Asherman's syndrome
| Ashermans syndrome | |
| ICD-10 | N85.6 |
|---|---|
| ICD-9 | 621.5 |
| DiseasesDB | 946 |
| MedlinePlus | 001483 |
| MeSH | D006175 |
Editor-In-Chief: Canan S Fornusek, PhD [1]
Associate Editor-In-Chief: M.Umer Tariq [2]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview

Asherman's syndrome (AS), also called "uterine synechiae" or intrauterine adhesions (IUA), presents a condition characterized by the presence of adhesions and/or fibrosis within the uterine cavity due to scars. A number of other terms have been used to describe the condition and related conditions including: traumatic intrauterine adhesions, uterine/cervical atresia, traumatic uterine atrophy, sclerotic endometrium, endometrial sclerosis. In this article AS and IUA are used interchangeably.
Causes and features

The cavity of the uterus is lined by the endometrium. This lining is composed of two layers, the functional layer which is shed during menstruation and an underlying basal layer which is necessary for regenerating the functional layer. Trauma to the basal layer, typically after a dilation and curettage (D&C) performed after a miscarriage, or delivery, or for elective abortion can lead to the development of intrauterine scars resulting in adhesions which can obliterate the cavity to varying degrees. In the extreme, the whole cavity has been scarred and occluded. Even with relatively few scars, the endometrium may fail to respond to estrogens and rests. Often, patients experience secondary menstrual irregularities characterized by changes in flow and duration of bleeding (amenorrhea, hypomenorrhea, or oligomenorrhea)[1] and become infertile. Menstrual anomlies are often but not always correlated with severity: adhesions restricted to only the cervix or lower uterus may block menstruation. Pain during menstruation and ovulation are also sometimes experienced, and can be attributed to blockages.
Asherman's syndrome occurs most frequently after a D&C is performed on a recently pregnant uterus, following a missed or incomplete miscarriage, birth, or elective termination (abortion) to remove retained products of conception/placental remains. As the same procedure is used in all three situations, Asherman's can result in all of the above circumstances. It affects women of all races and ages as there is no underlying predisposition or genetic basis to its development. According to a study on 1900 patients with Asherman's syndrome, over 90% of the cases occurred following pregnancy-related curettage.[2] Depending on the degree of severity, Asherman's syndrome may result in infertility, repeated miscarriages, pain from trapped blood, and future obstetric complications[3](see Prognoses below). There is evidence that left untreated, the obstruction of menstrual flow resulting from scarring can lead to endometriosis.[4]
Asherman's can also result from other pelvic surgeries including Cesarean sections,[2][5] removal of fibroid tumours (myomectomy) and from other causes such as IUDs, pelvic irradiation, schistosomiasis[6] and genital tuberculosis.[7] Chronic endometritis from genital tuberculosis is a significant cause of severe IUA in the developing world, often resulting in total obliteration of the uterine cavity which is difficult to treat.[8]
An artificial form of Asherman's syndrome can be surgically induced by endometrial ablation in women with excessive uterine bleeding, in lieu of hysterectomy.
Incidence
It is estimated that up to 5% of D&Cs result in Asherman's. More conservative estimates put this rate at 1%. Asherman's results from 25% of D&Cs performed 1-4 weeks post-partum[9],[10][4] 30.9% of D&Cs performed for missed miscarriages and 6.4% of D&Cs performed for incomplete miscarriages.[11] In the case of missed miscarriages, the time period between fetal demise and curettage increases the likelihood of adhesion formation to over 30.9%[2][12] The risk of Asherman's also increases with the number of procedures: one study estimated the risk to be 16% after one D&C and 32% after 3 or more D&Cs.[13]
Prevalence in the general population
The true prevalence of Asherman's syndrome is unclear as many doctors are unaware of the symptoms or diagnosis. Increased awareness about the condition and its diagnosis is also expected to reveal a higher frequency than previously reported. The condition was found in 1.5% of women undergoing HSG,[14] between 5 and 39% of women with recurrent miscarriage[15][16][17] and up to 40% of patients who have undergone D&C for retained products of conception.[18]
Diagnosis
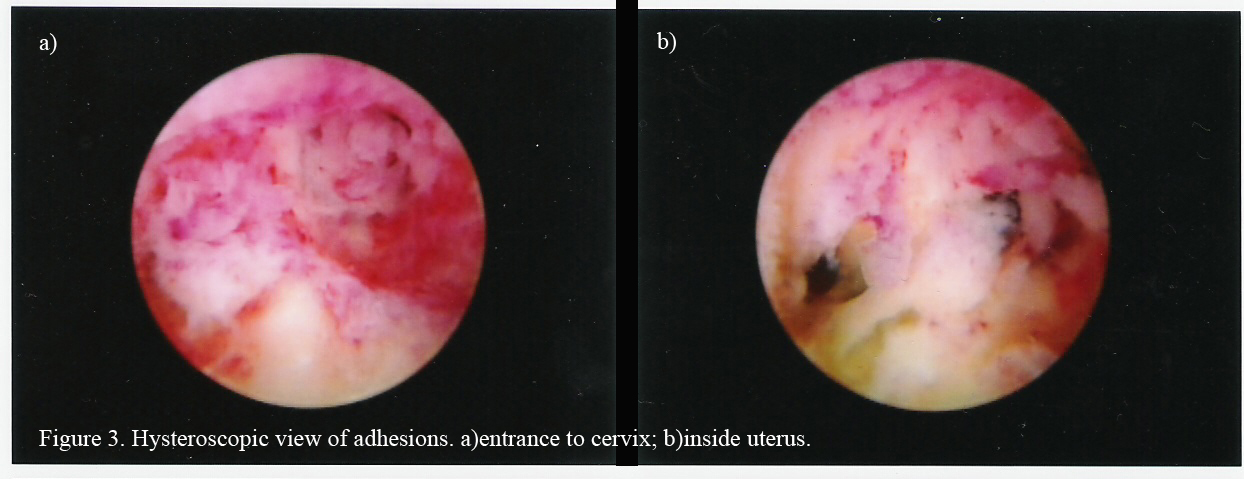
The history of a pregnancy event followed by a D&C leading to secondary amenorrhea is typical. Hysteroscopy is the gold standard for diagnosis.[3] Imaging by sonohysterography or hysterosalpingography will reveal the extent of the scar formation. Ultrasound is not a reliable method of diagnosing Asherman's Syndrome. Hormone studies show normal levels consistent with reproductive function.
Treatment
Fertility can be restored by removal of adhesions, depending on the severity of the initial trauma and other individual patient factors. Fluoroscopically guided operative hysteroscopy is used for visual inspection of the uterine cavity and dissection of scar tissue (adhesiolysis). In more severe cases, laparoscopy is used in addition to hysteroscopy as a protective measure against uterine perforation. Microscissors are usually used to cut adhesions. Electrocauterization is not recommended.[19] Sometimes a balloon stent such as a Cook Medical Balloon Uterine Stent filled with saline is inserted in the uterus for up to 3 weeks to keep the walls of the uterus apart as they heal to prevent the reformation of adhesions.
Hormonal therapy with synthetic or conjugated estrogen is usually prescribed following surgery to stimulate endometrial growth thereby preventing the walls of the uterus from re-adhering.
More studies are needed to evaluate which method of treatment is most likely to have a successful outcome.
Follow-up tests (HSG, hysteroscopy or SHG) are necessary to ensure that scars have not reformed. Further surgery may be necessary to restore a normal uterine cavity. According to a recent study among 61 patients, the overall rate of adhesion recurrence was 27.9% and in severe cases this was 41.9%.[20] Another study found that postoperative adhesions reoccur in close to 50% of severe Asherman's and in 21.6% of moederate cases.[3] Mild IUA unlike moderate to severe synechiae do not appear to reform.
Classification of IUA
As severity of the condition correlates with prognosis, classification of IUA is useful for choosing the treatment method and providing a prognosis relating to fertility outcome following treatment. Several classification systems have been proposed for Asherman’s syndrome, although none of them is currently endorsed universally. The older systems were based on hysterosalpingography findings however with the advent of hysteroscopy modern classification systems are based on hysteroscopic diagnosis of adhesions. Those of the American Fertility Society [21] , the European Society for Hysteroscopy [22]and Nasr's proposed system [23] are the most complex, taking into account several criteria. There is variation between criteria used in these systems but they include type of adhesions, location, extent of the uterine cavity affected, clinical symptoms, menstrual characteristics or history, and/or obstetric history. The precision in these systems may make them difficult to apply in practice because the boundaries between grade subtypes are sometimes subtle. None of these classification systems have been validated by clinical studies, and research reporting treatment outcomes often lack details on exact IUA grades in patients. This adds to the difficulties in comparing study outcomes in patients treated for Asherman's syndrome.
Prognosis
The extent of scar formation is critical. Small scars can usually be treated with success. Extensive obliteration of the uterine cavity or fallopian tube openings (ostia) may require several surgical interventions or even be uncorrectable. In this case surrogacy, IVF or adoption may be advised.
Patients who carry a pregnancy after correction of Asherman's syndrome may have an increased risk of having abnormal placentation including placenta accreta[24] where the placenta invades the uterus more deeply, leading to complications in placental separation after delivery. Premature delivery,[25] second-trimester pregnancy loss,[26] and uterine rupture[27] are other reported complications. They may also develop incompetent cervix where the cervix can no longer support the growing weight of the fetus, the pressure causes the placenta to rupture and the mother goes into premature labour. Cerclage is a surgical stitch which helps support the cervix if needed.[26]
The overall pregnancy rate after adhesiolysis was 60% and the live birth rate was 38.9% according to one study.[28] Success is related to the severity of the adhesions with 93, 78, and 57% pregnancies achieved after treatment of mild, moderate and severe adhesions, respectively and resulting in 81, 66, and 32% live birth rates, respectively.[3]
Age is another factor contributing to fertility outcomes after treatment of Asherman's. For women under 35 years of age treated for severe adhesions, pregnancy rates were 66.6% compared to 23.5% in women older than 35.[24]
Prevention
Asherman's need not be caused by an 'over-aggressive' D&C:the recently pregnant uterus is particularly soft and easily injured. Medical alternatives to D&C for evacuation of retained placenta/products of conception exist including misoprostol methotrexate and mifepristone. Studies show this less invasive and cheaper method to be efficacious, safe and an acceptable alternative to surgical management for most women.[29][30] It was suggested as early as in 1993[13] that the incidence of IUA might be lower following medical evacuation (eg. Misoprostol) of the uterus, thus avoiding any intrauterine instrumentation. So far, one study supports this proposal, showing that women who were treated for missed miscarriage with misoprostol did not develop IUA, while 7.7% of those undergoing D&C did.[31] The advantage of misoprostol is that it can be used for evacuation not only following miscarriage, but also following birth for retained placenta or hemorrhaging.
Alternatively, D&C could be performed under ultrasound guidance rather than blind procedure. This would enable the surgeon to end scraping the lining when all retained tissue has been removed, avoiding injury.
Early monitoring during pregnancy to identify miscarriage can prevent the development of, or as the case may be, the recurrence of Asherman's as adhesions are more likely to occur after a D&C the longer the period after fetal death.[2] Therefore immediate evacuation following fetal death may prevent IUA.
The use of hysteroscopic surgery instead of D&C to remove retained products of conception or placenta is another alternative, although it could be ineffective if tissue is abundant. Also, hysteroscopy is not a widely or routinely-used technique and requires expertise.
There is no data to indicate that suction D&C is less likely than sharp curette to result in Asherman's. A recent article describes three cases of women who developed intrauterine adhesions following manual vacuum aspiration.[32]
History
It was first described in 1894 by Heinrich Fritsch (Fritsch, 1894)[33] and further characterized by the gynecologist Joseph Asherman in 1948.[34]
It is also known as Fritsch syndrome, or Fritsch-Asherman syndrome.
References
- ↑ Klein SM, Garcia C-R (1973). "Asherman's syndrome: a critique and current review". Fertility and Sterility. 24 (9): 722–735. PMID 4725610.
- ↑ 2.0 2.1 2.2 2.3 Schenker JG, Margalioth EJ. (1982). "Intra-uterine adhesions: an updated appraisal". Fertility Sterility. 37 (5): 593–610. PMID 6281085.
- ↑ 3.0 3.1 3.2 3.3 Valle RF, and Sciarra JJ (1988). "Intrauterine adhesions: Hystreoscopic diagnosis, classification, treatment and reproductive outcome". . Am J Obstet. 158 (6Pt1): 1459–1470. PMID 3381869.
- ↑ 4.0 4.1 Buttram VC, Turati, G (1977). "Uterine synechiae: variations in severity and some conditions which may be conducive to severe adhesions". Int J Fertil. 22 (2): 98–103. PMID 20418.
- ↑ Rochet Y, Dargent D, Bremond A, Priou G, Rudigoz RC (1979). "The obstetrical outcome of women with surgically treated uterine synechiae (in French)". J Gynecol Obstet Biol Reprod. 8 (8): 723–726. PMID 553931.
- ↑ Krolikowski A, Janowski K, Larsen JV. (1995). "Asherman syndrome caused by schistosomiasis". Obstet Gynecol. 85 (5Pt2): 898–9. doi:10.1016/0029-7844(94)00371-J. PMID 7724154.
- ↑ Netter AP, Musset R, Lambert A Salomon Y (1956). "Traumatic uterine synechiae: a common cause of menstrual insufficiency, sterility, and abortion". Am J Obstet Gynecol. 71 (2): 368–75. PMID 13283012.
- ↑ Bukulmez O, Yarali H, Gurgan T. (1999). "Total corporal synechiae due to tuberculosis carry a very poor prognosis following hysteroscopic synechialysis". Hum Reprod. 14 (8): 1960–1961. doi:10.1093/humrep/14.8.1960. PMID 10438408.
- ↑ Parent B, Barbot J, Dubuisson JB. Uterine synechiae (in French). Encyl Med Chir Gynecol 1988; 140A (Suppl): 10-12.
- ↑ Rochet Y, Dargent D, Bremond A, Priou G, Rudigoz RC (1979). "The obstetrical outcome of women with surgically treated uterine synechiae (in French)". J Gynecol Obstet Biol Reprod. 8 (8): 723–726. PMID 553931.
- ↑ Adoni A, Palti Z, Milwidsky A, Dolberg M. (1982). "The incidence of intrauterine adhesions following spontaneous abortion". Int J Fertil. 27 (2): 117–118. PMID 6126446.
- ↑ Fedele L, Bianchi S, Frontino G. Septums and synechiae: approaches to surgical correction. Clin Obstet Gynecol 2006; 49:767-788.
- ↑ 13.0 13.1 Friedler S, Margalioth EJ, Kafka I, Yaffe H. (1993). "Incidence of postabortion intra-uterine adhesions evaluated by hysteroscopy: a prospective study". Hum Reprod. 8 (3): 442–444. PMID 8473464. Text "doi" ignored (help)
- ↑ Dmowski WP, Greenblatt RB. (1969). "Asherman's syndrome and risk of placenta accreta". Obstet Gynecol. 34 (2): 288–299. PMID 5816312.
- ↑ Rabau E, David A. (1963). "Intrauterine adhesions:etiology, prevention, and treatment". Obstet Gynecol. 22: 626–629. PMID 14082285.
- ↑ Toaff R. (1966). "Some remarks on posttraumatic uterine adhesions.in French". Rev Fr Gynecol Obstet. 61 (7): 550–552. PMID 5940506.
- ↑ Ventolini G, Zhang M, Gruber J. (2004). "Hysteroscopy in the evaluation of patients with recurrent pregnancy loss: a cohort study in a primary care population". Surg Endosc. 18 (12): 1782–1784. doi:10.1007/s00464-003-8258-y. PMID 15809790.
- ↑ Westendorp ICD, Ankum WM, Mol BWJ, Vonk J. (1998). "Prevalence of Asherman's syndrome after secondary removal of placental remnants or a repeat curettage for incomplete abortion". Hum Reprod. 13 (12): 3347–3350. doi:10.1093/humrep/13.12.3347. PMID 9886512.
- ↑ Kodaman PH, Arici AA. (2007). "Intra-uterine adhesions and fertility outcome: how to optimize success?". Curr Opin Obstet Gynecol. 19 (3): 207–214. PMID 17495635.
- ↑ Yu D, Li T, Xia E, Huang X, Peng X. (2008). "Factors affecting reproductive outcome of hysteroscopic adhesiolysis for Asherman's syndrome". Fertility and Sterility. 89 (3): 715–722. doi:10.1016/j.fertnstert.2007.03.070. PMID 17681324.
- ↑ American Fertility Society (1988). "The American Fertility Society classification of adnexal adhesions, distal tubal occlusions secondary to tubal ligation, tubal pregnancy, mullerian anomalies and intrauterine adhesions". Fertil Steril. 49 (6): 944–55. PMID 3371491.
- ↑ {{cite journal |author=Wamsteker K, DeBlok SJ |title=Diagnostic hysteroscopy: technique and documentation. |journal=Endoscopic surgery for gynecologist New York:Lippincott Williams & Wilkins Publishers |pages=263-76 |year=1995
- ↑ Nasr AL, AL-Inany HG, Thabet SM, Aboulghar M (2000). "A clinicohysteroscopic scoring system of intrauterine adhesions". Gynecol Obstet Invest. 50 (3): 178–81.
- ↑ 24.0 24.1 Fernandez H, Al Najjar F, Chauvenaud-Lambling; et al. (2006). "Fertility after treatment of Asherman's syndrome stage 3 and 4". J Minim Invasive Gynecol. 13 (5): 398–402. doi:10.1016/j.jmig.2006.04.013. PMID 16962521.
- ↑ Roge, P (1996). "Hysteroscopic management of uterine synechiae: a series of 102 observations". Eur J Obstet Gynecol Reprod Biol. 65 (2): 189–193. doi:10.1016/0301-2115(95)02342-9. PMID 8730623.
- ↑ 26.0 26.1 Capella-Allouc S, Morsad F, Rongieres-Bertrand C; et al. (1999). "Hysteroscopic treatment of severe Asherman's syndrome and subsequent fertility". Hum Reprod. 14 (5): 1230–1233. doi:10.1093/humrep/14.5.1230. PMID 10325268.
- ↑ Deaton JL, Maier D, Andreoli J. (1989). "Spontaneous uterine rupture during pregnancy after treatment of Asherman's syndrome". Am J Obstet Gynecol. 160 ((5Pt1)): 1053–1054. PMID 2729381.
- ↑ Siegler AM, Valle RF. (1988). "Therapeutic hysteroscopic procedures". Fertil Steril. 50 (5): 685–701. PMID 3053254.
- ↑ Zhang J, Gilles JM, Barnhart K, Creinin MD, Westhoff C, Frederick MM (2005). "National Institute of Child Health Human Development (NICHD) Management of Early Pregnancy Failure Trial. A comparison of medical management with misoprostol and surgical management for early pregnancy failure". N Engl J Med. 353 (8): 761–9. PMID 16120856.
- ↑ Weeks A, Alia G, Blum J, Winikoff B, Ekwaru P, Durocher J, Mirembe F. (2005). "A randomized trial of misoprostol compared with manual vacuum aspiration for incomplete abortion". Obstet Gynecol. 106 (3): 540–7. PMID 16135584.
- ↑ Tam WH, Lau WC, Cheung LP, Yuen PM, Chung TK. (2002). "Intrauterine adhesions after conservative and surgical management of spontaneous abortion". J Am Assoc Gynecol Laparosc. 9 (2): 182–185. doi:10.1016/S1074-3804(05)60129-6. PMID 11960045.
- ↑ Dalton VK, Saunders NA, Harris LH, Williams JA, Lebovic DI (2006). "Intrauterine adhesions after manual vacuum aspiration for early pregnancy failure". Fertil. Steril. 85 (6): 1823.e1–3. doi:10.1016/j.fertnstert.2005.11.065. PMID 16674955.
- ↑ >Template:WhoNamedItFritsch H, Ein Fall von volligem Schwaund der Gebormutterhohle nach Auskratzung. Zentralbl Gynaekol 1894; 18:1337-1342.
- ↑ Asherman JG. (1948.). "Traumatic intra-uterine adhesions". J Obstet Gynaecol Br Em. 55 (2): 2–30. Check date values in:
|year=(help)
External links
- Global Library of Women's Medicine; Intrauterine adhesions:Asherman's syndrome by Dr Humberto Scoccia
- Asherman's syndrome information by Dr Jason Abbott
- On a rare form of Asherman's syndrome by Dr Steven Palter
Template:Diseases of the pelvis, genitals and breasts
de:Synechie hr:Sinehija it:Sindrome di Asherman he:תסמונת אשרמן nl:Syndroom van Asherman