Acute myeloid leukemia laboratory tests: Difference between revisions
(Category) |
Shyam Patel (talk | contribs) No edit summary |
||
| Line 2: | Line 2: | ||
{{Acute myeloid leukemia}} | {{Acute myeloid leukemia}} | ||
{{CMG}}; {{AE}} {{RT}} {{CLG}} | {{CMG}}; {{AE}} {{RT}} {{CLG}} {{shyam}} | ||
==Overview== | ==Overview== | ||
The laboratory abnormalities in acute myeloid leukemia can be broadly divided into abnormalities of the complete blood count and abnormalities of the coagulation system. The complete blood count usually shows anemia, thrombocytopenia, leukopenia, and elevated blast count. In the acute promyelocytic leukemia subcategory of acute myeloid leukemia, the coagulation profile usually shows elevated prothrombin time, elevated partial thromboplastin time, elevated thrombin time, elevated reptilase time, and low fibrinogen. This combination of coagulation parameters accounts for high hemorrhagic risk especially in patients with acute promyelocytic leukemia. | |||
==Laboratory Findings== | ==Laboratory Findings== | ||
* | ===Abnormalities of the complete blood count=== | ||
* | *'''[[Anemia]]''': Anemia refers to decreased red blood cell production, which results in low hemoglobin content in the peripheral blood. Hemoglobin values are typically less than 10 g/dl in most patients with acute myeloid leukemia. The degree of anemia corresponds with the amount of bone marrow infiltration by leukemic cells. Patients with severe or advanced leukemia will usually have severe anemia. Severe anemia can result in profound fatigue, pallor, and shortness of breath. | ||
* | *'''[[Thrombocytopenia]]''': Thrombocytopenia refers to low [[platelet]] count. The platelet count is usually less than 150,000 cells per microliter. Low platelet count in patients with acute myeloid leukemia is typically due to two reasons. Firstly, leukemic cell infiltration in the bone marrow results in disruption of normal [[megakaryocyte]] production with decreased platelet production. Secondly, coagulopathy (disseminated intravascular coagulation) can result in platelet consumption and therefore a low platelet count. This latter reason is unique to the acute promyelocytic leukemia category of acute myeloid leukemia. The degree of thrombocytopenia also confers prognostic value in acute promyelocytic leukemia: platelet counts lower than 40,000 cells per microliter carries a worse prognosis than platelet counts greater than 40,000 cells per microliter. | ||
* | *'''[[Leukopenia]]''': Leukopenia refers to [[white blood cell]] count below 4,000 cells per microliter. Hyperleukocytosis, or excessively elevated [[white blood cell]] count, is common in some types of acute myeloid leukemia. Leukopenia, or low [[white blood cell]] count, is more common in patients with acute promyelocytic leukemia, unlike most other types of leukemia. In some cases, however, patients can have high [[white blood cell]] counts, which confers a worse prognosis. [[White blood cell]] count above 10,000 cells per microliter defines high-risk disease in acute promyelocytic leukemia. | ||
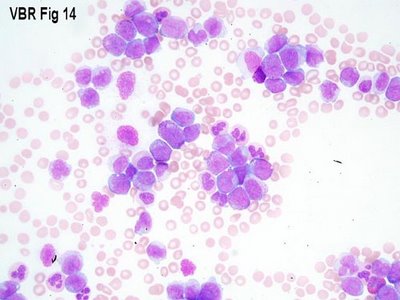
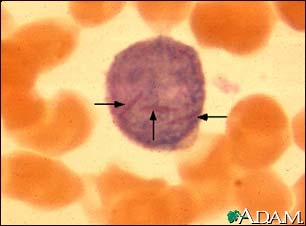
*'''[[Elevated blast count]]''': The [[white blood cell]] differential will typically show the presence of circulating [[blasts]], which are the malignant cells in acute promyelocytic leukemia. Blasts are equivalent to stem cells, and the normal blast count in the bone marrow is less than 5%. An elevated peripheral blood blast count is a common initial finding in the disease, and this finding frequently serves as the trigger for additional workup. The presence of peripheral blood blasts must be evaluated further by performing a bone marrow biopsy. | |||
===Abnormalities of coagulation parameters=== | |||
*'''[[Hypofibrinogenemia]]''': Hypofibrinogenemia, or fibrinogen level below 100 mg/dl, is commonly found in patients with acute promyelocytic leukemia. Hypofibrinogenemia is a key component of disseminated intravascular coagulation, which is characterized by widespread clot formation and breakdown. [[Fibrinogen]], also known as factor I of the coagulation cascade, is broken down in patients with acute promyelocytic leukemia, resulting in bleeding complications. Values of less than 100 mg/dl require treatment with [[cryoprecipitate]], which restores fibrinogen levels towards normal range.<ref name="pmid16504043">{{cite journal| author=Franchini M, Lippi G, Manzato F| title=Recent acquisitions in the pathophysiology, diagnosis and treatment of disseminated intravascular coagulation. | journal=Thromb J | year= 2006 | volume= 4 | issue= | pages= 4 | pmid=16504043 | doi=10.1186/1477-9560-4-4 | pmc=1402263 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16504043 }} </ref> | |||
* | *'''Elevated [[prothrombin time (PT)]]''': High PT values, typically above 15 seconds, are common in patients with acute promyelocytic leukemia. This is due to [[disseminated intravascular coagulation]], which results in consumption of coagulation factors of the intrinsic and extrinsic coagulation pathways. High PT reflects consumption of factors from the extrinsic pathway, such as factor VII.<ref name="pmid16504043">{{cite journal| author=Franchini M, Lippi G, Manzato F| title=Recent acquisitions in the pathophysiology, diagnosis and treatment of disseminated intravascular coagulation. | journal=Thromb J | year= 2006 | volume= 4 | issue= | pages= 4 | pmid=16504043 | doi=10.1186/1477-9560-4-4 | pmc=1402263 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16504043 }} </ref> | ||
*'''Elevated [[partial thromboplastin time (PTT)]]''': High PTT values, typically above 40 second, are common in patients with acute promyelocytic leukemia. This is due to [[disseminated intravascular coagulation]], which results in consumption of coagulation factors of the intrinsic and extrinsic coagulation pathways. High PTT reflects consumption of factors from the intrinsic pathway, such as factors XII, XI, IX, and VIII.<ref name="pmid16504043">{{cite journal| author=Franchini M, Lippi G, Manzato F| title=Recent acquisitions in the pathophysiology, diagnosis and treatment of disseminated intravascular coagulation. | journal=Thromb J | year= 2006 | volume= 4 | issue= | pages= 4 | pmid=16504043 | doi=10.1186/1477-9560-4-4 | pmc=1402263 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16504043 }} </ref> | |||
*'''Elevated [[thrombin time]]''': Thrombin time measures the conversion of [[fibrinogen]] to [[fibrin]], and therefore a high thrombin time is seen in patients with [[coagulopathy]] from acute promyelocytic leukemia. Thrombin is also known as factor II of the coagulation cascade and is immediately upstream of [[fibrinogen]].<ref name="pmid16504043">{{cite journal| author=Franchini M, Lippi G, Manzato F| title=Recent acquisitions in the pathophysiology, diagnosis and treatment of disseminated intravascular coagulation. | journal=Thromb J | year= 2006 | volume= 4 | issue= | pages= 4 | pmid=16504043 | doi=10.1186/1477-9560-4-4 | pmc=1402263 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16504043 }} </ref> | |||
*'''Elevated [[reptilase time]]''': Reptilase time also measures the conversion of [[fibrinogen]] to [[fibrin]], but this test uses a different enzyme, known as reptilase, which is derived from snake venom. The unique feature of the reptilase time is that it can be used to differentiate high PTT caused by heparin effect: the reptilase time is not sensitive to heparin. Reptilase time is high in patients with coagulopathy from acute promyelocytic leukemia. | |||
*'''Elevated [[D-dimer]]''': D-dimer measures simulataneous clot formation and breakdown. Elevated D-dimer is not specific to acute promyelocytic leukemia, as it can be found in patients with obstetric complications (eclampsia and amniotic fluid embolism) or sepsis from ''Neisseria meningitides''. Elevated D-dimer is very sensitive for an underlying coagulopathy and is an excellent test for ruling out a hematologic condition is the pre-test probability is low. D-dimer is elevated in the majority of cases of acute promyelocytic leukemia.<ref name="pmid23049403">{{cite journal| author=Bassi SC, Rego EM| title=Molecular basis for the diagnosis and treatment of acute promyelocytic leukemia. | journal=Rev Bras Hematol Hemoter | year= 2012 | volume= 34 | issue= 2 | pages= 134-9 | pmid=23049403 | doi=10.5581/1516-8484.20120033 | pmc=3459394 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23049403 }} </ref> | |||
* | |||
* | |||
{| align="center" | {| align="center" | ||
Revision as of 23:26, 28 October 2018
|
Acute myeloid leukemia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Acute myeloid leukemia laboratory tests On the Web |
|
American Roentgen Ray Society Images of Acute myeloid leukemia laboratory tests |
|
Risk calculators and risk factors for Acute myeloid leukemia laboratory tests |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Raviteja Guddeti, M.B.B.S. [2] Carlos A Lopez, M.D. [3] Shyam Patel [4]
Overview
The laboratory abnormalities in acute myeloid leukemia can be broadly divided into abnormalities of the complete blood count and abnormalities of the coagulation system. The complete blood count usually shows anemia, thrombocytopenia, leukopenia, and elevated blast count. In the acute promyelocytic leukemia subcategory of acute myeloid leukemia, the coagulation profile usually shows elevated prothrombin time, elevated partial thromboplastin time, elevated thrombin time, elevated reptilase time, and low fibrinogen. This combination of coagulation parameters accounts for high hemorrhagic risk especially in patients with acute promyelocytic leukemia.
Laboratory Findings
Abnormalities of the complete blood count
- Anemia: Anemia refers to decreased red blood cell production, which results in low hemoglobin content in the peripheral blood. Hemoglobin values are typically less than 10 g/dl in most patients with acute myeloid leukemia. The degree of anemia corresponds with the amount of bone marrow infiltration by leukemic cells. Patients with severe or advanced leukemia will usually have severe anemia. Severe anemia can result in profound fatigue, pallor, and shortness of breath.
- Thrombocytopenia: Thrombocytopenia refers to low platelet count. The platelet count is usually less than 150,000 cells per microliter. Low platelet count in patients with acute myeloid leukemia is typically due to two reasons. Firstly, leukemic cell infiltration in the bone marrow results in disruption of normal megakaryocyte production with decreased platelet production. Secondly, coagulopathy (disseminated intravascular coagulation) can result in platelet consumption and therefore a low platelet count. This latter reason is unique to the acute promyelocytic leukemia category of acute myeloid leukemia. The degree of thrombocytopenia also confers prognostic value in acute promyelocytic leukemia: platelet counts lower than 40,000 cells per microliter carries a worse prognosis than platelet counts greater than 40,000 cells per microliter.
- Leukopenia: Leukopenia refers to white blood cell count below 4,000 cells per microliter. Hyperleukocytosis, or excessively elevated white blood cell count, is common in some types of acute myeloid leukemia. Leukopenia, or low white blood cell count, is more common in patients with acute promyelocytic leukemia, unlike most other types of leukemia. In some cases, however, patients can have high white blood cell counts, which confers a worse prognosis. White blood cell count above 10,000 cells per microliter defines high-risk disease in acute promyelocytic leukemia.
- Elevated blast count: The white blood cell differential will typically show the presence of circulating blasts, which are the malignant cells in acute promyelocytic leukemia. Blasts are equivalent to stem cells, and the normal blast count in the bone marrow is less than 5%. An elevated peripheral blood blast count is a common initial finding in the disease, and this finding frequently serves as the trigger for additional workup. The presence of peripheral blood blasts must be evaluated further by performing a bone marrow biopsy.
Abnormalities of coagulation parameters
- Hypofibrinogenemia: Hypofibrinogenemia, or fibrinogen level below 100 mg/dl, is commonly found in patients with acute promyelocytic leukemia. Hypofibrinogenemia is a key component of disseminated intravascular coagulation, which is characterized by widespread clot formation and breakdown. Fibrinogen, also known as factor I of the coagulation cascade, is broken down in patients with acute promyelocytic leukemia, resulting in bleeding complications. Values of less than 100 mg/dl require treatment with cryoprecipitate, which restores fibrinogen levels towards normal range.[1]
- Elevated prothrombin time (PT): High PT values, typically above 15 seconds, are common in patients with acute promyelocytic leukemia. This is due to disseminated intravascular coagulation, which results in consumption of coagulation factors of the intrinsic and extrinsic coagulation pathways. High PT reflects consumption of factors from the extrinsic pathway, such as factor VII.[1]
- Elevated partial thromboplastin time (PTT): High PTT values, typically above 40 second, are common in patients with acute promyelocytic leukemia. This is due to disseminated intravascular coagulation, which results in consumption of coagulation factors of the intrinsic and extrinsic coagulation pathways. High PTT reflects consumption of factors from the intrinsic pathway, such as factors XII, XI, IX, and VIII.[1]
- Elevated thrombin time: Thrombin time measures the conversion of fibrinogen to fibrin, and therefore a high thrombin time is seen in patients with coagulopathy from acute promyelocytic leukemia. Thrombin is also known as factor II of the coagulation cascade and is immediately upstream of fibrinogen.[1]
- Elevated reptilase time: Reptilase time also measures the conversion of fibrinogen to fibrin, but this test uses a different enzyme, known as reptilase, which is derived from snake venom. The unique feature of the reptilase time is that it can be used to differentiate high PTT caused by heparin effect: the reptilase time is not sensitive to heparin. Reptilase time is high in patients with coagulopathy from acute promyelocytic leukemia.
- Elevated D-dimer: D-dimer measures simulataneous clot formation and breakdown. Elevated D-dimer is not specific to acute promyelocytic leukemia, as it can be found in patients with obstetric complications (eclampsia and amniotic fluid embolism) or sepsis from Neisseria meningitides. Elevated D-dimer is very sensitive for an underlying coagulopathy and is an excellent test for ruling out a hematologic condition is the pre-test probability is low. D-dimer is elevated in the majority of cases of acute promyelocytic leukemia.[2]
 |
 |
References
- ↑ 1.0 1.1 1.2 1.3 Franchini M, Lippi G, Manzato F (2006). "Recent acquisitions in the pathophysiology, diagnosis and treatment of disseminated intravascular coagulation". Thromb J. 4: 4. doi:10.1186/1477-9560-4-4. PMC 1402263. PMID 16504043.
- ↑ Bassi SC, Rego EM (2012). "Molecular basis for the diagnosis and treatment of acute promyelocytic leukemia". Rev Bras Hematol Hemoter. 34 (2): 134–9. doi:10.5581/1516-8484.20120033. PMC 3459394. PMID 23049403.