Altered mental status physical examination: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| Line 56: | Line 56: | ||
* HEENT: Sinus tenderness, thyroid, tympanic membrane examination. | * HEENT: Sinus tenderness, thyroid, tympanic membrane examination. | ||
*GIT: Hepatosleenomegaly, signs of liver failure<ref>{{Cite web | last = | first = | title = http://www.bgs.org.uk/Word%20Downloads/delirium.doc | url = http://www.bgs.org.uk/Word%20Downloads/delirium.doc | publisher = | date = | accessdate = }}</ref> | *GIT: Hepatosleenomegaly, signs of liver failure<ref>{{Cite web | last = | first = | title = http://www.bgs.org.uk/Word%20Downloads/delirium.doc | url = http://www.bgs.org.uk/Word%20Downloads/delirium.doc | publisher = | date = | accessdate = }}</ref> | ||
{#ev:youtube|CUaEwgfKOEc}} | |||
{{#ev:youtube|DfJGTXkOtVk}} | |||
==References== | ==References== | ||
Revision as of 02:48, 28 February 2014
|
Altered mental status Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Altered mental status On the Web |
|
American Roentgen Ray Society Images of Altered mental status |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Pratik Bahekar, MBBS [2]
Overview
Physical Examination
Confusion Assessment Method for the ICU (CAM-ICU)
Patient is accessed on following 4 features,
- Onset of symptoms, is acute(change from baseline) or fluctuating as calibrated by Richmond Agitation Sedation Scale or Glasgow Coma Scale.
- Inability to focus as measured by Attention Screening Examination.
- Thinking is not organized
- Altered level of consciousness if Vigilant, Lethargic, Stupor, Coma.
If feature 1 and 2 are present along with 3 or 4 then patient is assessed to have delirium by CAM-ICU scale.[1]
General Examination
- Vitals:
- Blood pressure: Malignant hypertension is an important cause of delirium, and blood pressure must be monitored if the patient is non compliant with antihypertension medications.
- Appearance: Cherry red color indicates CO poisoning, the cynosis may indicate respiratory or cardiac pathology. Jaundice may be indicative of hepatic or biliary pathology.
- Temperature: Fever may be indicative of an underlying infection.
- Pulse: Pulse may give clues to hydration status, cardiac pathology or endocrine disturbances.
- Conscious level: Various levels of arousal can be seen in delirium, ranging from stupor to hperarousal. If the patient appears to have normal arousal level, attention deficit must be accessed which is very commonly seen in delirium.
- Cognitive function using a standardized screening tool, e.g. MoCA, Mental status examination
{{#ev:youtube|3e3oKmtRfgM}}
- Nutritional status: B12 and folate deficiencies can be assessed on physical examination.
- Hydration state: Dehydration as well as an overload of fluids, resulting in hypoxia can cause delirium.
- Infectious foci: Careful examination to rule out conditions such as meningitis, encephalitis, pulmonary consolidation etc.
- Evidence of intoxication or withdrawal for alcohol, and recreational drugs are an important part of delirium work up. Look for tremors, pupil size, needle tracks etc.
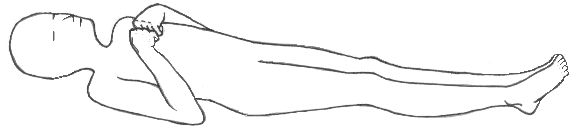
- Posture: Decorticate and Decerebrate rigidity.[2]
{{#ev:youtube|yZUE2Dvf1Q4}}
Decerebrate:
 |
Decorticate:
 |
Systemic Examination
- Neurological examinations: Careful examination must be done to find out neurological causes of delirium, such as cerebrovascular diseases, neurodegenrative disorders such as parkinsonism, alzhimers, and lewi body dementia etc. Many systemic diseases may show neurological manifestations, e.g.hepatic encephalopathy causes flapping tremors. Overdose and intoxication can also effect the central nervous system, e.g. opiates causes pin point pupils, and respiratory depression.[3]
- Cranial nerve examination
- Brainstem reflexes: Cold calorics, doll’s eyes
- Examination of motor system and reflexes.
- Examination of sensory systems.
- Cerebellar function test: Coordination and gait
- signs of meningeal irritation
- Carotid bruits and venous hums
- Cardiopulmonary examination: Pulse, cardiomegaly
- HEENT: Sinus tenderness, thyroid, tympanic membrane examination.
- GIT: Hepatosleenomegaly, signs of liver failure[4]
{#ev:youtube|CUaEwgfKOEc}} {{#ev:youtube|DfJGTXkOtVk}}
References
- ↑ "http://www.icudelirium.org/docs/CAM_ICU_worksheet.pdf" (PDF). External link in
|title=(help) - ↑ "Clinical policy for the initial approach to pa... [Ann Emerg Med. 1999] - PubMed - NCBI".
- ↑ "http://www.bgs.org.uk/Word%20Downloads/delirium.doc". External link in
|title=(help) - ↑ "http://www.bgs.org.uk/Word%20Downloads/delirium.doc". External link in
|title=(help)