Abdominal aortic aneurysm history and symptoms
|
Abdominal Aortic Aneurysm Microchapters |
|
Differentiating Abdominal Aortic Aneurysm from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Abdominal aortic aneurysm history and symptoms On the Web |
|
Directions to Hospitals Treating Abdominal aortic aneurysm history and symptoms |
|
Risk calculators and risk factors for Abdominal aortic aneurysm history and symptoms |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
History & Symptoms
AAAs are commonly divided according to their size and symptomatology. An aneurysm is usually considered to be present if the measured outer aortic diameter is over 3 cm (normal diameter of aorta is around 2 cm). The natural history is of increasing diameter over time, followed eventually by the development of symptoms (usually rupture). If the outer diameter exceeds 5 cm, the aneurysm is considered to be large. For aneurysms under 5 cm, the risk of rupture is low, so that the risks of surgery usually outweigh the risk of rupture. Aneurysms less than 5cm are therefore usually kept under surveillance until such time as they become large enough to warrant repair, or develop symptoms.[1][2] The vast majority of aneurysms are asymptomatic. The risk of rupture is high in a symptomatic aneurysm, which is therefore considered an indication for surgery. Possible symptoms include low back pain, flank pain, abdominal pain, groin pain or pulsating abdominal mass.[3] The complications include rupture, peripheral embolisation, acute aortic occlusion, aortocaval or aortoduodenal fistulae. On physical examination, a palpable abdominal mass can be noted. Bruits can be present in case of renal or visceral arterial stenosis.[4]
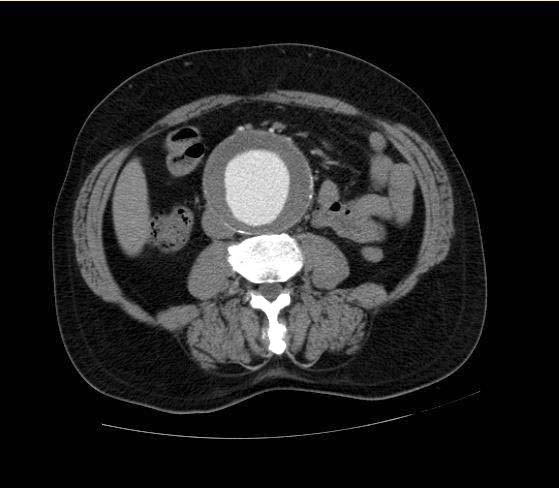
As most of the AAAs are asymptomatic, their presence is usually revealed during an abdominal examination for another reason - the most common being abdominal ultrasonography. A physician may also detect the presence of an AAA by abdominal palpation. Ultrasonography provides the initial assessment of the size and extent of the aneurysm, and is the usual modality for surveillance. Preoperative examinations include CT, MRI and special modes thereof, like CT/MR angiography. Angiography may be useful also, as an additional method of measurement for the planning of endoluminal repair. Note that an aneurysmal aorta may appear normal on angiogram, due to thrombus within the sac.
- Many AAAs are detected incidentally during cardiac catheterizations, computed tomography (CT), or magnetic resonance imaging (MRI) performed for unrelated reasons.
- Up to 50% of AAAs can be recognized on plain roentgenograms as a calcified aneurysmal wall.
- Spontaneous abdominal pain in a patient with a pulsatile epigastric mass or a known AAA may signal rupture into the retroperitoneum or leakage within the aneurysm wall
- This could lead to rapid expansion or imminent rupture.
- Peripheral embolization to the lower extremities (common in popliteal artery aneurysms) is rare with AAAs.
- Rarely in larger or unstable aneurysms, disseminated intravascular coagulopathy may develop.
References
Acknowledgements
The content on this page was first contributed by: C. Michael Gibson M.S., M.D.