Acute kidney injury
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: Acute kidney failure; acute renal failure; acute uremia; AKI; ARF
Overview
Acute kidney injury (AKI), formerly known as acute renal failure, is characterized by an abrupt loss of kidney function resulting in a failure to excrete nitrogenous waste products (among others), and a disruption of fluid and electrolyte homeostasis. AKI defines a spectrum of disease with common clinical features including an increase in the serum creatinine and BUN levels, often associated with a reduction in urine volume. AKI can be caused by a multitude of factors broadly categorized into pre-renal (usually ischemic), intrinsic renal (usually toxic), and post-renal (usually obstructive) injuries. Generally, treatment is supportive until renal function is restored especially in light of the fluid overload, electrolyte imbalances, and uremic toxin accumulation. Still, renal replacement modalities are sometimes indicated.
Definition
Over 30 different definitions of AKI have been used in the literature since it was first described, which prompted the need for a uniform definition. In 2002, The Acute Dialysis Quality Initiative (ADQI) proposed the first consensus definition known as the RIFLE criteria. The acronym combines a classification of 3 levels of renal dysfunction (Risk, Injury, Failure) with 2 clinical outcomes (Loss, ESRD). This unified classification was proposed to enable a viable comparison in trials of prevention and therapy and to observe clinical outcomes of the defined stages of AKI.[1]
| Classification | GFR criteria | Urine output criteria |
| Risk | 1.5x increase in SCr or GFR decrease >25% | <0.5 mL/kg/h for 6 hours |
| Injury | 2x increase in SCr or GFR decrease >50% | <0.5 mL/kg/h for 12 hours |
| Failure | 3x increase in SCr or GFR decrease >75% | <0.3 mL/kg/h for 24 hours or anuria for 12 hours |
| Loss | Complete loss of renal function >4 weeks | |
| End-stage Renal Disease | Complete loss of renal function >3 months | |
In 2007, the Acute Kidney Injury Network (AKIN) proposed a modified diagnostic criteria based on the RIFLE criteria. The initiative separated the definition and staging into 2 separate entities previously combined in the RIFLE criteria. This made the definition more clinically applicable. AKI was defined as either one of the following:[2]
|
In March 2012, the Kidney Disease Improving Global Outcomes (KDIGO) Clinical Practice Guidelines for Acute Kidney Injury retained the AKIN definition while implementing modifications to the staging criteria of AKI. [3]
Historical Perspective
It is really unclear when acute kidney injury or acute renal failure came to light as a separate disease entity. The first documented report of abrupt loss of renal function came from Beall et al in 1941 who described a man admitted to St. Thomas's Hospital after a crush injury to the leg in a bombing incident. They describe a course of rapidly progressive renal insufficiency with dark urine, edema, elevated potassium levels, and disorientation. [4]
The earliest definition came from Lucké in 1946 who described the histologic pathology we now know as acute tubular necrosis. The term lower nephron nephrosis was introduced and was later used to refer to abrupt renal failure secondary to excessive vomiting, thermal burns, crush injuries, hemolysis, and obstructive prostate disease.[5][6] The term slowly drifted to become acute renal failure to depict a clinical syndrome rather than a pathologic finding. Acute renal failure was then replaced by acute kidney injury in 2006 following a consensus that even minor changes in serum creatinine not necessarily overt failure can lead to significant changes in outcome.
Staging
Initially, the staging of AKI was a part of the proposed definition by the ADQI initiative and the RIFLE criteria. In 2007, AKIN proposed separated the 2 and created a new staging scheme modified from the RIFLE criteria. Prior to the 2012, RIFLE and AKIN criteria were used interchangeably to stage patients with renal injury.[1][2] Although certain concerns about the differences between the 2 classification schemes, it was shown that the differences do not carry through to mortality and outcome measures.[7]
| Classification | GFR criteria | Urine output criteria |
| Stage 1 | Increase in SCr ≥0.3 mg/dL or 1.5x to 2x increase from baseline | <0.5 mL/kg/h for 6 hours |
| Stage 2 | 2x to 3x increase in SCr from baseline | <0.5 mL/kg/h for 12 hours |
| Stage 3 | >3x increase in SCr or SCr≥ 4.0 mg/dL with acute increase >0.5 md/dL | <0.3 mL/kg/h for 24 hours or anuria for 12 hours |
In 2012, the KDIGO AKI guidelines proposed a combined staging scheme that takes into account both criteria and clinical outcome. [3] The rationale behind AKI staging is the needed to determine overall outcome as higher stags of AKI carry a greater risk of all cause and cardiovascular mortality, renal replacement, as well as chronic kidney disease even after AKI resolution.[8][9][10][11]
| Staging | GFR criteria | Urine output criteria |
| Stage 1 | 1.5 - 1.9 times baseline or ≥ 0.3 mg/dl increase | <0.5 ml/kg/h for 6 - 12 hours |
| Stage 2 | 2.0 - 2.9 times baseline | <0.5 ml/kg/h for ≥ 12 hours |
| Stage 3 | 3.0 times baseline or increase in serum creatinine to 4.0 mg/dL or initiation of renal replacement therapy or decrease in eGFR to <35 ml/min per 1.73 m2 (in patients <18 years) |
<0.3 mL/kg/h for 24 hours or anuria for 12 hours |
The guidelines also advocated that in case of discordance between urine output and serum creatinine patients should be classified to the highest applicable AKI stage. Also, new emphasis on the differences seen in the pediatric population gave rise to revised definition of Stage 3 AKI in patients less than 18 years of age.[3]
Pathophysiology & Etiologies
Etiologies of AKI can be divided based on pathophysiologic mechanisms into 3 broad categories: prerenal, intrinsic renal, and postrenal causes.

Prerenal AKI
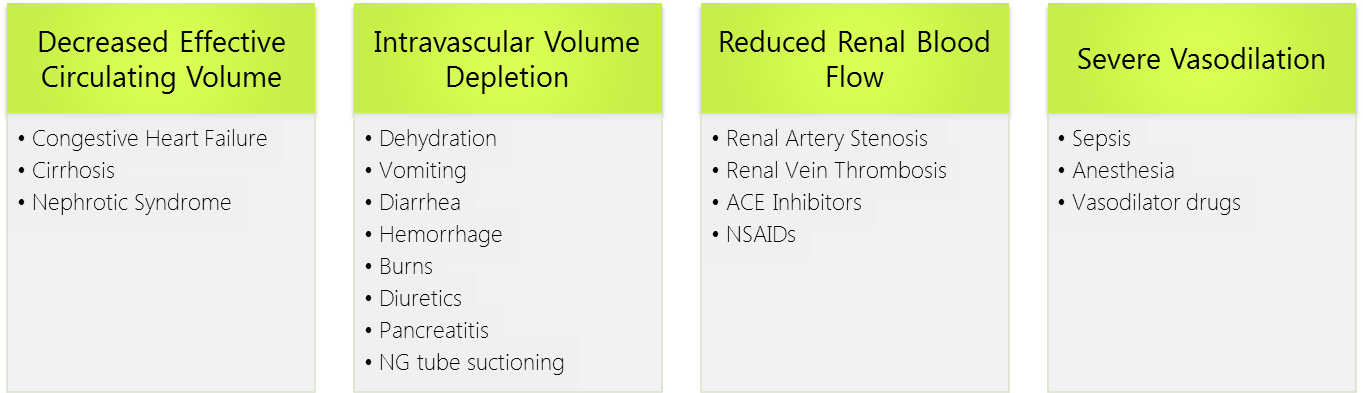
Prerenal AKI, known as prerenal azotemia, is by far the most common cause of AKI representing 30-50% of all cases. It is provoked by inadequate renal blood flow commonly due to decreased effective circulating blood flow. This causes a decrease in the intraglomerular hydrostatic pressure required to achieve proper glomerular filtration.
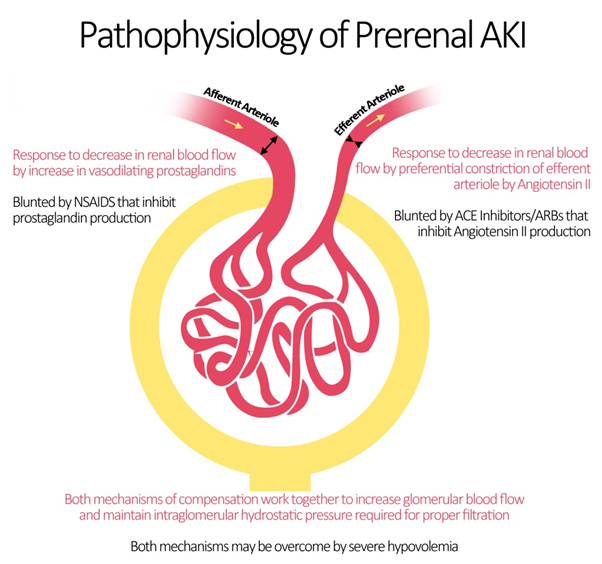
Blood flow to the kidneys can vary with systemic changes; however, glomerular perfusion pressure and GFR are maintained relatively constant by the kidney itself. Under physiologic conditions, minor drops in blood flow to the renal circulation are counteracted by changes in the resistances across the afferent and efferent arterioles of individual glomerular capillary beds.[12] The afferent arteriole vasodilates via 2 mechanisms.[13] The myogenic reflex, mediating medial smooth muscle relaxation in states of decrease perfusion pressure, vasodilates the afferent arteriole leading to increased blood flow.[14] Additionally, intrarenal synthesis of vasodilatory prostaglandins such as prostacyclin and prostaglandin E2 causes further dilation of the afferent arteriole.[15] The mechanism explains why the intake of NSAIDs leads to acute kidney injury by inhibiting this autoregulatory mechanism.[16]
At the level of the efferent arteriole, an increase in resistance is crucial for appropriate maintenance of glomerular hydrostatic pressure. This is achieved by an increase in the production of angiotensin II (via the Renin-Angiotensin System) which acts preferentially on the efferent arteriole leading to vasoconstriction.[17] Important medications that target angiotensin II production and action are ACE inhibitors (ACEIs) and angiotensin receptor blockers (ARBs) which may be responsible for renal decompensation in patients dependent on the action of angiotensin II to maintain glomerular perfusion pressure. Such is the case in chronic kidney disease patients, whose autoregulatory mechanisms are typically operating at maximum capacity.[18]
As such, the pathophysiology of prerenal azotemia entails a drop in renal plasma flow beyond the capacity of autoregulation, a blunted or inadequate renal compensation for an otherwise tolerable change in perfusion, or a combination of both. This eventually leads to ischemic renal injury particularly to the medulla which is maintained in hypoxic conditions at baseline. Causes of prerenal injury are summarized in the figure below. To note, as prerenal AKI progresses with further ischemia, it transforms into acute tubular necrosis (ATN) crossing into the realm of intrinsic AKI.
Intrinsic Renal AKI
Intrinsic renal AKI generally occurs due to renal parenchymal injury and may be classified according to the site of injury into: glomerular, tubular, interstitial, and vascular.
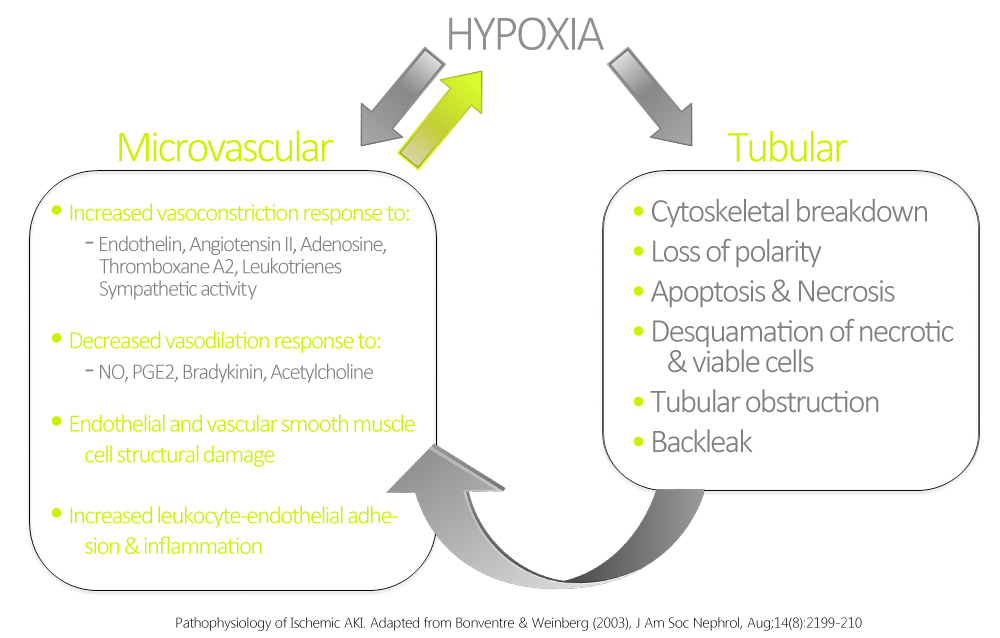
Tubular AKI
The most common form of intrinsic renal AKI involves damage to the renal tubules. In this context, the most common etiologies are sepsis, nephrotoxins, and ischemia. Ischemic AKI is part of a disease continuum involving prerenal AKI and manifests in states of prolonged renal blood flow compromise or renal hypoperfusion with other pre-existing or concomitant renal insults. Although sometimes dubbed acute tubular necrosis (ATN), ATN is non-specific to prerenal disease, and may be induced by sepsis and nephrotoxins. ATN is also not a very accurate pathological term, as renal biopsies have rarely shown true tubular necrosis, but rather tubular cell injury & apoptosis with secondary dysfunction are more accurate. These pathological manifestations are related to hypoxia and ATP depletion in areas that are physiologically hypoxic such as the renal medulla, and areas that are very metabolically active such as the proximal tubule. The response of the renal tubules and the microvasculature are maladaptive leading to a paradoxical increase in hypoxia and further damage and inflammation.[19] Ischemia and hypoxia are known to cause increased reactivity to vasoconstrictive agents, and decreased vasodilatory responses in arterioles as compared to normal kidneys.[20]
AKI is seen in 20 to 25% of cases of sepsis and in 50% of cases of septic shock. A decrease in GFR in a septic patient is usually a marker of poor prognosis, and the combination of sepsis and AKI is associated with a mortality rate of 70%. Although most cases of AKI occur with severe hemodynamic compromise in septic patients, renal injury may occur without overt hypotension. While there is clear tubular damage in sepsis-associated AKI, interstitial inflammation and interstitial edema have also been proposed in the pathogenesis.[21][22] The mechanisms of alteration of renal hemodynamics proposed in sepsis include excessive efferent arteriolar vasodilation or generalized renal vasoconstriction secondary to tumor necrosis factor induced release of endothelin.
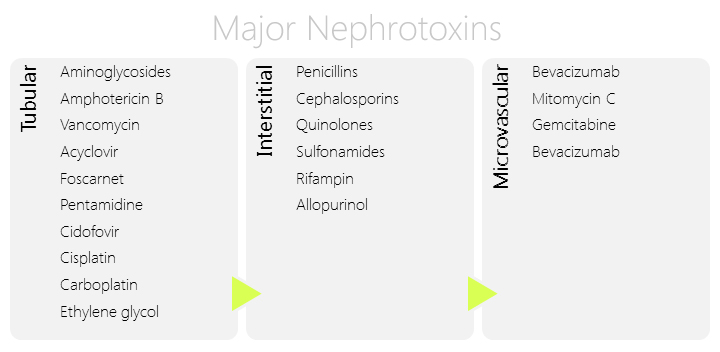
Another major cause of intrinsic renal AKI is nephrotoxins. The latter may be either endogenous such as myoglobin, hemoglobin, and myeloma light chains, or exogenous such as contrast agents, antibiotics, and chemotherapeutic agents. The kidney is a particularly susceptible organ to toxin injury mainly due to the high blood perfusion and the high concentration of substances in the kidneys destined for excretion. Nephrotoxic injury may be secondary to tubular, interstitial, or microvascular damage depending on the nephrotoxin itself. Major risk factors for nephrotoxic AKI include old age, pre-existing chronic kidney disease (CKD), and prerenal azotemia.[23]
Contrast induced nephropathy (CIN) recently called contrast induced AKI (CIAKI) is also major cause of intrinsic injury caused by iodinated contrast media used in cardiovascular imaging. This entity is virtually non-existent in healthy young individuals. Risk factors that increase susceptibility to contrast media include advanced age, pre-existing CKD, diabetic nephropathy, severe cardiac failure, and concomitant exposure to other nephrotoxins. The pathophysiology of CIN is not clearly understood; however, several attempts have been made to explain the underlying mechanism. It is generally agreed that CIN is due to a combination of several influences brought on by contrast-media infusion rather than a single process. The most important mechanism thought to be involved in CIN is a reduction in renal perfusion at the level of the microvasculature leading to tubular damage. This is attributed to several alterations in the renal microenvironment including activation of the tubuloglomerular feeback, local vasoactive metabolites including adenosine, prostaglandin, NO, and endothelin as well as increased interstitial pressure. Studies have also proposed injury to renal tubular cells may occur via a direct cytotoxic effect of the contrast media and via reactive oxygen species production.[24]
Glomerular & Vascular AKI
Glomerular damage causing AKI accounts for a small propotion of cases of AKI. Glomerulonephritis leading to AKI is usually seen in rapidly progressive glomerulonephritis (RPGN). Other forms of glomerulonephritis progress slowly and generally lead to chronic kidney disease. RPGN is characterized by a triad of hematuria, proteinuria, and hypertension progressing to a decrease in GFR and urine output.[25] RPGN can be idiopathic or secondary to SLE, Henoch Schonlein Purpura, Wegener’s Granulomatosis, and Goodpasture’s Syndrome. The pathophysiology is almost always related to an autoimmune insult, but specific characteristics depend on the underlying etiologies.[26]
Other causes of AKI of vascular origin include diseases affecting the macro and microvasculature not only confined to the glomerular capillaries. Examples include TTP/HUS & DIC associated with microangiopathic hemolytic anemia (MAHA) typically arising from an endothelial cell injury with subsequent leukocyte adhesion, complement consumption, platelet aggregation and eventual ischemic damage. Other causes include atheroemboli, calcineurin inhibitors in renal transplant patients via vasoconstriction of the afferent arterioles (although a tubulointerstitial pattern is also seen),[27] and vasculitides.[28]
Interstitial AKI
AKI may be secondary to acute interstitial nephritis caused by an idiosyncratic immune-mediated mechanism. Classically it is associated with a number of medications including penicillins, cephalosporins, NSAIDs, sulfonamides, and allopurinol. AIN can also be secondary to an infectious process, or systemic syndromes such as cryoglobulinemia, Sjogren syndrome, sarcoidosis, and primary biliary cirrhosis. Clinically, it may be associated with fever, and urinary eosinophilia although it may often be asymptomatic. Pathophysiology involves a cell-mediated immune reaction with interstitial infiltrates mostly composed of lymphocytes, macrophages, eosinophils, and plasma cells, with subsequent transformation into areas of interstitial fibrosis.[28]
Postrenal AKI
Postrenal AKI occurs due to an obstruction in the urinary flow leading to an increase in the intratubular hydrostatic pressure which interferes with proper glomerular filtration. Obstructions occurring at the level of the renal pelvis and the ureters must affect both kidneys simultaneously to cause AKI in healthy adults unless only one kidney is functional. Causes of upper tract obstructions may be intraluminal such as calculi or blood clots, transmural secondary to neoplastic invasion, or extrinsic compression by retroperitoneal fibrosis, neoplasia, or an abscess. The most common cause of postrenal AKI is bladder neck obstruction secondary to benign prostatic hypertrophy and prostate cancer. Other etiologies of lower urinary tract obstruction are calculi, blood clots and strictures. Patients usually have evident hydronephrosis unless early in the course of obstruction. [29]
Epidemiology and Demographics
AKI in the General Population
Most studies addressing the epidemiology of AKI focus on patients admitted to the hospital due to the high incidence of AKI in that setting. Ali el al conducted a retrospective cohort study in the Grampian region of Scotland involving 523,390 subjects for a span of 6 months. Their results showed an overall 6-month incidence of approximately 0.09% in the general population. The estimated yearly incidence was 1811 pmp for AKI without prior history of kidney disease. Out of the patients with AKI, 53% were males, 67.7% had full renal recovery, and 7.8% required renal replacement therapy. To note, the in-hospital mortality was estimated to be 32.7% while the 6-month mortality approached 50%. [11]
AKI in ICU Patients
Many studies have addressed the epidemiology of AKI in the intensive care unit with varying incidence rates. A trend of increasing incidence of is apparent with reported incidence of 4.9% in 1983, 7.2% in 2002, and up to 67% most recently.[30][31] Thakar et al reported an overall AKI incidence of 22% when studying 323,395 ICU patients admitted to the ICU in Veterans Affairs Hospitals across the USA, 17.5% of which matched the criteria for Stage 1 AKI.[32] The NEiPHROS-AKI study prospectively assessed the incidence rates of AKI in 19 ICUs in northeastern Italy in a 3-month period following the RIFLE criteria and showed a lower incidence of 10.8% in the cohort of 2164 patients.[33] Probably the highest recorded incidence came from Hoste et al who studied 5383 ICU patients with a reported rate of AKI of 67% according to the RIFLE criteria (Class R: 12%, Class I: 27%, Class F: 28%).[34] None of the studies showed any gender preponderance. Generally, lower incidence rates were seen in patients admitted for elective surgery and higher incidence in patients admitted for sepsis.[35]
Risk Factors
Risk assessment is an important step in the prevention of AKI especially when certain risk factors are preventable. Risk assessment includes both patient susceptibilities and exposures. Risk factors identified generally depend on the patient population studied.
- In ICU patients, those at the highest risk for developing AKI had one or more of the following risk factors: age more than 65 years, diabetes, presence of infection, acute circulatory or respiratory failure, past history of chronic heart failure (CHF), pre-existing kidney disease, lymphoma or leukemia, use of aminoglycosides, or cirrhosis.[36][37][38]
- In patients undergoing open heart surgery, major risk factors predisposing to postoperative AKI are advanced age, diabetes mellitus, hypertension, impaired left ventricular function, urgent operation or reoperation, prolonged cardiopulmonary bypass and aortic cross-clamp periods, hypothermia, re-exploration for bleeding or pericardial tamponade, systemic infection, peripheral vascular disease, cerebral vascular disease and COPD. CABG was associated with a higher risk for AKI than valve replacement surgery.[39][40]
- In patients exposed to contrast media especially in the context of coronary interventions, pre-existing renal disease is the most important risk factor for contrast induced-AKI (CIAKI). For that, it is indicated to carefully monitor the serum creatinine and GFR before and after PCI. Still, studies have not shown a clear GFR value below which risk of AKI increases drastically. Other important risk factors include, diabetes, hypertension, CHF, advanced age (especially >75), volume depletion, IABP, anemia, hemodynamic instability, concurrent nephrotoxic medications, and high osmolality or large volume of contrast media.[3]
| Exposures | Susceptibilities |
| Sepsis | Dehydration or volume depletion |
| Critical illness | Advanced age |
| Circulatory shock | Female gender |
| Burns | Black race |
| Trauma | CKD |
| Cardiac surgery (especially with cardiopulmonary bypass) | Chronic diseases (heart, lung, liver) |
| Major non-cardiac surgery | Diabetes mellitus |
| Nephrotoxic drugs | Cancer |
| Radiocontrast agents | Anemia |
| Poisonous plants and animals |
Differential Diagnosis
Natural History, Complications & Prognosis
Diagnosis
Signs and Symptoms
Signs and symptoms of AKI are limited and often unrecognized early on. The major clinical symptoms include decreased urine output and dark colored urine. Other symptoms are largely non-specific and related to azotemia. Patients may complain of malaise, nausea, pruritis, confusion, and a metallic taste. History should focus on determining the possible etiologies. History of volume depletion secondary to vomiting, diarrhea, or diuretics use should point to a pre-renal cause of AKI. Medications should be noted carefully for the intake of NSAIDs, ACE inhibitors, ARBs, and other medications with known nephrotoxic properties. A history of prostatic hypertrophy or cancer, nephrolithiasis, or malignancy could be a sign of post-renal obstruction.
Signs on physical exam may show volume overload, orthostatic hypotension, tachycardia, reduced jugular venous pressure, decreased skin turgor, and dry mucous membranes with asterixis and a friction rub occasionally present in late disease. [41]
Lab Findings
Clinical signs of AKI are scarce prompting aggressive laboratory surveillance especially in high-risk patients. With past diagnostic strategies, the diagnosis of AKI depended on an elevation of BUN and serum creatinine without response to a fluid challenge. However, this approach alone is not enough. Proper diagnosis and management on AKI requires careful examination of serum chemistries, urinary chemistries and sediments.
Diagnosis of AKI is usually made by documenting an acute elevation in BUN and serum creatinine. Serum creatinine is also used to monitor disease progression and may hint to the etiology of the acute insult. For example, prerenal azotemia usually causes a small increase in serum creatinine that returns to baseline with the improvement of hemodynamics while contrast-induced nephropathy usually causes a rise in serum creatinine 24–48 hours after exposure, peaking within 3 to 5 days, and resolving within 1 week.
AKI may also lead to severe electrolyte disturbances such as hyperkalemia, hyperphosphatemia, and hypocalcemia that need regular follow-up and may often need corrective measures. Other findings may also help detect the etiology of AKI and are disease specific.
| Blood Laboratory Finding | Related Etiologies |
| Severe hyperphosphatemia, hypocalcemia, elevated CPK and uric acid | Tumor Lysis Syndrome, Rhabdomyolysis |
| Increased anion gap and osmolal gap | Ethylene Glycol Poisoning |
| Low anion gap | Multiple Myeloma |
| Low complement levels and high titers of ANAs, ANCAs and cryoglobulins | Vasculitides |
| Severe anemia in the absence of bleeding | Hemolysis, Multiple Myeloma |
| Anemia, thrombocytopenia, schistocytes on peripheral blood smear, elevated LDH, and low haptoglobin | TTP, HUS, DIC |
| Peripheral eosinophilia | Acute interstitial nephritis, atheroembolic disease, polyarteritis nodosa, Churg-Strauss |
| Elevated BNP | Heart Failure |
| Bacteremia | Sepsis |
Urine is a very important marker of kidney function and injury, and a urinalysis is almost invariably a crucial tool for the detection of the etiology and site of injury in AKI. AKI may be defined by oliguria alone; however, urine output is not necessarily decreased. Urine should be noted for volume, color, specific gravity, proteinuria, hematuria, pyuria, and sodium and creatinine concentrations.
Careful urine sediment examination is essential and may show hyaline casts, granular casts, red blood cells casts and tubular epithelial cell casts each denoting a different site and etiology for the AKI For instance, RBC casts in the urine sediment strongly suggest a glomerular or vascular cause of AKI. Acute tubular necrosis secondary to ischemia classically gives muddy-brown casts, pigmented granular casts, and epithelial cell casts. Tumor lysis syndrome would show uric acid crystals in the urine. Still, it is important to correlate the urinary sediment examination to the clinical context since urinary sediment findings have a low specificity when used alone.
Several calculated indices can also be used in the diagnosis of AKI including BUN/creatinine ratio, fractional excretion of sodium & fractional excretion of urea. In prerenal azotemia, low tubular flow rate and enhanced recycling of urea causes an uneven elevation in the BUN compared to creatinine which may manifest as an elevated BUN/creatinine ratio (greater than 20:1). In intrinsic renal AKI however, urea reabsorption is not elevated, so BUN and serum creatinine concentrations increase proportionally usually preserving the BUN/creatinine ratio (10-20:1).
Another important index used in AKI is the fractional excretion of sodium (FENa). The FENa represents the fraction of filtered sodium load that is excreted in the urine and is a measure of tubular function by the kidney's ability to reabsorb sodium. The FENa is calculated by the following equation:
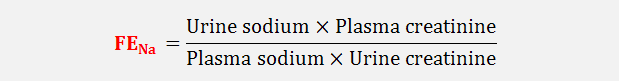
In prerenal azotemia, tubular function is preserved and sodium reabsorption increases with the associated renal vasoconstriction. Hence the FENa is usually <1% in prerenal azotemia. A high FENa in the context of prerenal azotemia is possible during diuretic treatment and glycosuria.
Another important index is the fractional excretion of urea (FEurea) calculated using the same equation for the fractional excretion of sodium. FEurea is of value in states of reduced effective circulating volume, and in cases where diuretics have been administered. In these situations, a low FEurea (<35%) has a higher sensitivity and specificity than FENa in differentiating between prerenal azotemia and renal AKI.
Novel Biomarkers
Treatment
Medical Therapy
Renal Replacement Therapy
Prophylaxis
Future or Investigational Therapies
AKI and Chronic Kidney Disease
See also
- BUN-to-creatinine ratio
- Chronic kidney disease
- Dialysis
- Renal failure
- Rhabdomyolysis
- Contrast-induced nephropathy
Related Chapters
References
- ↑ 1.0 1.1 Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P, Acute Dialysis Quality Initiative workgroup (2004). "Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group". Crit Care. 8 (4): R204–12. doi:10.1186/cc2872. PMC 522841. PMID 15312219.
- ↑ 2.0 2.1 Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG; et al. (2007). "Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury". Crit Care. 11 (2): R31. doi:10.1186/cc5713. PMC 2206446. PMID 17331245.
- ↑ 3.0 3.1 3.2 3.3 3.4 Kidney Disease Improving Global Outcomes Work Group (2012). "2012 KDIGO Clinical Practice Guideline for Acute Kidney Injury". Kidey Int Supp. 2: 69–88. doi:10.1038/kisup.2011.34.
- ↑ Beall D, Bywaters EG, Belsey RH, Miles JA (1941). "Crush Injury with Renal Failure". Br Med J. 1 (4185): 432–4. PMC 2161708. PMID 20783578 Check
|pmid=value (help). - ↑ LUCKE B (1946). "Lower nephron nephrosis; the renal lesions of the crush syndrome, of burns, transfusions, and other conditions affecting the lower segments of the nephrons". Mil Surg. 99 (5): 371–96. PMID 20276793.
- ↑ STRAUSS MB (1948). "Acute renal insufficiency due to lower-nephron nephrosis". N Engl J Med. 239 (19): 693–700. doi:10.1056/NEJM194811042391901. PMID 18892579.
- ↑ Bagshaw SM, George C, Bellomo R, ANZICS Database Management Committe (2008). "A comparison of the RIFLE and AKIN criteria for acute kidney injury in critically ill patients". Nephrol Dial Transplant. 23 (5): 1569–74. doi:10.1093/ndt/gfn009. PMID 18281319.
- ↑ Uchino S, Bellomo R, Goldsmith D, Bates S, Ronco C (2006). "An assessment of the RIFLE criteria for acute renal failure in hospitalized patients". Crit Care Med. 34 (7): 1913–7. doi:10.1097/01.CCM.0000224227.70642.4F. PMID 16715038.
- ↑ Bagshaw SM, George C, Dinu I, Bellomo R (2008). "A multi-centre evaluation of the RIFLE criteria for early acute kidney injury in critically ill patients". Nephrol Dial Transplant. 23 (4): 1203–10. doi:10.1093/ndt/gfm744. PMID 17962378.
- ↑ Ricci Z, Cruz D, Ronco C (2008). "The RIFLE criteria and mortality in acute kidney injury: A systematic review". Kidney Int. 73 (5): 538–46. doi:10.1038/sj.ki.5002743. PMID 18160961.
- ↑ 11.0 11.1 Ali T, Khan I, Simpson W, Prescott G, Townend J, Smith W; et al. (2007). "Incidence and outcomes in acute kidney injury: a comprehensive population-based study". J Am Soc Nephrol. 18 (4): 1292–8. doi:10.1681/ASN.2006070756. PMID 17314324.
- ↑ Loutzenhiser R, Griffin K, Williamson G, Bidani A (2006). "Renal autoregulation: new perspectives regarding the protective and regulatory roles of the underlying mechanisms". Am J Physiol Regul Integr Comp Physiol. 290 (5): R1153–67. doi:10.1152/ajpregu.00402.2005. PMC 1578723. PMID 16603656.
- ↑ Badr KF, Ichikawa I (1988). "Prerenal failure: a deleterious shift from renal compensation to decompensation". N Engl J Med. 319 (10): 623–9. doi:10.1056/NEJM198809083191007. PMID 3045546.
- ↑ Cupples WA, Braam B (2007). "Assessment of renal autoregulation". Am J Physiol Renal Physiol. 292 (4): F1105–23. doi:10.1152/ajprenal.00194.2006. PMID 17229679.
- ↑ Herbaczynska-Cedro K, Vane JR (1973). "Contribution of intrarenal generation of prostaglandin to autoregulation of renal blood flow in the dog". Circ Res. 33 (4): 428–36. PMID 4355037.
- ↑ Winkelmayer WC, Waikar SS, Mogun H, Solomon DH (2008). "Nonselective and cyclooxygenase-2-selective NSAIDs and acute kidney injury". Am J Med. 121 (12): 1092–8. doi:10.1016/j.amjmed.2008.06.035. PMID 19028206.
- ↑ Arendshorst WJ, Brännström K, Ruan X (1999). "Actions of angiotensin II on the renal microvasculature". J Am Soc Nephrol. 10 Suppl 11: S149–61. PMID 9892156.
- ↑ Abuelo JG (2007). "Normotensive ischemic acute renal failure". N Engl J Med. 357 (8): 797–805. doi:10.1056/NEJMra064398. PMID 17715412.
- ↑ Bonventre JV, Weinberg JM (2003). "Recent advances in the pathophysiology of ischemic acute renal failure". J Am Soc Nephrol. 14 (8): 2199–210. PMID 12874476.
- ↑ Conger JD, Weil JV (1995). "Abnormal vascular function following ischemia-reperfusion injury". J Investig Med. 43 (5): 431–42. PMID 8528754.
- ↑ Devarajan P (2006). "Update on mechanisms of ischemic acute kidney injury". J Am Soc Nephrol. 17 (6): 1503–20. doi:10.1681/ASN.2006010017. PMID 16707563.
- ↑ Bonventre JV (2010). "Pathophysiology of AKI: injury and normal and abnormal repair". Contrib Nephrol. 165: 9–17. doi:10.1159/000313738. PMID 20427950.
- ↑ Choudhury D, Ahmed Z (2006). "Drug-associated renal dysfunction and injury". Nat Clin Pract Nephrol. 2 (2): 80–91. doi:10.1038/ncpneph0076. PMID 16932399.
- ↑ Wong PC, Li Z, Guo J, Zhang A (2012). "Pathophysiology of contrast-induced nephropathy". Int J Cardiol. 158 (2): 186–92. doi:10.1016/j.ijcard.2011.06.115. PMID 21784541.
- ↑ Erwig LP, Rees AJ (1999). "Rapidly progressive glomerulonephritis". J Nephrol. 12 Suppl 2: S111–9. PMID 10688410.
- ↑ Chen YX, Chen N (2013). "Pathogenesis of rapidly progressive glomerulonephritis: what do we learn?". Contrib Nephrol. 181: 207–15. doi:10.1159/000348633. PMID 23689582.
- ↑ Naesens M, Kuypers DR, Sarwal M (2009). "Calcineurin inhibitor nephrotoxicity". Clin J Am Soc Nephrol. 4 (2): 481–508. doi:10.2215/CJN.04800908. PMID 19218475.
- ↑ 28.0 28.1 Ruggenenti P, Noris M, Remuzzi G (2001). "Thrombotic microangiopathy, hemolytic uremic syndrome, and thrombotic thrombocytopenic purpura". Kidney Int. 60 (3): 831–46. doi:10.1046/j.1523-1755.2001.060003831.x. PMID 11532079.
- ↑ Patel TV, Kumar S, Singh AK (2007). "Post-renal acute renal failure". Kidney Int. 72 (7): 890–4. doi:10.1038/sj.ki.5002301. PMID 17495862.
- ↑ Hou SH, Bushinsky DA, Wish JB, Cohen JJ, Harrington JT (1983). "Hospital-acquired renal insufficiency: a prospective study". Am J Med. 74 (2): 243–8. PMID 6824004.
- ↑ Nash K, Hafeez A, Hou S (2002). "Hospital-acquired renal insufficiency". Am J Kidney Dis. 39 (5): 930–6. doi:10.1053/ajkd.2002.32766. PMID 11979336 Check
|pmid=value (help). - ↑ Thakar CV, Christianson A, Freyberg R, Almenoff P, Render ML (2009). "Incidence and outcomes of acute kidney injury in intensive care units: a Veterans Administration study". Crit Care Med. 37 (9): 2552–8. doi:10.1097/CCM.0b013e3181a5906f. PMID 19602973.
- ↑ Cruz DN, Bolgan I, Perazella MA, Bonello M, de Cal M, Corradi V; et al. (2007). "North East Italian Prospective Hospital Renal Outcome Survey on Acute Kidney Injury (NEiPHROS-AKI): targeting the problem with the RIFLE Criteria". Clin J Am Soc Nephrol. 2 (3): 418–25. doi:10.2215/CJN.03361006. PMID 17699446.
- ↑ Hoste EA, Clermont G, Kersten A, Venkataraman R, Angus DC, De Bacquer D; et al. (2006). "RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: a cohort analysis". Crit Care. 10 (3): R73. doi:10.1186/cc4915. PMC 1550961. PMID 16696865.
- ↑ Case J, Khan S, Khalid R, Khan A (2013). "Epidemiology of acute kidney injury in the intensive care unit". Crit Care Res Pract. 2013: 479730. doi:10.1155/2013/479730. PMC 3618922. PMID 23573420.
- ↑ de Mendonça A, Vincent J, Suter PM, Moreno R, Dearden NM, Antonelli M, Takala J, Sprung C, Cantraine F (2007). "Acute renal failure in the ICU: risk factors and outcome evaluated by the SOFA score". Intensive Care Medicine. 26 (7): 915–21. doi:10.1007/s001340051281.
- ↑ Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S; et al. (2005). "Acute renal failure in critically ill patients: a multinational, multicenter study". JAMA. 294 (7): 813–8. doi:10.1001/jama.294.7.813. PMID 16106006.
- ↑ Mennel S, Barbazetto I, Meyer CH, Peter S, Stur M (2007). "Ocular photodynamic therapy--standard applications and new indications. Part 2. Review of the literature and personal experience". Ophthalmologica. 221 (5): 282–91. doi:10.1159/000104757. PMID 17728549.
- ↑ Thakar CV, Arrigain S, Worley S, Yared JP, Paganini EP (2005). "A clinical score to predict acute renal failure after cardiac surgery". J Am Soc Nephrol. 16 (1): 162–8. doi:10.1681/ASN.2004040331. PMID 15563569.
- ↑ Bahar I, Akgul A, Ozatik MA, Vural KM, Demirbag AE, Boran M; et al. (2005). "Acute renal failure following open heart surgery: risk factors and prognosis". Perfusion. 20 (6): 317–22. PMID 16363316.
- ↑ PALMER RA, HENRY EW (1957). "The clinical course of acute renal failure; observations on 54 cases". Can Med Assoc J. 77 (12): 1078–84. PMC 1824321. PMID 13489601.