Acrodermatitis enteropathica
| Acrodermatitis enteropathica | |
| ICD-10 | E83.2 |
|---|---|
| OMIM | 201100 |
| DiseasesDB | 29602 |
| eMedicine | derm/5 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Acrodermatitis enteropathica is an autosomal recessive disorder characterized by periorificial (around the natural orifices) and acral (in the limbs) dermatitis, alopecia (loss of hair), and diarrhea. Similar features may be present in acquired zinc deficiency. This disease also is related to deficiency of zinc due to congenital causes. Some synonyms of this condition are:
- Brandt Syndrome
- Danbolt-Cross Syndrome
- Congenital Zinc Deficiency
Pathogenesis
The genetic mutation of SLC39A4 gene on Chromosome 8q locus 24.3 appears to be the cause. The SLC39A4 gene appears to encode a transmembrane protein that serves as a zinc uptake protein. The features of the disease usually start manifesting as an infant is weaned from breast milk. This has led some scientists to suspect that human milk contains a beneficial substance that helps uptake of zinc and prevents the disease from being manifested while an infant is on breast milk.
Presentation
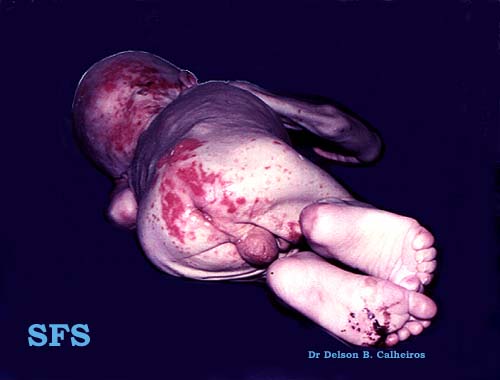
Features of acrodermatitis enteropathica start appearing in the first few months of life, as the infant discontinues breast milk. There are erythematous patches and plaques of dry, scaly skin. The lesions may appear eczematous, or may evolve further into crusted vesicles , bullas or pustules. The lesions are frequent around natural orifices like the mouth (peri-oral) and anus (peri-anal), and also in hands, feet and scalp. There may be suppurative inflammation of the nail fold surrounding the nail plate - known as paronychia. Alopecia - loss of hair from scalp, eyebrows and eyelashes may occur. The skin lesions may be secondarily infected by bacteria such as Staphylococcus aureus or fungi like Candida albicans. These skin lesions are accompanied by diarrhea.
Physical examination
Gallery
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
-
Acrodermatitis enteropathica. [http://www.atlasdermatologico.com.br/disease.jsf?diseaseId=12
Treatment
Without treatment, the disease is fatal and affected individuals may die within a few years. However, there is no absolute treatment of the condition. Lifelong dietary zinc supplementation in the range of greater than 1-2 mg/kg of bodyweight per day is usually needed.
External links
Organizations and resources
The following organizations provide information and patient support resources: