Arrhythmia resident survival guide
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rim Halaby, M.D. [2]
Click on The Type of Arrhythmia You Are Looking For:
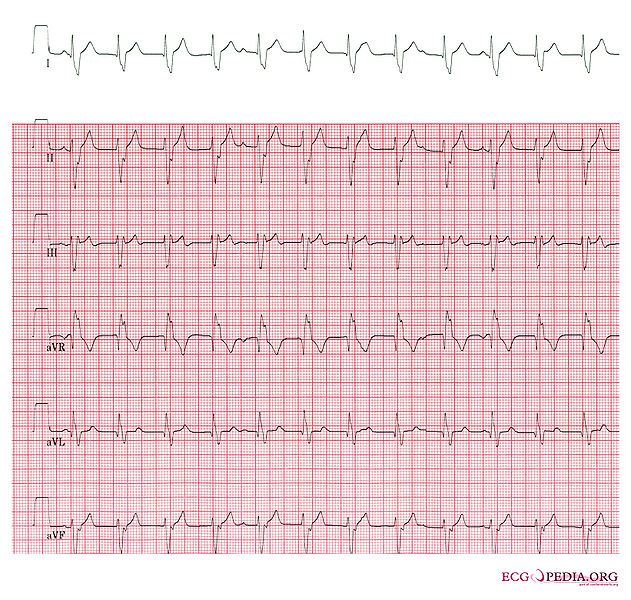
Atrial fibrillation resident survival guide
Atrial fibrillation is characterized by an irregularly irregular rhythm, absent P waves and a ventricular rate of 100-180 beats/minute. Suspect the presence of atrial fibrillation with WPW when ventricular rate exceeds this range.
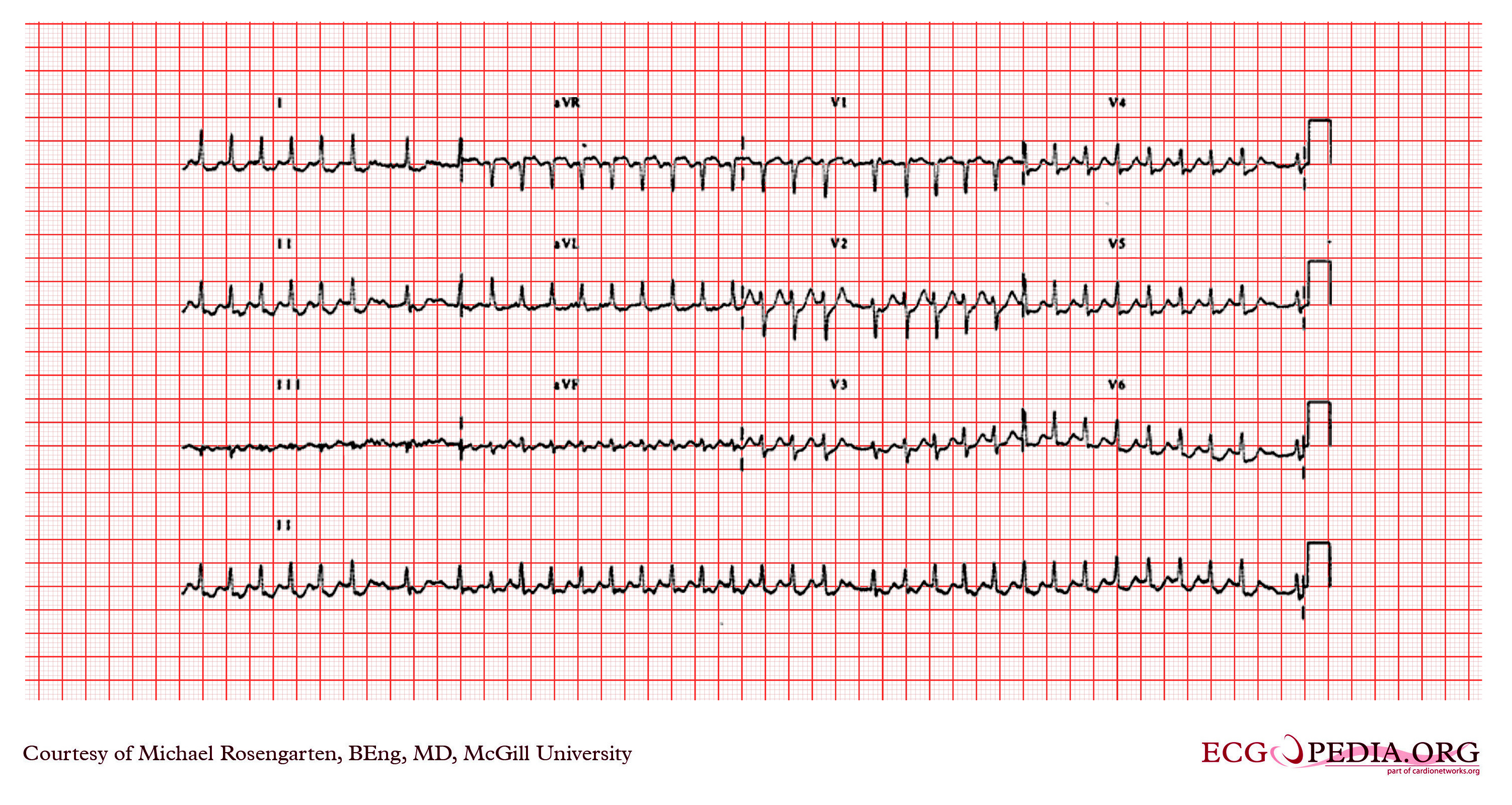
Atrial flutter resident survival guide
Atrial flutter is characterized by a regular rhythm, sawtooth appearance and an average atrial rate of 300 beats per minute. Depending on the nature of the atrioventricular conduction, the average ventricular rate is 300, 150 or 75 beats per minute for 1:1, 2:1 or 4:1 conduction respectively.
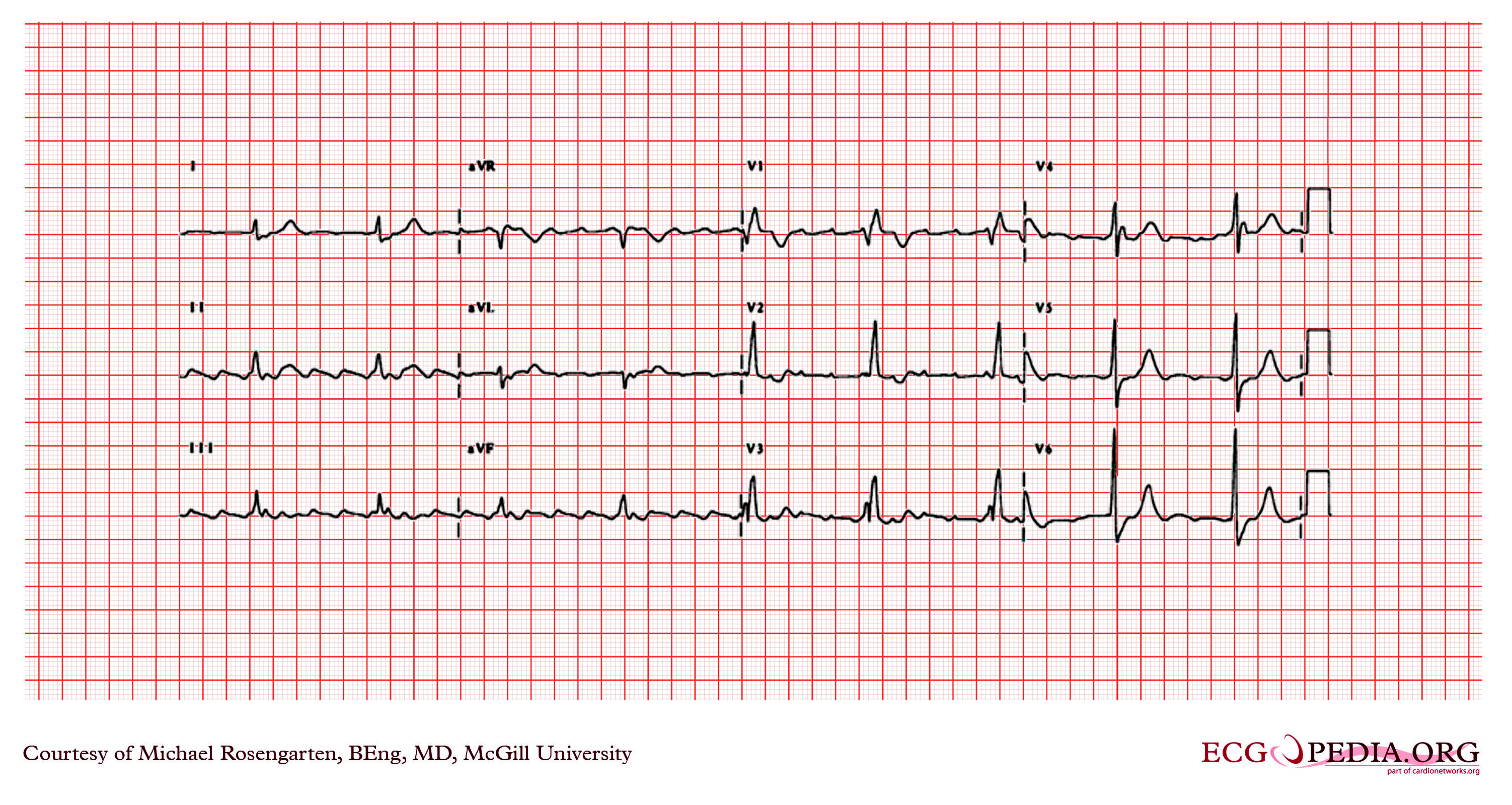
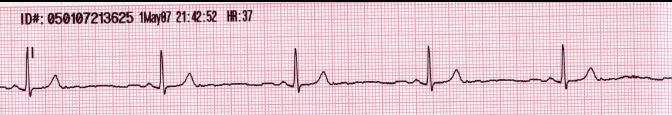
Bradycardia resident survival guide
Bradycardia is characterized by a heart rate lower than 60 beats per minute.
Narrow complex tachycardia resident survival guide
Narrow complex tachycardia is characterized by a heart rate > 100 beats per minute and a QRS complex of a duration < 120 milliseconds.
Wide complex tachycardia resident survival guide
Narrow complex tachycardia is characterized by a heart rate > 100 beats per minute and a QRS complex of a duration > 120 milliseconds.
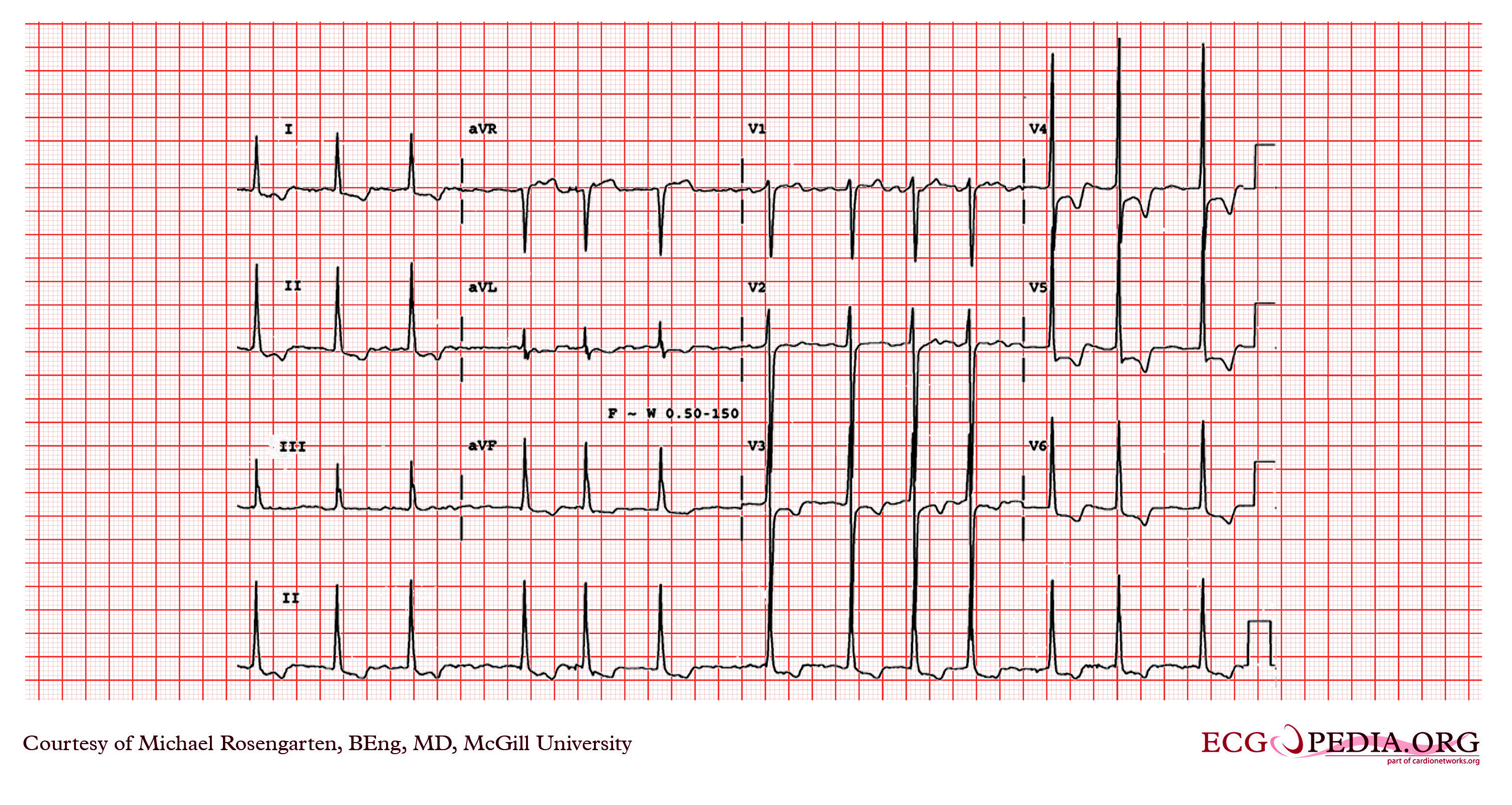
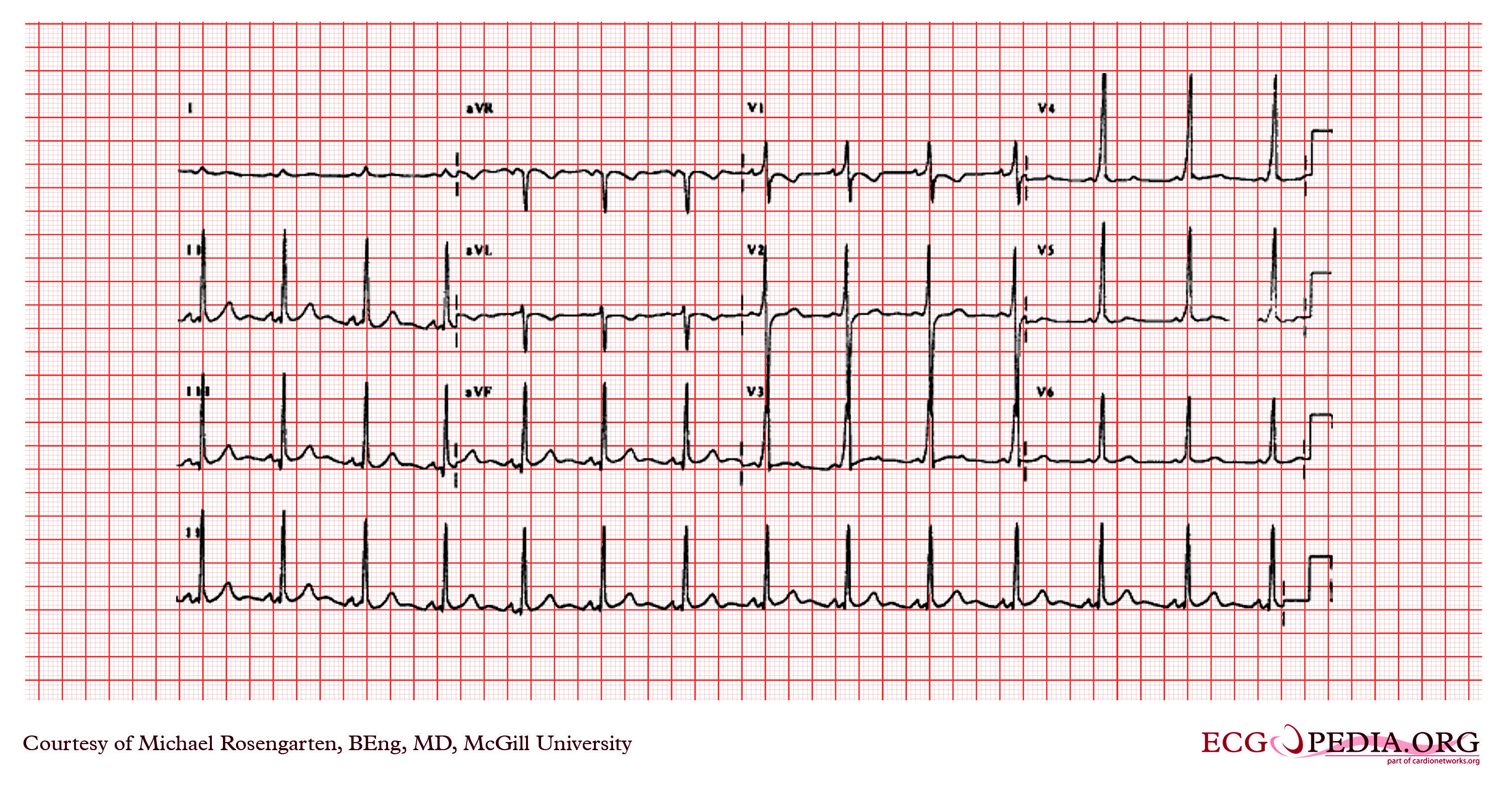
Wolff-Parkinson-White syndrome resident survival guide
While Wolff Parkinson White (WPW) pattern is characterized by a short PR interval and the presence of a delta wave, WPW syndrome is the presence of an arrhythmia, such as AVRT, atrial fibrillation or atrial flutter, in a subject with preexisting WPW pattern. When the arrhythmia occurs, the delta wave commonly disappears. AVRT is orthodromic in most of the cases (regular rhythm, narrow QRS) but can also be antidromic (regular rhythm, wide QRS).