Androgen insensitivity syndrome (patient information)
| Androgen insensitivity syndrome | |
 | |
|---|---|
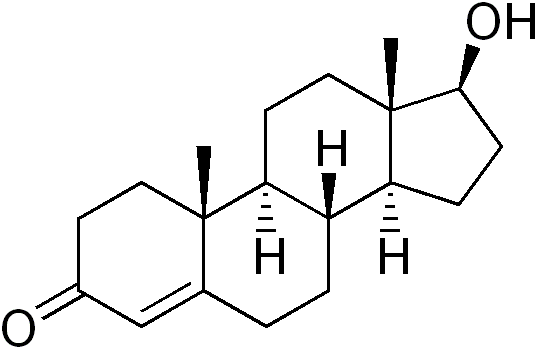
| Testosterone (structure pictured) and dihydrotestosterone to a lesser degree, are the primary androgens involved in AIS. | |
| ICD-10 | E34.5 |
| ICD-9 | 259.5 |
| OMIM | 312300 300068 |
| DiseasesDB | 29662 Template:DiseasesDB2 |
| MeSH | D013734 |
For the WikiDoc page for this topic, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Jinhui Wu, M.D. Aravind Reddy Kothagadi M.B.B.S[2]
Overview
Androgen insensitivity syndrome, also known as testicular feminization, is an x-linked recessive condition resulting in a failure of normal masculinization of the external genitalia. Mutations in the androgen receptor (AR) gene is the cause of this disease. Depending on the amount of residual receptor function, androgen insensitivity syndrome can be divided into two categories: complete androgen insensitivity syndrome and incomplete androgen insensitivity syndrome. The typical characteristic of this disease is feminization. The tests in blood levels of hormones, such as testosterone, dihydrotestosterone (DHT), follicle-stimulating hormone (FSH) and luteinizing hormone (LH) may be helpful for the diagnosis. Treatments may be complex, invloving medical practice and medical ethics. The options are hormone replacement therapy, surgery and psychosocial support. For patients with complete androgen insensitivity syndrome, prognosis is good after orchidectomy at the proper time. Prognosis of incomplete androgen insensitivity syndrome patients depends on the presence and severity of ambiguous genitalia.
What are the symptoms of Androgen insensitivity syndrome?
The typical characteristic of androgen insensitivity syndrome is feminization. It can be divided into two main categories: complete androgen insensitivity syndrome and incomplete androgen insensitivity syndrome. Complete androgen insensitivity syndrome
- At birth, because of external sex characteristics of females, this type of people are usually raised as females and have a female gender identity.
- During puberty, their female secondary sex characteristics, such as breasts develope. At the same time, they have sparse or absent hair in the pubic area and under the arms. They do not menstruate and testes are undescended.
- At adult, they are unable to conceive a child for without uterus. Undescended testes can become cancerous later in life if they are not surgically removed.
Incomplete androgen insensitivity syndrome
- At birth, they may have normal female sex characteristics, both male and female sex characteristics, or normal male sex characteristics. They may be raised as males or as females, and may have a male or a female gender identity.
- During puberty, people with mild androgen insensitivity tend to experience female secondary sex characteristics, such as breast enlargement. Many of them have partial closing of the outer vaginal lips, an enlarged clitoris, and a short vagina but no cervix or uterus. Their testes locate in the abdomen or other unusual places in the body.
- In adult, they are often infertile.
What Causes (disease name)?
- Mutations in the androgen receptor (AR) gene have been shown to cause androgen insensitivity syndrome (AIS), which is characterized by complete or partial resistance to the biological effects of androgens in 46,XY karyotype individuals with normal testis determination and production of age-appropriate androgen concentrations.
- AIS may be classified into mild (MAIS), partial (PAIS) or complete androgen insensitivity (CAIS), based on its phenotypic expression, which ranges from a male phenotype with isolated infertility, to ambiguous genitalia, to a completely female external phenotype.
Who is at highest risk?
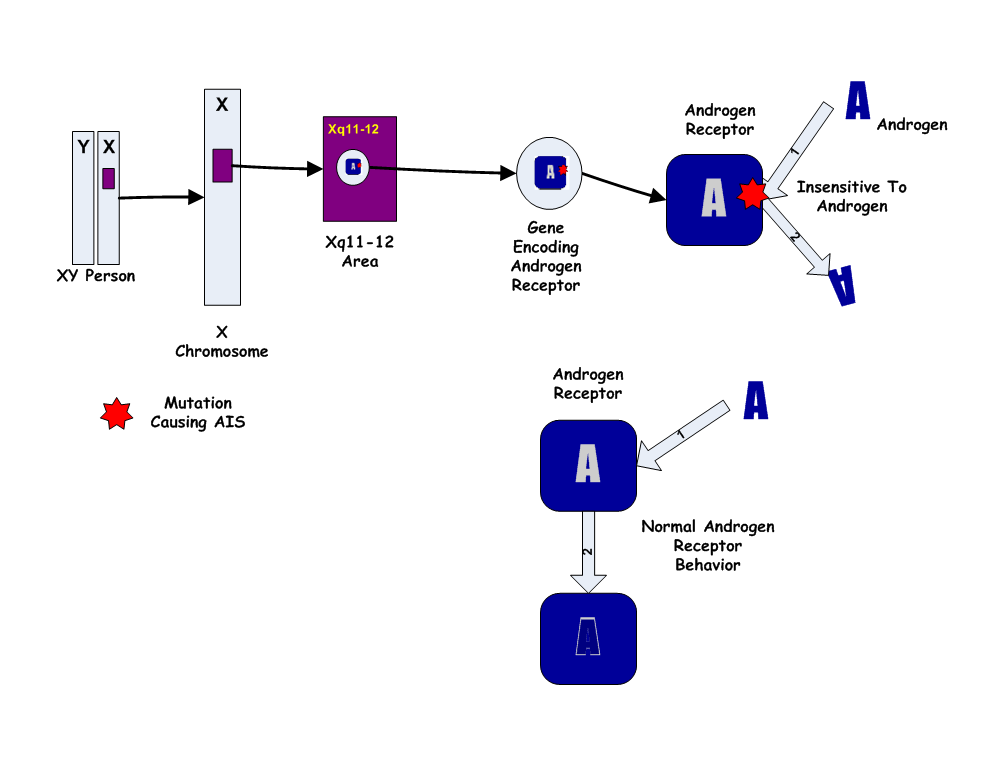
Mutations in the androgen receptor (AR) gene is the cause of androgen insensitivity syndrome. This gene controls the making of a protein called androgen receptor. The mutative gene prevents androgen receptors from working properly. Thus, it makes cells less sensitive response to androgens or prevents cells from using these hormones at all. At last, it makes the body unable to respond to the hormones responsible for the male appearance.
Diagnosis
- Blood levels of hormones: In patients with androgen insensitivity syndrome, normal or high normal blood level of testosterone, dihydrotestosterone (DHT), follicle-stimulating hormone (FSH) may be detected. The level of luteinizing hormone (LH) may be mild higher than normal people. These are important different characteristics between androgen insensitivity syndrome and androgen deficiency.
- Pelvic ultrasound: This is an painless test which uses sound waves to create a picture of the internal organs inside the body. When detecting pelvic ultrasound on the patients with androgen insensitivity syndrome, the doctor may find a vagina but no cervix or uterus, testes in the abdomen.
- Genetic testing: Genetic detect can be done in a gene lab and the patient's blood is analysed by some molecular biology techniques. Researchers may find (AR) gene mutations in the patients with androgen insensitivity syndrome.
When to seek urgent medical care?
Call your health care provider if you or your child appears to have signs or symptoms of the syndrome.
Treatment options
Patients with androgen insensitivity syndrome may be very complex. Medical practice and court decisions appear to be moving in this direction as the new standard of care. The options are hormone replacement therapy, surgery and psychosocial support. Talk to you or your kid's doctor about treatment options and your family's preferences on treatment decisions.
- Hormone replacement therapy: Treatment protocol varies depending on the nature of the gene defect. For patients with complete androgen insensitivity syndrome, estrogen replacement is prescribed after puberty. However for patients with partial androgen insensitivity syndrome who have a male gender identity, testosterone and/or dihydrotestosterone (DHT) may be needed.
- Surgery: For individuals with androgen insensitivity syndrome, orchidectomy may be a standard surgery to prevent possible malignant degeneration of the testes. Many surgeons suggest to execute the surgery during the late teenage years or early 20s. For female gender patients with incomplete androgen insensitivity syndrome, parents and medical ethicists advocate to delay the reconstructive surgery until children are old enough to decide for themselves.
- Psychosocial support: Appropriate psychosocial support for the patient and family is very important. Parents need genetic counseling to know the nature of the condition and the risk of recurrence. Furthermore, they need to establish a long-term relationship with the doctors to discuss new problems when the child grows. The doctors of psychosociology can supply accurate and complete information about the disease, provide emotional support of the family, facilitate communication between the family and medical team.
Diseases with similar symptoms
Where to find medical care for Androgen insensitivity syndrome?
Directions to Hospitals Treating androgen insensitivity syndrome
Prevention of Androgen insensitivity syndrome
The main point of prevention revolves around the women who may carry the gene, providing appropriate information about the condition and the risk of having an affected child, giving her the right to decide on whether to have children.
What to expect (Outlook/Prognosis)?
For patients with complete androgen insensitivity syndrome, prognosis is good after orchidectomy at the proper time. For incomplete androgen insensitivity syndrome patients, it depends on the presence and severity of ambiguous genitalia.
Sources
http://www.geneclinics.org/profiles/androgen/details.html http://www.nlm.nih.gov/medlineplus/ency/article/001180.htm http://ghr.nlm.nih.gov/condition=androgeninsensitivitysyndrome Template:WH Template:WS