Acute myeloid leukemia natural history
|
Acute myeloid leukemia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Acute myeloid leukemia natural history On the Web |
|
American Roentgen Ray Society Images of Acute myeloid leukemia natural history |
|
Risk calculators and risk factors for Acute myeloid leukemia natural history |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Raviteja Guddeti, M.B.B.S. [2] Carlos A Lopez, M.D. [3]
Overview
Common complications of acute myeloid leukemia include infections, disseminated intravascular coagulation, pyoderma gangrenosum, hemorrhage and complications due to side effects of chemotherapy. Prognosis of acute myelogenous leukemia depends on cytogenetics. Cytogenetics that indicate a good prognosis include inversions in chromosome 16 inv(16), translocations between chromosome 8 and 21 t(8;21) and translocations between chromosome 15 and 17 t(15;17).
Complications and Prognosis
Complications
Complications may include:
- Infections
- Disseminated intravascular coagulation
- Pyoderma gangrenosum
- Hemorrhage
- Complications due to side effects of chemotherapy
Prognosis
Acute myeloid leukemia is a curable disease; the chance of cure for a specific patient depends on a number of prognostic factors.[1]
Cytogenetics and prognosis in acute myeloid leukemia
The first publication to address cytogenetics and prognosis was the MRC trial of 1998:[2]
In this table we can see the staging concerning the risk category of acute myeloid leukemia cytogenetics.
| Risk Category | Abnormality | 5-year survival | Relapse rate |
|---|---|---|---|
| Favorable | t(8;21), t(15;17), inv(16) | 70% | 33% |
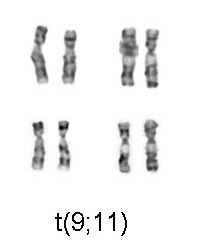
| Intermediate | Normal, +8, +21, +22, del(7q), del(9q), Abnormal 11q23, all other structural or numerical changes | 48% | 50% |
| Adverse | -5, -7, del(5q), Abnormal 3q, Complex cytogenetics | 15% | 78% |
Later, the Southwest Oncology Group and Eastern Cooperative Oncology Group,[6] and later still, Cancer and Leukemia Group B published other, mostly overlapping lists of cytogenetics prognostication in leukemia[7]
Cytogenetics that indicate a good prognosis
- t(8; 21)[8]
- inv(16) or t(16;16)
- t(15;17)
Cytogenetics that indicate poor prognoses
Patients with acute myeloid leukemia that is characterized by deletions of the long arms or monosomies of chromosomes 5 or 7; by translocations or inversions of chromosome 3, t(6; 9), t(9; 22); or by abnormalities of chromosome 11q23.[8]
Note: Normal cytogenetics portends average-risk of acute myeloid leukemia.
Antecedent MDS and prognosis
Acute myeloid leukemia which arises from a pre-existing myelodysplastic syndrome or myeloproliferative disease (so-called secondary AML) has a worse prognosis, as does treatment-related AML arising after chemotherapy for another previous malignancy. Both of these entities are associated with a high rate of unfavorable cytogenetic abnormalities.[9][10][11]
Other prognostic markers
In some studies, age > 60 years and elevated lactate dehydrogenase level were also associated with poorer outcomes.[12] As with most forms of cancer, performance status (i.e. the general physical condition and activity level of the patient) plays a major role in prognosis as well.
- FLT3 internal tandem duplications (ITDs) have been shown to confer a poorer prognosis in acute myeloid leukemia.[13]
- Treating these patients with more aggressive therapy, such as stem-cell transplantation in first remission, has not been shown to enhance long-term survival, so this prognostic feature is of uncertain clinical significance at this point.[14]
- Researchers are investigating the clinical significance of c-KIT mutations[15] in acute myeloid leukemia. These are prevalent, and clinically relevant because of the availability of tyrosine kinase inhibitors, such as sunitinib and imatinib that can block the activity of c-KIT pharmacologically.
- Other genes being investigated as prognostic factors or therapeutic targets include CEBPA, BAALC, ERG, and NPM1.
Overall expectation of cure
- Cure rates in clinical trials have ranged from 20–45%;[16][17] however, it should be noted that clinical trials often include only younger patients and those able to tolerate aggressive therapies. The overall cure rate for all patients with acute myeloid leukemia (including the elderly and those unable to tolerate aggressive therapy) is likely lower. Cure rates for promyelocytic leukemia can be as high as 98%.[18]
Survival
- More than 25% of adults with acute myeloid leukemia (about 45% of those who attain CR) can be expected to survive 3 or more years and may be cured.
- Remission rates in adult acute myeloid leukemia are inversely related to age, with an expected remission rate of more than 65% for those younger than 60 years.
- Data suggest that once attained, duration of remission may be shorter in older patients.
5-Year Survival
- Between 2004 and 2010, the 5-year relative survival of patients with acute myeloid leukemia was 25.4%.[19]
- When stratified by age, the 5-year relative survival of patients with acute myeloid leukemia was 42.8% and 5.6% for patients <65 and ≥ 65 years of age respectively.[19]
References
- ↑ Estey E (2001). "Prognostic factors in acute myelogenous leukemia". Leukemia. 15 (4): 670–2. PMID 11368376.
- ↑ Grimwade D, Walker H, Oliver F, Wheatley K, Harrison C, Harrison G, Rees J, Hann I, Stevens R, Burnett A, Goldstone A. The importance of diagnostic cytogenetics on outcome in AML: analysis of 1,612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children's Leukaemia Working Parties. Blood. 1998 Oct 1;92(7):2322–33.
- ↑ Wheatley K, Burnett A, Goldstone A, Gray R, Hann I, Harrison C, Rees J, Stevens R, Walker H (1999). "A simple, robust, validated and highly predictive index for the determination of risk-directed therapy in acute myeloid leukaemia derived from the MRC AML 10 trial. United Kingdom Medical Research Council's Adult and Childhood Leukaemia Working Parties". Br J Haematol. 107 (1): 69–79. PMID 10520026.
- ↑ Slovak M, Kopecky K, Cassileth P, Harrington D, Theil K, Mohamed A, Paietta E, Willman C, Head D, Rowe J, Forman S, Appelbaum F (2000). "Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study". Blood. 96 (13): 4075–83. PMID 11110676.
- ↑ Byrd J, Mrózek K, Dodge R, Carroll A, Edwards C, Arthur D, Pettenati M, Patil S, Rao K, Watson M, Koduru P, Moore J, Stone R, Mayer R, Feldman E, Davey F, Schiffer C, Larson R, Bloomfield C (2002). "Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B (CALGB 8461)". Blood. 100 (13): 4325–36. PMID 12393746.
- ↑ Slovak ML; Kopecky KJ; Cassileth PA; Harrington DH; Theil KS; Mohamed A; Paietta E; Willman CL; Head DR; Rowe JM; Forman SJ; Appelbaum FR Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood 2000 Dec 15;96(13):4075–83.
- ↑ Byrd J, Mrózek K, Dodge R, Carroll A, Edwards C, Arthur D, Pettenati M, Patil S, Rao K, Watson M, Koduru P, Moore J, Stone R, Mayer R, Feldman E, Davey F, Schiffer C, Larson R, Bloomfield C (2002). "Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B (CALGB 8461)". Blood. 100 (13): 4325–36. PMID 12393746.
- ↑ 8.0 8.1 "National Cancer Institute".
- ↑ Thirman M, Larson R (1996). "Therapy-related myeloid leukemia". Hematol Oncol Clin North Am. 10 (2): 293–320. PMID 8707757.
- ↑ Rowley J, Golomb H, Vardiman J (1981). "Nonrandom chromosome abnormalities in acute leukemia and dysmyelopoietic syndromes in patients with previously treated malignant disease". Blood. 58 (4): 759–67. PMID 7272506.
- ↑ Pedersen-Bjergaard J, Andersen M, Christiansen D, Nerlov C (2002). "Genetic pathways in therapy-related myelodysplasia and acute myeloid leukemia". Blood. 99 (6): 1909–12. PMID 11877259.
- ↑ Haferlach T, Schoch C, Löffler H, Gassmann W, Kern W, Schnittger S, Fonatsch C, Ludwig W, Wuchter C, Schlegelberger B, Staib P, Reichle A, Kubica U, Eimermacher H, Balleisen L, Grüneisen A, Haase D, Aul C, Karow J, Lengfelder E, Wörmann B, Heinecke A, Sauerland M, Büchner T, Hiddemann W (2003). "Morphologic dysplasia in de novo acute myeloid leukemia (AML) is related to unfavorable cytogenetics but has no independent prognostic relevance under the conditions of intensive induction therapy: results of a multiparameter analysis from the German AML Cooperative Group studies". J Clin Oncol. 21 (2): 256–65. PMID 12525517.
- ↑ Schnittger S, Schoch C, Dugas M, Kern W, Staib P, Wuchter C, Löffler H, Sauerland C, Serve H, Büchner T, Haferlach T, Hiddemann W (2002). "Analysis of FLT3 length mutations in 1003 patients with acute myeloid leukemia: correlation to cytogenetics, FAB subtype, and prognosis in the AMLCG study and usefulness as a marker for the detection of minimal residual disease". Blood. 100 (1): 59–66. PMID 12070009.
- ↑ Gale R, Hills R, Kottaridis P, Srirangan S, Wheatley K, Burnett A, Linch D (2005). "No evidence that FLT3 status should be considered as an indicator for transplantation in acute myeloid leukemia (AML): an analysis of 1135 patients, excluding acute promyelocytic leukemia, from the UK MRC AML10 and 12 trials". Blood. 106 (10): 3658–65. PMID 16076872.
- ↑ Paschka P, Marcucci G, Ruppert A, Mrózek K, Chen H, Kittles R, Vukosavljevic T, Perrotti D, Vardiman J, Carroll A, Kolitz J, Larson R, Bloomfield C (2006). "Adverse prognostic significance of KIT mutations in adult acute myeloid leukemia with inv(16) and t(8;21): a Cancer and Leukemia Group B Study". J Clin Oncol. 24 (24): 3904–11. PMID 16921041.
- ↑ Cassileth P, Harrington D, Appelbaum F, Lazarus H, Rowe J, Paietta E, Willman C, Hurd D, Bennett J, Blume K, Head D, Wiernik P (1998). "Chemotherapy compared with autologous or allogeneic bone marrow transplantation in the management of acute myeloid leukemia in first remission". N Engl J Med. 339 (23): 1649–56. PMID 9834301.
- ↑ Matthews J, Bishop J, Young G, Juneja S, Lowenthal R, Garson O, Cobcroft R, Dodds A, Enno A, Gillett E, Hermann R, Joshua D, Ma D, Szer J, Taylor K, Wolf M, Bradstock K (2001). "Patterns of failure with increasing intensification of induction chemotherapy for acute myeloid leukaemia". Br J Haematol. 113 (3): 727–36. PMID 11380464.
- ↑ Sanz M, Lo Coco F, Martín G, Avvisati G, Rayón C, Barbui T, Díaz-Mediavilla J, Fioritoni G, González J, Liso V, Esteve J, Ferrara F, Bolufer P, Bernasconi C, Gonzalez M, Rodeghiero F, Colomer D, Petti M, Ribera J, Mandelli F (2000). "Definition of relapse risk and role of nonanthracycline drugs for consolidation in patients with acute promyelocytic leukemia: a joint study of the PETHEMA and GIMEMA cooperative groups". Blood. 96 (4): 1247–53. PMID 10942364.
- ↑ 19.0 19.1 Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.