Aortic coarctation: Difference between revisions
(→CT) |
(→CT) |
||
| Line 220: | Line 220: | ||
===CT=== | ===CT=== | ||
<small> CT images shown below are courtesy of Cafer Zorkun and copylefted </small> | |||
<div align="left"> | <div align="left"> | ||
<gallery heights="225" widths="225"> | <gallery heights="225" widths="225"> | ||
Image:Coarctation-of-the-aorta-CT-001.jpg|Aortic Coarctation | Image:Coarctation-of-the-aorta-CT-001.jpg|Aortic Coarctation | ||
Image:Coarctation-of-the-aorta-CT-002.jpg|Aortic Coarctation | Image:Coarctation-of-the-aorta-CT-002.jpg|Aortic Coarctation | ||
</gallery> | </gallery> | ||
</div> | </div> | ||
Revision as of 22:44, 3 March 2011
For patient information click here
| Aortic coarctation | |
 | |
|---|---|
| ICD-10 | Q25.1 |
| ICD-9 | 747.10 |
| OMIM | 120000 |
| DiseasesDB | 2876 |
| eMedicine | med/154 |
| MeSH | D001017 |
| Cardiology Network |
 Discuss Aortic coarctation further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor in Chief: Claudia P. Hochberg M.D. [2]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [3]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [4] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
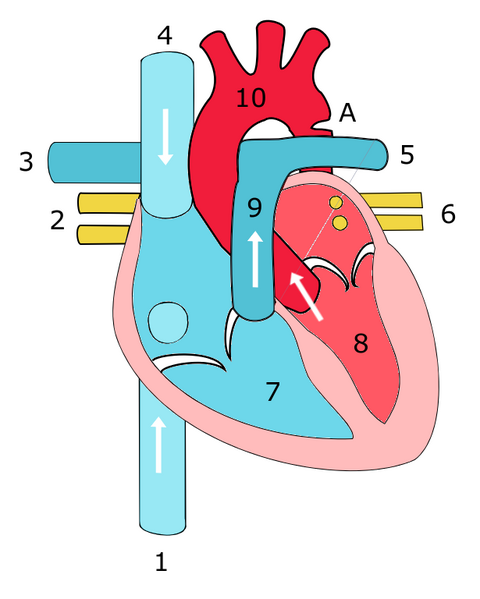
Aortic coarctation is a localized narrowing or abrupt constriction of the aortic arch anywhere along its length. It is most common distal to the origin of the left subclavian artery, near the area where the ductus arteriosus (ligamentum arteriosum after its regression) inserts. Less commonly, the obstruction can occur in the abdominal aorta.
There is a dilation of the aorta immediately above the narrowing, but especially just below. Therefore the latin term "coarctatus", which means contracted or tightened.
History
Johann Friederich Meckel, Prussian anatomist, introduced the description of coarctation of aorta in 1760.
In 1903, Bonnett was the first in classify the aortic coarctation into infantile type (diffuse narrowing of the aorta in the region proximal to the ductus arteriousus) and adult type or more abrupt constriction of the aorta just distal to the origin of the left subclavian artery, close to the ductus insertion.
In 1951, Johnson et al, classified the coarctation based upon the position of the ductus arteriousus and its relation to the coarctation as preductal aortic coarctation and postductal aortic coarctation.
Epidemiology and Demographics
Coarctation occurs in about 7% of patients with congenital heart defects. It is more common in males than females with a ratio of 2:1. Up to 25% of patients with Turner syndrome have coarctation of the aorta.
Classification
There are three types:[1]
- Preductal coarctation: The narrowing is proximal to the ductus arteriosus. If severe, blood flow to the aorta distal (to lower body) to the narrowing is dependent on a patent ductus arteriosus, and hence its closure can be life-threatening. Preductal coarctation results when an intracardiac anomaly during fetal life decreases blood flow through the left side of the heart, leading to hypoplastic development of the aorta.
- Ductal coarctation: The narrowing occurs at the insertion of the ductus arteriosus. This kind usually appears when the ductus arteriosus closes.
- Postductal coarctation: The narrowing is distal to the insertion of the ductus arteriosus. Even with an open ductus arteriosus blood flow to the lower body can be impaired. Newborns with this type of coarctation may be critically sick from the birth. This type is most common in adults. It is associated with notching of the ribs, hypertension in the upper extremities, and weak pulses in the lower extremities. Postductal coarctation is most likely the result of muscular ductal (ductus arteriosis) extends into the aorta during fetal life.
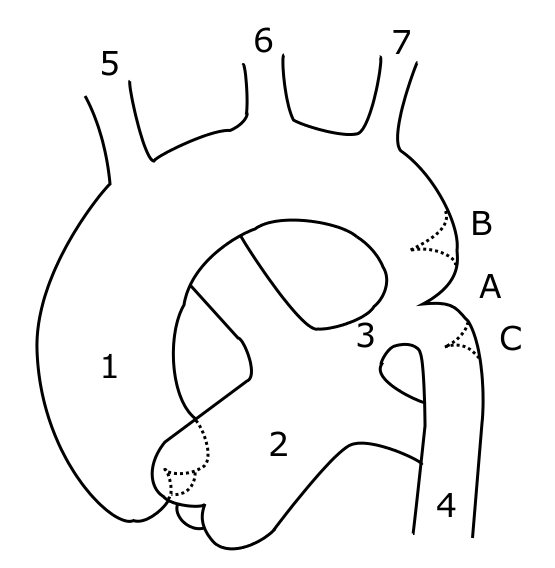
Anatomy
Defect location
- 95% of the lesions are located distal to the left subclavian artery and proximal to the ductus arteriosus (preductal coarctation) or just at or distal to the ductus (postductal coarctation).
- 5% of coarctations are located proximal to the left subclavian artery, or rarely in the abdominal aorta.
- In some cases, coarctation presents as a long segment or a tubular hypoplasia.
The stenosis is caused by an infolding of the left posterolateral aspect of the aortic wall resulting in an eccentric narrowing.
Sites of secondary dilation
- Aorta proximal to the coarct
- Aorta distal to the coarctation
- Left subclavian artery
The narrowing progresses throughout life, and extensive collaterals develop from the subclavian (predominantly) and axillary arteries through:
- Internal mammary artery
- Scapular artery
- Intercostal arteries
- Epigastric arteries
- Anterior spinal arteries
Pathophysiology
Coarctation of the aorta can be either congenital or acquired.
Congenital coarctation results from an infolding of the aortic media that incorportaes ductal tissue, forming a ridge that eccentrically narrows the lumen of the vessel. Subsequent intimal proliferation on the ridge leads to progressive narrowing of the vessel lumen. There is a dilatation before and after the narrowing, giving the aorta an hourglass appearance. The exact etiology of the aortic abnormality remains unclear but likely involves a defect in the vascular wall of the aorta due to reduced antegrade intrauterine blood flow or to constriction of ductal tissue extending into the thoracic aorta.
Acquired coartation can occur in systemic arteritides such as Takayasu arteritis. Additionally it may occur in rare cases of severe atherosclerosis.
Natural History
Infancy: In infants with a preductal coarct, the LV output goes to the upper extremities, and the RV output goes to the lower extremities through the patentductus.
Childhood:
- 80% of cases are diagnosed in childhood.
- The preductal form is usually discovered in early infancy because it is usually severe.
- Childhood coarctation is associated with a ventricular septal defect (VSD), tubular hypoplasia of the aortic arch, transposition of the great vessels, and mitral valve disease.
Adolescence:
- When first recognized in adolescents, ocarctation of the aorta is usually not associated with symptoms.
Adulthood:
- The postductal form is often less severe and discovered in adulthood.
- Infrequently coarctation of the aorta is associated with other congenital abnormalities.
- If the coarctation is left untreated, arterial hypertension may become permanent due to irreversible changes in some organs (such as the kidney).
-
AORTA: Coarctation, Adult: Gross, fixed tissue, an excellent illustration of postductal coarctation
-
AORTA: Coarctation: Gross, hypoplastic aortic arch and infantile coarctation well demonstrated.
Genetics
There are rare instances of autosomal dominant inheritence.
Complications
About 50% of patients with coarctation of the aorta die within the first three decades of life, and more than 75% are dead by age 50 due to:
Rupture of the aorta or aortic dissection
- Most frequently in the third or fourth decade.
- Dissections originate either proximally (secondary to hypertension and local stress)or distally (where the jet erodes the intima).
- Ruptures may bleed into the esophagus, and hematemesis or melena may portend disaster.
Infective endocarditis or endarteritis
- Most frequently in the second to fourth decade of life.
Rupture of the circle of Willis
- Most frequently in the second or third decade of life.
- Secondary to the increased incidence of aneurysms in this population and the presence of proximal hypertension.
Congestive Heart Failure
- Common in infants, often occurs with associated abnormalities such as VSD or mitral valve disease.
- In the adult is secondary to hypertension associated with coronary artery disease or aortic valve disease.
Calcific aortic stenosis
- Result of associated bicuspid aortic valve disease that over time becomes calcified.
Associated Conditions
- Turner's syndrome
- Bicuspid aortic valve is present in 40% to 80% of cases
- Patent ductus arteriosus
- Ventricular septal defect
- Anomalies of the head and neck vessels
- Intracerebral aneurysms
Diagnosis
Symptoms
Patients may complain of a headache most likely due to the presence of hypertension.
Physical Examination
Vital Signs
Blood Pressure
Arterial hypertension in the right arm with normal to low blood pressure in the lower extremities is classic. The blood pressure is higher in the upper extremities than in the lower extremities. The patient may complain of a headache due to hypertension.
Pulses
Femoral pulses are often diminished in strength. Exercise exacerbates this gradient.
If the coarctation is situated before the left subclavian artery, the left pulse will be diminished in strength and asynchronous radial pulses will be detected in the right and left arms. A radial-femoral delay between the right arm and the femoral artery may be apparent, while no such delay may be observed with left arm radial-femoral palpation.
A coarctation occurring after the left subclavian artery will produce synchronous radial pulses, but radial-femoral delay will be present under palpation in either arm.
Neck
There may be "webbing" of the neck in patients with Turner syndrome, 10% of whom have aortic coarctation.
Heart
- A systolic ejection click is present when there is an associated bicuspid aortic valve.
- The S2 is loud secondary to hypertension
- An S4 may be present secondary to LVH
- There are 3 potential sources of a murmur: arterial collaterals, an associated bicuspid aortic valve, and the coarctation itself which can be heard over the spine.
- A prominent P2 may be present if there is associated pulmonary hypertension.
Extremities
Cyanosis of the lower extremities may be present.
Occasionally adults may have narrow hips and thin legs or have an undeveloped left arm (in those patients in which the coarctation compromises the origin of the subclavian artery).
Laboratory Findings
Electrocardiogram
With severe coarctation, left ventricular hypertrophy LVH may be present.
Chest X Ray
Irregularities or notching of the inferior margins of the posterior ribs results from collateral flow through dilated and pulsatile intercostal arteries. These collaterals appear after 6 years of age if the coarctation is significant.
Post-stenotic dilation of the aorta results in a classic 'reverse 3 sign' on x-ray. The characteristic bulging of the sign is caused by dilatation of the aorta due to an indrawing of the aortic wall at the site of cervical rib obstruction, with consequent post-stenotic dilation. This physiology results in the reversed '3' image for which the sign is named.[4][5][6]
Echocardiography
- Useful in determining associated abnormalities.
- Weyman et al were able to visualize this area and make the diagnosis on 2D echo in 16/18 patients.
- Confirmation by cardiac catheterization is unnecessary. Only done when the diagnosis is unclear, which is rare. It is mandatory in the infant to determine preoperative anatomy.
<googlevideo>-1958798054061108175&hl=en</googlevideo>
<googlevideo>-5952201527214554387&hl=en</googlevideo>
Angiography
<youtube v=yvwCL3D8MFM />
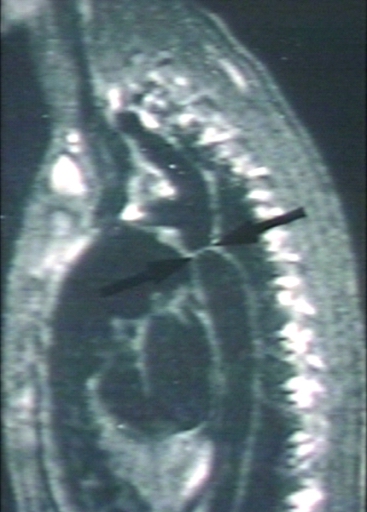
MRI
Magnetic resonance imaging (MRI) can define the location and severity of a coarctation. MRI can also detect associated cardiac abnormalities and is used for serial follow-up after surgical repair or balloon angioplasty. MR angiography has almost completely replaced invasive catheter based techniques for evaluating re coarctation. In adults with untreated coarctation blood often reaches the lower body through collaterals, eg. internal thoracic arteries via. the subclavian arteries. Those can be seen on MR or angiography.
-
[Courtesy of RadsWiki and copylefted]
-
[Courtesy of RadsWiki and copylefted]
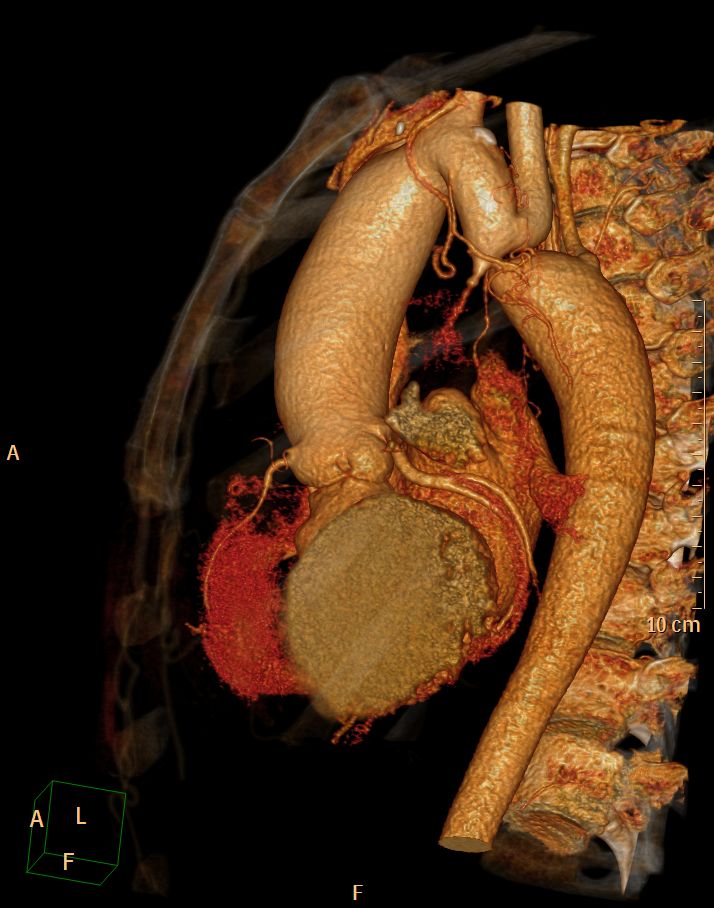
CT
CT images shown below are courtesy of Cafer Zorkun and copylefted
Therapy
Therapy is conservative if the patient is asymptomatic. If symptoms or hypertension are present, treatment for coarctation may be surgical or catheter based. The treatment choice depends on the patients age, the location of the coarctation and other associated anomalies. Recoartctaion after previous surgery is treated percutaneously with either balloon dilation and/or stenting.
References
- ↑ Valdes-Cruz LM, Cayre RO: Echocardiographic diagnosis of congenital heart disease. Philadelphia, 1998.
- ↑ Giuliani et al, Cardiology: Fundamentals and Practice, Second Edition, Mosby Year Book, Boston, 1991, pp. 1670-1676.
- ↑ Deal K, Wooley CF. Coarctation of the Aorta and Pregnancy. Annals of Internal Medicine 1973, 78:706-710.
- ↑ Sabatine, Marc (February 15, 2000). Pocket Medicine. Lippincott Williams & Wilkins. pp. 256 pages. ISBN 0781716497.
- ↑ Blecha, Matthew J. (August 30, 2005). "General Surgery ABSITE and Board Review (Pearls of Wisdom)". McGraw-Hill. ISBN 978-0071464314.
- ↑ Brady Pregerson (October 1, 2006). "Quick Essentials: Emergency Medicine, 2nd Edition". ED Insight Books. ISBN 0976155273.
External links
- A case of coarctation of the aorta was published in the New England Journal of Medicine in 2007 showing chest X-Rays and MRT Images.[1]
- Aortic Coarctation information from Seattle Children's Hospital Heart Center
- Overview and diagram at childrenscentralcal.org
- Diagram at kumc.edu
- Overview and diagram at umich.edu
Template:Link FA de:Aortenisthmusstenose it:Coartazione dell'aorta no:Koarktasjon av aorta nn:Koarktasjon sr:Коарктација аорте uk:Коарктація аорти
- ↑ Quiros-Lopez R, Garcia-Alegria J (2007). "A medical mystery -- high blood pressure". N Engl J Med. 356 (25): 2630. PMID 17582073.


![[Courtesy of RadsWiki and copylefted]](/images/c/c6/Coarctation-of-the-aorta-MRI-002.jpg)