Amoebiasis: Difference between revisions
No edit summary |
(No difference)
|
Revision as of 17:19, 28 April 2010
| Amoebiasis | |
| ICD-10 | A06 |
|---|---|
| ICD-9 | 006 |
| MeSH | D000562 |
|
WikiDoc Resources for Amoebiasis |
|
Articles |
|---|
|
Most recent articles on Amoebiasis |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Amoebiasis at Clinical Trials.gov Clinical Trials on Amoebiasis at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Amoebiasis
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Amoebiasis Discussion groups on Amoebiasis Patient Handouts on Amoebiasis Directions to Hospitals Treating Amoebiasis Risk calculators and risk factors for Amoebiasis
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Amoebiasis |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Amoebiasis is a parasitic infection caused by Entamoeba histolytica. It is usually contracted by ingesting water or food contaminated with amoebic cysts. Amoebiasis is an intestinal infection that may or may not be symptomatic. When symptoms are present it is generally known as invasive amoebiasis.
Transmission
Amoebiasis is usually transmitted by , but it can also be transmitted indirectly through contact with dirty hands or objects as well as by oral-anal contact.
Amoebiasis is usually transmitted by the fecal-oral route (contamination of drinking water and foods with fecal matter), but it can also be transmitted indirectly through contact with dirty hands or objects as well as by anal-oral contact.
Infection is spread through ingestion of the cyst form of the parasite, a semi-dormant and hardy structure found in feces. Free-living amoebae, or trophozoites, that do not form cysts but die quickly after leaving the body may also be present: these are rarely the source of new infections. Since amoebiasis is transmitted through contaminated food and water, it is often endemic in regions of the world with limited modern sanitation systems, including Mexico, western South America, South Asia, and western and southern Africa.[1]
Amoebic dysentery is often confused with "traveler's diarrhea", or "Montezuma's Revenge" in Mexico, because of the prevalence of both in developing nations. In fact, most traveler's diarrhea is bacterial or viral in origin.
Liver abscesses can occur without previous development of amoebic dysentery.
Prevention
To help prevent the spread of amoebiasis around the home:
- Wash hands thoroughly with soap and hot running water for at least 10 seconds after using the toilet or changing a baby's diaper, and before handling food
- Clean bathrooms and toilets often. Pay particular attention to toilet seats and taps.
- Avoid sharing towels or face washers.
To help prevent infection:
- Avoid raw vegetables when in endemic areas as they may have been fertilized using human feces.
- Boil water or treat with iodine tablets
Nature of the disease
Most infected people, perhaps 90%, are asymptomatic but this disease has the potential to make the sufferer dangerously ill and it is estimated by the WHO that about 70,000 people die annually worldwide.
Infections can sometimes last for years. Symptoms take from a few days to a few weeks to develop and manifest themselves, but usually it is about two to four weeks. Symptoms can range from mild diarrhoea to dysentery with blood and mucus. The blood comes from amoebae invading the lining of the intestine. In about 10% of invasive cases the amoebae enter the bloodstream and may travel to other organs in the body. Most commonly this means the liver, as this is where blood from the intestine reaches first, but they can end up almost anywhere.
Onset time is highly variable and the average asymptomatic infection persists for over a year. It is theorized that the absence of symptoms or their intensity may vary with such factors as strain of amoeba, immune response of the host, and perhaps associated bacteria and viruses.
In asymptomatic infections the amoeba lives by eating and digesting bacteria and food particles in the gut. It does not usually come in contact with the intestine itself due to the protective layer of mucus that lines the gut. Disease occurs when amoeba comes in contact with the cells lining the intestine. It then secretes the same substances it uses to digest bacteria, which include enzymes that destroy cell membranes and proteins. This process leads to penetration and digestion of human tissues, resulting first in flask-shaped ulcers in the intestine. Entamoeba histolytica ingests the destroyed cells by phagocytosis and is often seen with red blood cells inside. Especially in Latin America, a granulomatous mass (known as an amoeboma) may form in the wall of the colon due to long-lasting cellular response, and is sometimes confused with cancer.
Theoretically, the ingestion of one viable cyst can cause an infection.
Diagnosis of human illness
Asymptomatic human infections are usually diagnosed by finding cysts shed with the stool. Various flotation or sedimentation procedures have been developed to recover the cysts from fecal matter and stains help to visualize the isolated cysts for microscopic examination. Since cysts are not shed constantly, a minimum of 3 stools should be examined. In symptomatic infections, the motile form (the trophozoite) can often be seen in fresh feces. Serological tests exist and most individuals (whether with symptoms or not) will test positive for the presence of antibodies. The levels of antibody are much higher in individuals with liver abscesses. Serology only becomes positive about two weeks after infection. More recent developments include a kit that detects the presence of ameba proteins in the feces and another that detects ameba DNA in feces. These tests are not in widespread use due to their expense.
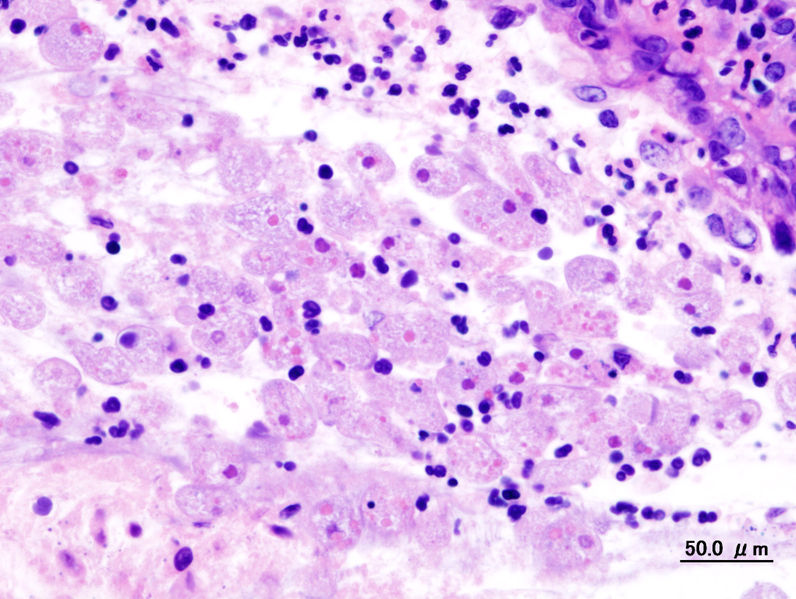
Microscopy is still by far the most widespread method of diagnosis around the world. However it is not as sensitive or accurate in diagnosis as the other tests available. It is important to distinguish the E. histolytica cyst from the cysts of nonpathogenic intestinal protozoa such as Entamoeba coli by its appearance. E. histolytica cysts have a maximum of four nuclei, while the commensal Entamoeba coli has up to 8 nuclei. Additionally, in E. histolytica, the endosome is centrally located in the nucleus, while it is off-center in Entamoeba coli. Finally, chromatoidal bodies in E. histolytica are rounded, while they are jagged in Entamoeba coli. However, other species, Entamoeba dispar and E. moshkovskii, are also a commensal and cannot be distinguished from E. histolytica under the microscope. As E. dispar is much more common than E. histolytica in most parts of the world this means that there is a lot of incorrect diagnosis of E. histolytica infection taking place. The WHO recommends that infections diagnosed by microscopy alone should not be treated if they are asymptomatic and there is no other reason to suspect that the infection is actually E. histolytica.
Relative frequency of the disease
In older textbooks it is often stated that 10% of the world's population is infected with Entamoeba histolytica. It is now known that at least 90% of these infections are due to E. dispar. Nevertheless, this means that there are up to 50 million true E. histolytica infections and approximately seventy thousand die each year, mostly from liver abscesses or other complications. Although usually considered a tropical parasite, the first case reported (in 1875) was actually in St Petersburg in Russia, near the Arctic Circle. Infection is more common in warmer areas, but this is both because of poorer hygiene and because the parasite cysts survive longer in warm moist conditions.
Treatment
E. histolytica infections occur in both the intestine and (in people with symptoms) in tissue of the intestine and/or liver. As a result two different sorts of drugs are needed to rid the body of the infection, one for each location. Metronidazole, or a related drug such a tinidazole, is used to destroy amebae that have invaded tissue. It is rapidly absorbed into the bloodstream and transported to the site of infection. Because it is rapidly absorbed there is almost none remaining in the intestine. Since most of the amebae remain in the intestine when tissue invasion occurs, it is important to get rid of those also or the patient will be at risk of developing another case of invasive disease. Several drugs are available for treating intestinal infections, the most effective of which has been shown to be Paromomycin (also known as Humatin); diloxanide furoate is used in the US. Both types of drug must be used to treat infections, with metronidazole usually being given first, followed by paromomycin or diloxanide. E. dispar does not require treatment, but many laboratories (even in the developed world) do not have the facilities to distinguish this from E. histolytica.
For amebic dysentery a multi-prong approach must be used, starting with one of:
- Metronidazole 500-750mg three times a day for 5-10 days
- Tinidazole 2g once a day for 3 days is an alternative to metronidazole
In addition to the above, one of the following luminal amebicides should be prescribed as an adjunctive treatment, either concurrently or sequentially, to destroy E. histolytica in the colon:
- Paromomycin 500mg three times a day for 10 days
- Diloxanide furoate 500mg three times a day for 10 days
- Iodoquinol 650mg three times a day for 20 days
For amebic liver abscess:
- Metronidazole 400mg three times a day for 10 days
- Tinidazole 2g once a day for 6 days is an alternative to metronidazole
- Diloxanide furoate 500mg three times a day for 10 days must always be given afterwards
Doses for children are calculated by body weight and a pharmacist should be consulted for help.
Herbal treatments
In Mexico, it is common to use herbal tinctures of chaparro amargo (English: castela). 30 drops are taken in a small glass of water first thing in the morning, and 30 drops before the last meal of the day, for seven days straight. After taking a seven day break from the treatment, it is resumed for seven days. Some mild cramping may be felt; it is claimed this means that the amoebas are dying and will be expelled from the body. Many Mexicans use the chaparro amargo treatment regularly, three times a year. The efficacy of such treatments has not been scientifically proven.
A 1998 study in Africa suggests that 2 tablespoons per week of papaya seeds may have some antiamoebic action and aid in prevention of amoebiasis, but this remains unconfirmed. Papaya fruit and seeds are often considered beneficial to digestion in areas where this plant is common.
Complications
In the majority of cases, amoebas remain in the gastrointestinal tract of the hosts. Severe ulceration of the gastrointestinal mucosal surfaces occurs in less than 16% of cases. In fewer cases, the parasite invades the soft tissues, most commonly the liver. Only rarely are masses formed (amoebomas) that lead to intestinal obstruction.
Entamoeba histolytica infection is associated with malnutrition and stunting of growth.[2]
Populations at risk
All people are believed to be susceptible to infection and there is no evidence that individuals with a damaged or undeveloped immunity may suffer more severe forms of the disease.
Food analysis
E. histolytica cysts may be recovered from contaminated food by methods similar to those used for recovering Giardia lamblia cysts from feces. Filtration is probably the most practical method for recovery from drinking water and liquid foods. E. histolytica cysts must be distinguished from cysts of other parasitic (but nonpathogenic) protozoa and from cysts of free-living protozoa as discussed above. Recovery procedures are not very accurate; cysts are easily lost or damaged beyond recognition, which leads to many falsely negative results in recovery tests. (See the FDA Bacteriological Analytical Manual.)
Outbreaks
The most dramatic incident the USA was the Chicago World's Fair outbreak in 1933 caused by contaminated drinking water; defective plumbing permitted sewage to contaminate water. There were 1,000 cases (with 58 deaths). In recent times, food handlers are suspected of causing many scattered infections, but there has been no single outbreak.
Colon: Amebiasis
<youtube v=Xti6OURHxhc/>
References
- ↑
- ↑ Mondal D, Petri Jr WA, Sack RB; et al. (2006). "Entamoeba histolytica-associated diarreal illness is negatively associated with the growth of preschool shildren: evidence from a prospective study". Trans R Soc Trop Med H. 100 (11): 1032&ndash, 38. doi:10.1016/j.trstmh.2005.12.012.