top of a layer of cells from the patient’s own uterine lining, creating a more natural environment for embryo development.
Zygote intrafallopian transfer (ZIFT)
In zygote intrafallopian transfer egg cells are removed from the woman's ovaries and fertilized in the laboratory; the resulting zygote is then placed into the fallopian tube.
Egg Donor
Egg donors are resources for women with no eggs due to surgery, chemotherapy, or genetic causes; or with poor egg quality, previously unsuccessful IVF cycles or advanced maternal age. In the egg donor process, eggs are retrieved from a donor’s ovaries, fertilized in the laboratory with the sperm from the recipient’s partner, and the resulting healthy embryos are returned to the recipient’s uterus.
Gestational Carrier
A gestational carrier an option when a patient’s medical condition prevents safe pregnancy or when a patient has ovaries but no uterus due to congenital absence or previous surgical removal.
Cryopreservation
Eggs, sperm and reproductive tissue can be preserved for later IVF.
Complementary or alternative medicine
Acupuncture, complementary medicines and hypnosis has shown positive with IVF in occasional studies, but no ones without subsequent criticism. There is no definitive positive effect of any complementary or alternative medicine on IVF.
Others
The following Assisted Reproduction techniques don't necessarily involve IVF.
Gamete intrafallopian transfer (GIFT)
In gamete intrafallopian transfer a mixture of sperm and eggs is placed directly into a woman’s fallopian tubes using laparoscopy following a transvaginal ovum retrieval.
Preimplantation genetic diagnosis (PGD)
PGD involves the use of Fluorescent In Situ Hybridization (FISH) or Polymerase Chain Reaction (PCR) DNA amplification to help identify genetically abnormal embryos and improve healthy outcomes.
Artificial insemination
Artificial insemination (AI) is when sperm is placed into a female's uterus (intrauterine) or cervix (intracervical) using artificial means rather than by natural copulation.
Therapeutic Donor Insemination
Therapeutic donor is an expansion of artificial insemination. It is also called artificial insemination by donor and is used in situations where the woman doesn't have a partner with functional sperm. Instead, a sperm donor supplies the sperm.
Surgical sperm retrieval (SSR)
The reproductive urologist may obtain sperm from the vas deferens, epididymis or directly from the testis in a short outpatient procedure. [1]
Tuboplasty
Tuboplasty is a surgery to restore potency of obstructed fallopian tubes.
Frozen embryo transfer
A fertilized embryo can be cryopreserved. The latter insertion in he body is by the technique Frozen embryo transfer (FET).
Mind/Body Medicine
Mind/Body Medical approaches to infertility reduce psychological distress which often accompanies infertility. A reduction in distress (e.g., depression, anxiety) is found to be associated with improved fertility rates both with traditional medical procedures and without. These approaches typically focus on techniques such as relaxation, stress reduction, cognitive restructuring and mindfulness.
Risks
The majority of IVF-conceived infants do not have birth defects.[2] However, some studies have suggested that assisted reproductive technology is associated with an increased risk of birth defects.[3][4] In the largest U.S. study, which used data from a statewide registry of birth defects,[5] 6.2% of IVF-conceived children had major defects, as compared with 4.4% of naturally conceived children matched for maternal age and other factors (odds ratio, 1.3; 95% confidence interval, 1.00 to 1.67).[2]
Costs
United States of America
Not everyone in the U.S. has insurance coverage for fertility investigations and treatments. Many states are starting to mandate coverage, and the rate of utilization is 277% higher in states with complete coverage. [6]
There are some health insurance companies that cover diagnosis of infertility but frequently once diagnosed will not cover any treatment costs.
2005 approximate treatment/diagnosis costs (United States, costs in US$):
- Initial workup: hysteroscopy, hysterosalpingogram, blood tests ~$2,000
- Artificial insemination ~ $200- 900 per. trial
- Sonohysterogram (SHG) ~ $600 - 1,000
- Clomiphene citrate cycle ~ $ 200 - 500
- IVF cycle ~ $10,000 -30,000
- Use of a surrogate mother to carry the child - dependent on arrangements
Another way to look at costs is to determine the cost of establishing a pregnancy. Thus if a clomiphene treatment has a chance to establish a pregnancy in 8% of cycles and costs $500, it will cost ~ $6,000 to establish a pregnancy, compared to an IVF cycle (cycle fecundity 40%) with a corresponding cost of ($12,000/40%) $30,000.
United Kingdom
In the UK all patients have the right to preliminary testing, provided free of charge by the National Health Service. However, treatment is not widely available on the NHS and there can be long waiting lists. Most patients therefore seek help from private clinics[7].
Sweden
In Sweden, at official fertility clinics most necessary treatments and initial workup etc. is charged with normal patient fee (less than $50). This includes e.g.:
- Cryopreservation of semen, if there is risk that an operation or disease might harm the testes[8].
- Artificial insemination (AID or AIH), if the couple are unable to achieve pregnancy naturally and hasn't got any children since before. [9]
- Egg donor, with the same rules as above.
However, there are long waiting lists, especially for egg donations, since the donor gets just as low reward as the receiving couple are charged. However, almost all treatments have long waiting lists, to compensate for how would otherwise burden the health care system. Therefore, there are also private fertility clinics additionally. The prices here could be e.g. (by corresponding prices from SEK as of October 2007):
- Standard-IVF: $3600. Second attempt: $3300. [10]
- Kostnad för ICSI: $4300. Second attempt: $3900[10]
- Fertility investigation: $825[10]
- Cryopreservation of semen: $225 for two samples, $75 for each additional one[8]
- Reinsertion of embryo: $1300 [11]
- PESA/TESE: $750 [11]
See also
References
- ↑ Abington Reproductive Medicine: ART (2006)
- ↑ 2.0 2.1 Van Voorhis BJ (2007). "Clinical practice. In vitro fertilization". N Engl J Med. 356 (4): 379–86. PMID 17251534.
- ↑ Kurinczuk JJ, Hansen M, Bower C (2004). "The risk of birth defects in children born after assisted reproductive technologies". Curr Opin Obstet Gynecol. 16 (3): 201–9. PMID 15129049.
- ↑ Hansen M, Bower C, Milne E, de Klerk N, Kurinczuk JJ (2005). "Assisted reproductive technologies and the risk of birth defects--a systematic review" (PDF). Hum Reprod. 20 (2): 328–38. PMID 15567881.
- ↑ Olson CK, Keppler-Noreuil KM, Romitti PA, Budelier WT, Ryan G, Sparks AE, Van Voorhis BJ (2005). "In vitro fertilization is associated with an increase in major birth defects". Fertil Steril. 84 (5): 1308–15. PMID 16275219.
- ↑ Jain T, Harlow BL, Hornstein MD. "Insurance coverage and outcome of in vitro fertilization." New England Journal of Medicine. 347(9):661-6.
- ↑ Infertility Treatment, NHS Direct Online (NHS Direct Online Health Enyclopaedia)
- ↑ 8.0 8.1 Karolinska (Swedish)
- ↑ RMC Skåne (Swedish)
- ↑ 10.0 10.1 10.2 Fertilitetscentrum - Stockholm (Swedish)
- ↑ 11.0 11.1 CvLK (Swedish)
External links
- Buying babies, bit by bit, From The Economist. Prices and costs of ART
- Mind/Body Medicine Research for Infertility
de:Künstliche Befruchtung no:Assistert befruktning fi:Hedelmöityshoito