Abciximab
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sheng Shi, M.D. [2]; Aparna Vuppala, M.B.B.S. [3]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Abciximab is a Platelet aggregation inhibitor that is FDA approved for the prophylaxis of cardiac ischemic complications in patients undergoing percutaneous coronary intervention and in patients with unstable angina not responding to conventional medical therapy when percutaneous coronary intervention is planned within 24 hours. Common adverse reactions include chest pain, hypotension, injection site pain, abdominal pain,nausea, vomiting, bleeding, backache.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Prevention of Cardiac Ischemic Complications in PCI
- Dosing Information
- Initial dosage: 0.25 mg/kg IV bolus (10-60 minutes before the start of PCI)
- Maitaining dosage: 0.125 mg/kg/min IV for 12 hours (max 10 ug/min)
Treatment of patient with unstable angina planned to undergo PCI within 24 hours
- Dosing Information
- Initial dosage: 0.25 mg/kg IV bolus (10-60 minutes before the start of PCI)
- Maitaining dosage: 10 ug/min IV for 18- 24h (concluding one hour after the PCI)
- The safety and efficacy of Abciximab have only been investigated with concomitant administration of heparin and aspirin
- In patients with failed PCIs, the continuous infusion of Abciximab should be stopped because there is no evidence for Abciximab efficacy in that setting.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Myocardial ischemia
- Developed by: American College of Cardiology Foundation (ACCF) and American Heart Association (AHA)
- Class of Recommendation: Class IIa
- Level of Evidence: Level A
- Recommendation
- initial dosage: 0.25 mg/kg IV bolus (over 5 minutes)
- maitaing dosage: 10 ug/min IV (continued for 12 hours unless complications developed)
Non–Guideline-Supported Use
Acute myocardial infarction
- Dosing information
- initial dosage: 0.25 mg/kg IV bolus’‘’
- maitaing dosage: 10 ug/min IV for 12h [1]
Acute arterial thrombosis
- Dosing information
- initial dosage: 0.25 mg/kg IV bolus
- maitaing dosage: 10 ug/min IV for 12h [2]
Cerebrovascular accident
- Dosing information
- initial dosage: 0.25 mg/kg IV bolus
- maitaing dosage: 10 ug/min IV for 12h [3]
Myocardial infarction
- Dosing information
- initial dosage: 0.25 mg/kg IV bolus
- maitaing dosage: 10 ug/min IV for 12h [4]
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
FDA Package Insert for Abciximab contains no information regarding Pediatric Indications and Dosage.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information about Off-Label Guideline-Supported Use of Abciximab in pediatric patients.
Non–Guideline-Supported Use
Aneurysm of coronary vessels
- Dosing information
- loading dose: 0.25 mg/kg IV
- follow-up: 0.125 mg/min IV for 12h [5]
Contraindications
Because Abciximab may increase the risk of bleeding, Abciximab is contraindicated in the following clinical situations:
- Active internal bleeding
- Recent (within six weeks) gastrointestinal (GI) or genitourinary (GU) bleeding of clinical significance.
- History of cerebrovascular accident (CVA) within two years, or CVA with a significant residual neurological deficit
- Bleeding diathesis
- Administration of oral anticoagulants within seven days unless prothrombin time is <1.2 times control
- Thrombocytopenia (<100,000 cells/mL)
- Recent (within six weeks) major surgery or trauma
- Intracranial neoplasm, arteriovenous malformation, or aneurysm
- Severe uncontrolled hypertension
- Presumed or documented history of vasculitis
- Use of intravenous dextran before PCI, or intent to use it during an intervention
Abciximab is also contraindicated in patients with known hypersensitivity to any component of this product or to murine proteins.
Warnings
Bleeding Events
Abciximab has the potential to increase the risk of bleeding events, rarely including those with a fatal outcome, particularly in the presence of anticoagulation, e.g., from heparin, other anticoagulants, or thrombolytics
The risk of major bleeds due to Abciximab therapy is increased in patients receiving thrombolytics and should be weighed against the anticipated benefits.
Should serious bleeding occur that is not controllable with pressure, the infusion of Abciximab and any concomitant heparin should be stopped.
Allergic Reactions (including anaphylaxis)
Allergic reactions, some of which were anaphylaxis (sometimes fatal), have been reported rarely in patients treated with ReoPro. Patients with allergic reactions should receive appropriate treatment. Treatment of anaphylaxis should include immediate discontinuation of ReoPro administration and initiation of resuscitative measures.
Precautions
Bleeding Precautions
To minimize the risk of bleeding with Abciximab, it is important to use a low-dose, weight-adjusted heparin regimen, a weight-adjusted Abciximab bolus and infusion, strict anticoagulation guidelines, careful vascular access site management, discontinuation of heparin after the procedure and early femoral arterial sheath removal.
Therapy with Abciximab requires careful attention to all potential bleeding sites including catheter insertion sites, arterial and venous puncture sites, cutdown sites, needle puncture sites, and gastrointestinal, genitourinary, pulmonary (alveolar), and retroperitoneal sites.
Arterial and venous punctures, intramuscular injections, and use of urinary catheters, nasotracheal intubation, nasogastric tubes and automatic blood pressure cuffs should be minimized. When obtaining intravenous access, non-compressible sites (e.g., subclavian or jugular veins) should be avoided. Saline or heparin locks should be considered for blood drawing. Vascular puncture sites should be documented and monitored. Gentle care should be provided when removing dressings.
Femoral artery access site
Arterial access site care is important to prevent bleeding. Care should be taken when attempting vascular access that only the anterior wall of the femoral artery is punctured, avoiding a Seldinger (through and through) technique for obtaining sheath access. Femoral vein sheath placement should be avoided unless needed. While the vascular sheath is in place, patients should be maintained on complete bed rest with the head of the bed ≤ 30° and the affected limb restrained in a straight position. Patients may be medicated for back/groin pain as necessary.
Discontinuation of heparin immediately upon completion of the procedure and removal of the arterial sheath within six hours is strongly recommended if APTT ≤ 50 sec or ACT≤ 175 sec . In all circumstances, heparin should be discontinued at least two hours prior to arterial sheath removal.
Following sheath removal, pressure should be applied to the femoral artery for at least 30 minutes using either manual compression or a mechanical device for hemostasis. A pressure dressing should be applied following hemostasis. The patient should be maintained on bed rest for six to eight hours following sheath removal or discontinuation of Abciximab, or four hours following discontinuation of heparin, whichever is later. The pressure dressing should be removed prior to ambulation. The sheath insertion site and distal pulses of affected leg(s) should be frequently checked while the femoral artery sheath is in place and for six hours after femoral artery sheath removal. Any hematoma should be measured and monitored for enlargement.
The following conditions have been associated with an increased risk of bleeding and may be additive with the effect of Abciximab in the angioplasty setting: PCI within 12 hours of the onset of symptoms for acute myocardial infarction, prolonged PCI (lasting more than 70 minutes) and failed PCI.
Use of Thrombolytics, Anticoagulants and Other Antiplatelet Agents
In the EPIC, EPILOG, CAPTURE, and EPISTENT trials, Abciximab was used concomitantly with heparin and aspirin.
For details of the anticoagulation algorithms used in these clinical trials,: Anticoagulation. Because Abciximab inhibits platelet aggregation, caution should be employed when it is used with other drugs that affect hemostasis, including thrombolytics, oral anticoagulants, non-steroidal anti-inflammatory drugs, dipyridamole, and ticlopidine.
In the EPIC trial, there was limited experience with the administration of Abciximab with low molecular weight dextran. Low molecular weight dextran was usually given for the deployment of a coronary stent, for which oral anticoagulants were also given. In the 11 patients who received low molecular weight dextran with Abciximab, five had major bleeding events and four had minor bleeding events. None of the five placebo patients treated with low molecular weight dextran had a major or minor bleeding event . Because of observed synergistic effects on bleeding, Abciximab therapy should be used judiciously in patients who have received systemic thrombolytic therapy. The GUSTO V trial randomized patients with acute myocardial infarction to treatment with combined Abciximab and half-dose Reteplase, or full-dose Reteplase alone (15). In this trial, the incidence of moderate or severe nonintracranial bleeding was increased in those patients receiving Abciximab and half-dose Reteplase versus those receiving Reteplase alone (4.6% versus 2.3%, respectively).
Thrombocytopenia
Thrombocytopenia, including severe thrombocytopenia, has been observed with Abciximab administration . Platelet counts should be monitored prior to, during, and after treatment with Abciximab. Acute decreases in platelet count should be differentiated between true thrombocytopenia and pseudothrombocytopenia . If true thrombocytopenia is verified, Abciximab should be immediately discontinued and the condition appropriately monitored and treated.
In clinical trials, patients who developed thrombocytopenia were followed with daily platelet counts until their platelet count returned to normal. Heparin and aspirin were discontinued for platelet counts below 60,000 cells/μL and platelets were transfused for a platelet count below 50,000 cells/μL. Most cases of severe thrombocytopenia (< 50,000 cells/μL) occurred within the first 24 hours of Abciximab administration.
In a registry study of Abciximab readministration, a history of thrombocytopenia associated with prior use of Abciximab was predictive of an increased risk of recurrent thrombocytopenia . Readministration within 30 days was associated with an increased incidence and severity of thrombocytopenia, as was a positive human anti-chimeric antibody (HACA) test at baseline, compared to the rates seen in studies with first administration.
Restoration of Platelet Function- In the event of serious uncontrolled bleeding or the need for emergency surgery, Abciximab should be discontinued. If platelet function does not return to normal, it may be restored, at least in part, with platelet transfusions.
Laboratory Tests
Before infusion of Abciximab, prothrombin time, ACT, APTT, and platelet count should be measured to identify pre-existing hemostatic abnormalities.
Based on an integrated analysis of data from all studies, the following guidelines may be utilized to minimize the risk for bleeding:
- When Abciximab is initiated 18 to 24 hours before PCI, the APTT should be maintained between 60 and 85 seconds during the Abciximab and heparin infusion period.
- If anticoagulation is continued in these patients following PCI, the APTT should be maintained between 55 and 75 seconds.
- The APTT or ACT should be checked prior to arterial sheath removal. The sheath should not be removed unless APTT ≤ 50 seconds or ACT ≤ 175 seconds.
- Platelet counts should be monitored prior to treatment, two to four hours following the bolus dose of Abciximab and at 24 hours or prior to discharge, whichever is first. If a patient experiences an acute platelet decrease (e.g., a platelet decrease to less than 100,000 cells/μL and a decrease of at least 25% from pre-treatment value), additional platelet counts should be determined. Platelet monitoring should continue until platelet counts return to normal.
- To exclude pseudothrombocytopenia, a laboratory artifact due to in vitro anticoagulant interaction, blood samples should be drawn in three separate tubes containing ethylenediaminetetraacetic acid (EDTA), citrate and heparin, respectively. A low platelet count in EDTA but not in heparin and/or citrate is supportive of a diagnosis of pseudothrombocytopenia.
Readministration
Administration of Abciximab may result in the formation of HACA that could potentially cause allergic or hypersensitivity reactions (including anaphylaxis), thrombocytopenia or diminished benefit upon readministration of Abciximab .
Readministration of Abciximab to patients undergoing PCI was assessed in a registry that included 1342 treatments in 1286 patients. Most patients were receiving their second Abciximab exposure; 15% were receiving the third or subsequent exposure. The overall rate of HACA positivity prior to the readministration was 6% and increased to 27% post-readministration. There were no reports of serious allergic reactions or anaphylaxis . Thrombocytopenia was observed at higher rates in the readministration study than in the phase 3 studies of first-time administration , suggesting that readministration may be associated with an increased incidence and severity of thrombocytopenia.
Adverse Reactions
Clinical Trials Experience
Bleeding
Abciximab has the potential to increase the risk of bleeding, particularly in the presence of anticoagulation, e.g., from heparin, other anticoagulants or thrombolytics. Bleeding in the Phase 3 trials was classified as major, minor or insignificant by the criteria of the Thrombolysis in Myocardial Infarction study group (16). Major bleeding events were defined as either an intracranial hemorrhage or a decrease in hemoglobin greater than 5 g/dL. Minor bleeding events included spontaneous gross hematuria, spontaneous hematemesis, observed blood loss with a hemoglobin decrease of more than 3 g/dL, or a decrease in hemoglobin of at least 4 g/dL without an identified bleeding site. Insignificant bleeding events were defined as a decrease in hemoglobin of less than 3 g/dL or a decrease in hemoglobin between 3-4 g/dL without observed bleeding. In patients who received transfusions, the number of units of blood lost was estimated through an adaptation of the method of Landefeld, et al. (17).
In the EPIC trial, in which a non-weight-adjusted, longer-duration heparin dose regimen was used, the most common complication during Abciximab therapy was bleeding during the first 36 hours. The incidences of major bleeding, minor bleeding and transfusion of blood products were significantly increased. Major bleeding occurred in 10.6% of patients in the Abciximab bolus plus infusion arm compared with 3.3% of patients in the placebo arm. Minor bleeding was seen in 16.8% of Abciximab bolus plus infusion patients and 9.2% of placebo patients (7). Approximately 70% of Abciximab-treated patients with major bleeding had bleeding at the arterial access site in the groin. Abciximab-treated patients also had a higher incidence of major bleeding events from gastrointestinal, genitourinary, retroperitoneal, and other sites.
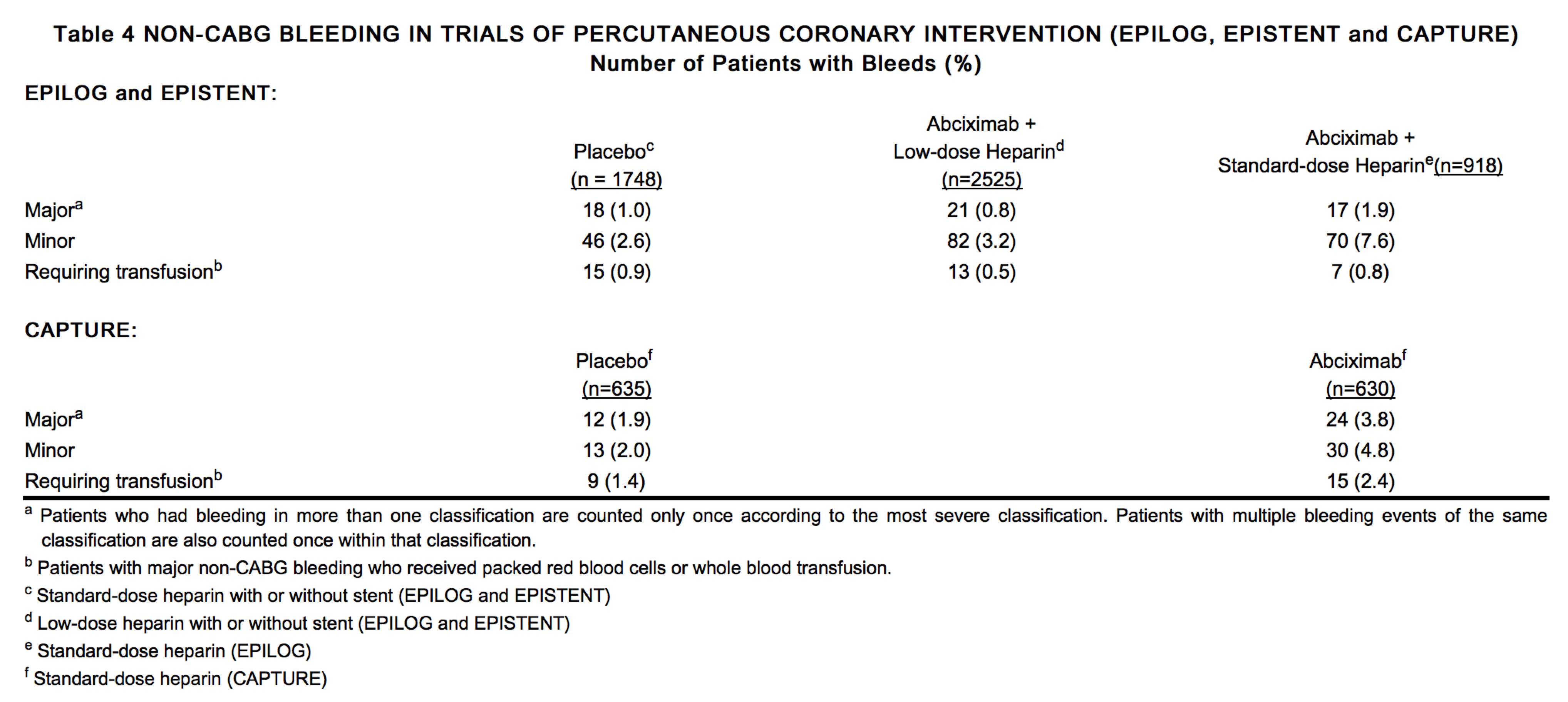
Bleeding rates were reduced in the CAPTURE trial, and further reduced in the EPILOG and EPISTENT trials by use of modified dosing regimens and specific patient management techniques. In EPILOG and EPISTENT, using the heparin and Abciximab dosing, sheath removal and arterial access site guidelines described under PRECAUTIONS, the incidence of major bleeding in patients treated with Abciximab and low-dose, weight-adjusted heparin was not significantly different from that in patients receiving placebo.
Subgroup analyses in the EPIC and CAPTURE trials showed that non-CABG major bleeding was more common in Abciximab patients weighing ≤ 75 kg. In the EPILOG and EPISTENT trials, which used weight-adjusted heparin dosing, the non-CABG major bleeding rates for Abciximab-treated patients did not differ substantially by weight subgroup.
Although data are limited, Abciximab treatment was not associated with excess major bleeding in patients who underwent CABG surgery. (The range among all treatment arms was 3-5% in EPIC, and 1-2% in the CAPTURE, EPILOG, and EPISTENT trials.) Some patients with prolonged bleeding times received platelet transfusions to correct the bleeding time prior to surgery.
The rates of major bleeding, minor bleeding and bleeding events requiring transfusions in the CAPTURE, EPILOG, and EPISTENT trials are shown in Table 4. The rates of insignificant bleeding events are not included in Table 4.
Cases of fatal bleeding have been reported rarely during post-marketing use of Abciximab Pulmonary alveolar hemorrhage has been rarely reported during use of Abciximab. This can present with any or all of the following in close association with ReoPro administration: hypoxemia, alveolar infiltrates on chest x-ray, hemoptysis, or an unexplained drop in hemoglobin.
Intracranial Hemorrhage and Stroke
The total incidence of intracranial hemorrhage and non-hemorrhagic stroke across all four trials was not significantly different, 9/3023 for placebo patients and 15/4680 for Abciximab-treated patients. The incidence of intracranial hemorrhage was 3/3023 for placebo patients and 7/4680 for Abciximab patients.
Thrombocytopenia
In the clinical trials, patients treated with Abciximab were more likely than patients treated with placebo to experience decreases in platelet counts.
Among patients in the EPILOG and EPISTENT trials who were treated with Abciximab plus low-dose heparin, the proportion of patients with any thrombocytopenia (platelets less than 100,000 cells/μL) ranged from 2.5 to 3.0%. The incidence of severe thrombocytopenia (platelets less than 50,000 cells/μL) ranged from 0.4 to 1.0% and platelet transfusions were required in 0.9 to 1.1%, respectively. Modestly lower rates were observed among patients treated with placebo plus standard-dose heparin. Overall higher rates were observed among patients in the EPIC and CAPTURE trials treated with Abciximab plus longer duration heparin: 2.6 to 5.2% were found to have any thrombocytopenia, 0.9 to 1.7% had severe thrombocytopenia, and 2.1 to 5.5% required platelet transfusion, respectively.
In a readministration registry study of patients receiving a second or subsequent exposure to Abciximab the incidence of any degree of thrombocytopenia was 5%, with an incidence of profound thrombocytopenia of 2% (<20,000 cell/μL). Factors associated with an increased risk of thrombocytopenia were a history of thrombocytopenia on previous Abciximab exposure, readministration within 30 days, and a positive HACA assay prior to the readministration.
Among 14 patients who had thrombocytopenia associated with a prior exposure to Abciximab, 7 (50%) had recurrent thrombocytopenia. In 130 patients with a readministration interval of 30 days or less, 25 (19%) developed thrombocytopenia. Severe thrombocytopenia occurred in 19 of these patients. Among the 71 patients who had a positive HACA assay at baseline, 11 (15%) developed thrombocytopenia, 7 of which were severe.
Allergic Reactions
There have been rare reports of allergic reactions, some of which were anaphylaxis .
Other Adverse Reactions
Table 5 shows adverse events other than bleeding and thrombocytopenia from the combined EPIC, EPILOG and CAPTURE trials which occurred in patients in the bolus plus infusion arm at an incidence of more than 0.5% higher than in those treated with placebo.
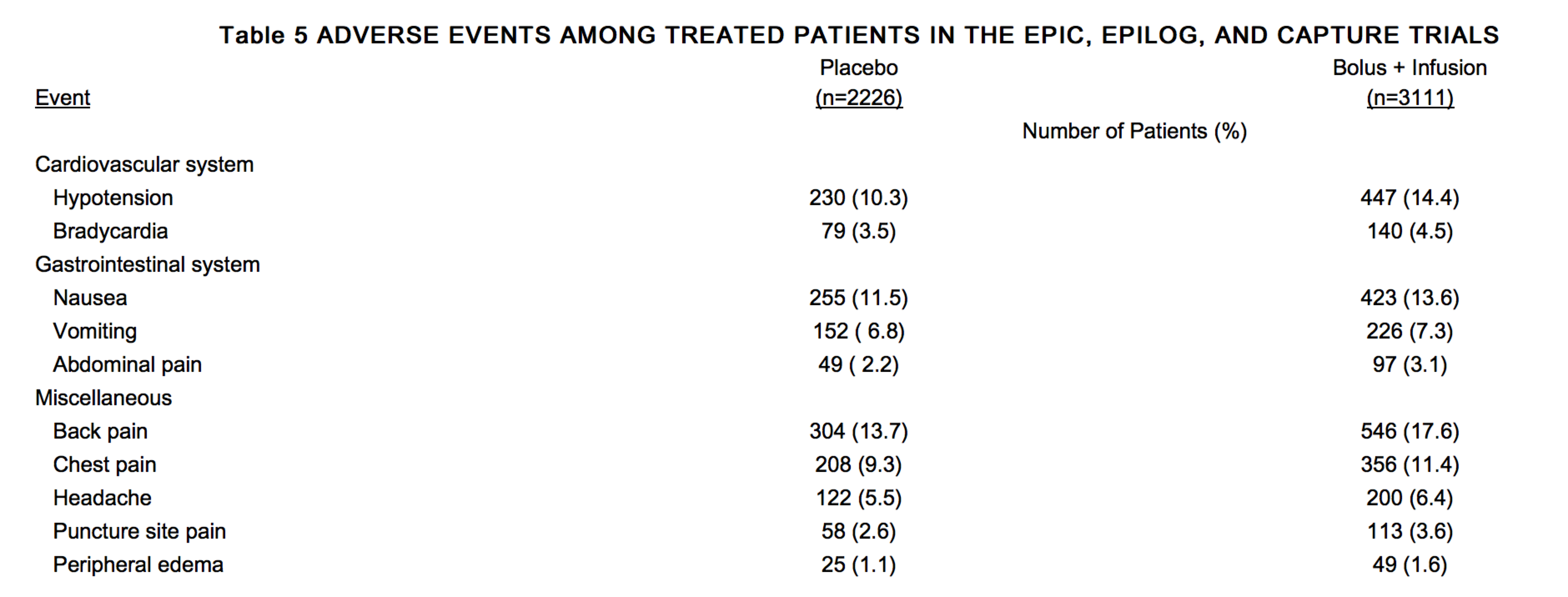
The following additional adverse events from the EPIC, EPILOG and CAPTURE trials were reported by investigators for patients treated with a bolus plus infusion of Abciximab at incidences which were less than 0.5% higher than for patients in the placebo arm.
Cardiovascular System: ventricular tachycardia (1.4%), pseudoaneurysm (0.8%), palpitation (0.5%), arteriovenous fistula (0.4%), incomplete AV block (0.3%), nodal arrhythmia (0.2%), complete AV block (0.1%), embolism (limb)(0.1%); thrombophlebitis (0.1%);
Gastrointestinal System: dyspepsia (2.1%), diarrhea (1.1%), ileus (0.1%), gastroesophogeal reflux (0.1%);
Hemic and Lymphatic System: anemia (1.3%), leukocytosis (0.5%), petechiae (0.2%);
Nervous System: dizziness (2.9%), anxiety (1.7%), abnormal thinking (1.3%), agitation (0.7%), hypesthesia (0.6%), confusion (0.5%) muscle contractions (0.4%), coma (0.2%), hypertonia (0.2%), diplopia (0.1%);
Respiratory System: pneumonia (0.4%), rales (0.4%), pleural effusion (0.3%), bronchitis (0.3%) bronchospasm (0.3%), pleurisy (0.2%), pulmonary embolism (0.2%), rhonchi (0.1%);
Musculoskeletal System: myalgia (0.2%);
Urogenital System: urinary retention (0.7%), dysuria (0.4%), abnormal renal function (0.4%), frequent micturition (0.1%), cystalgia (0.1%), urinary incontinence (0.1%), prostatitis (0.1%);
Miscellaneous: pain (5.4%), sweating increased (1.0%), asthenia (0.7%), incisional pain (0.6%), pruritus (0.5%), abnormal vision (0.3%), edema (0.3%), wound (0.2%), abscess (0.2%), cellulitis (0.2%), peripheral coldness (0.2%), injection site pain (0.1%), dry mouth (0.1%), pallor (0.1%), diabetes mellitus (0.1%), hyperkalemia (0.1%), enlarged abdomen (0.1%), bullous eruption (0.1%), inflammation (0.1%), drug toxicity (0.1%).
Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity. In the EPIC, EPILOG, and CAPTURE trials, positive HACA responses occurred in approximately 5.8% of these patients receiving a first exposure to Abciximab. No increase in hypersensitivity or allergic reactions was observed with Abciximab treatment .
In a study of readministration of Abciximab to patients the overall rate of HACA positivity prior to the readministration was 6% and increased post-readministration to 27%. Among the 36 subjects receiving a fourth or greater Abciximab exposure, HACA positive assays were observed post-readministration in 16 subjects (44%).
There were no reports of serious allergic reactions or anaphylaxis. HACA positive status was associated with an increased risk of thrombocytopenia . The data reflect the percentage of patients whose test results were considered positive for antibodies to Abciximab using an ELISA assay, and are highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody positivity in an assay may be influenced by several factors including sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to Abciximab with the incidence of antibodies to other products may be misleading.
Postmarketing Experience
FDA Package Insert for Abcixmab contains no information regarding Adverse Reactions.
Drug Interactions
Formal drug interaction studies with Abciximab have not been conducted. Abciximab has been administered to patients with ischemic heart disease treated concomitantly with a broad range of medications used in the treatment of angina, myocardial infarction and hypertension. These medications have included heparin, warfarin, beta-adrenergic receptor blockers, calcium channel antagonists, angiotensin converting enzyme inhibitors, intravenous and oral nitrates, ticlopidine, and aspirin. Heparin, other anticoagulants, thrombolytics, and antiplatelet agents are associated with an increase in bleeding. Patients with HACA titers may have allergic or hypersensitivity reactions when treated with other diagnostic or therapeutic monoclonal antibodies.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA):
Animal reproduction studies have not been conducted with Abciximab. It is also not known whether Abciximab can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Abciximab should be given to a pregnant woman only if clearly needed.
Pregnancy Category (AUS): C
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Abciximab in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Abciximab during labor and delivery.
Nursing Mothers
It is not known whether this drug is excreted in human milk or absorbed systemically after ingestion. Because many drugs are excreted in human milk, caution should be exercised when Abciximab is administered to a nursing woman.
Pediatric Use
Safety and effectiveness in pediatric patients have not been studied.
Geriatic Use
Of the total number of 7860 patients in the four Phase 3 trials, 2933 (37%) were 65 and over, while 653 (8%) were 75 and over. No overall differences in safety or efficacy were observed between patients of age 65 to less than 75 as compared to younger patients. The clinical experience is not adequate to determine whether patients of age 75 or greater respond differently than younger patients.
Gender
There is no FDA guidance on the use of Abciximab with respect to specific gender populations.
Race
There is no FDA guidance on the use of Abciximab with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Abciximab in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Abciximab in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Abciximab in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Abciximab in patients who are immunocompromised.
Administration and Monitoring
Administration
The safety and efficacy of Abciximab have only been investigated with concomitant administration of heparin and aspirin as described in clinical studies.
In patients with failed PCIs, the continuous infusion of Abciximab should be stopped because there is no evidence for Abciximab efficacy in that setting.
In the event of serious bleeding that cannot be controlled by compression, Abciximab and heparin should be discontinued immediately.
The recommended dosage of Abciximab in adults is a 0.25 mg/kg intravenous bolus administered 10-60 minutes before the start of PCI, followed by a continuous intravenous infusion of 0.125 μg/kg/min (to a maximum of 10 μg/min) for 12 hours.
Patients with unstable angina not responding to conventional medical therapy and who are planned to undergo PCI within 24 hours may be treated with an Abciximab 0.25 mg/kg intravenous bolus followed by an 18- to 24-hour intravenous infusion of 10 μg/min, concluding one hour after the PCI.
Instructions for Administration
Parenteral drug products should be inspected visually for particulate matter prior to administration. Preparations of Abciximab containing visibly opaque particles should NOT be used.
Hypersensitivity reactions should be anticipated whenever protein solutions such as Abciximab are administered. Epinephrine, dopamine, theophylline, antihistamines and corticosteroids should be available for immediate use. If symptoms of an allergic reaction or anaphylaxis appear, the infusion should be stopped and appropriate treatment given .
As with all parenteral drug products, aseptic procedures should be used during the administration of Abciximab.
Withdraw the necessary amount of Abciximab for bolus injection into a syringe. Filter the bolus injection using a sterile, non-pyrogenic, low protein-binding 0.2 or 5 μm syringe filter (Millipore SLGV025LS or SLSV025LS or equivalent).
Withdraw the necessary amount of Abciximab for the continuous infusion into a syringe. Inject into an appropriate container of sterile 0.9% saline or 5% dextrose and infuse at the calculated rate via a continuous infusion pump. The continuous infusion should be filtered either upon admixture using a sterile, non-pyrogenic, low protein-binding 0.2 or 5 μm syringe filter (Millipore SLGV025LS or SLSV025LS or equivalent) or upon administration using an in-line, sterile, non-pyrogenic, low protein-binding 0.2 or 0.22 μm filter (Abbott #4524 or equivalent). Discard the unused portion at the end of the infusion.
No incompatibilities have been shown with intravenous infusion fluids or commonly used cardiovascular drugs. Nevertheless, Abciximab should be administered in a separate intravenous line whenever possible and not mixed with other medications.
No incompatibilities have been observed with glass bottles or polyvinyl chloride bags and administration sets.
Monitoring
- Vascular puncture sites should be documented and monitored.
- Any hematoma should be measured and monitored for enlargement.
- Platelet counts should be monitored prior to, during, two to four hours following the bolus dose of Abciximab and at 24 hours or prior to discharge, whichever is first. If a patient experiences an acute platelet decrease (e.g., a platelet decrease to less than 100,000 cells/μL and a decrease of at least 25% from pre-treatment value), additional platelet counts should be determined. Platelet monitoring should continue until platelet counts return to normal.
- If true thrombocytopenia is verified, Abciximab should be immediately discontinued and the condition appropriately monitored and treated.
IV Compatibility
- No incompatibilities have been shown with intravenous infusion fluids or commonly used cardiovascular drugs. Nevertheless, Abciximab should be administered in a separate intravenous line whenever possible and not mixed with other medications.
- No incompatibilities have been observed with glass bottles or polyvinyl chloride bags and administration sets.
Overdosage
There has been no experience of overdosage in human clinical trials
Pharmacology
Mechanism of Action
The mechanism of action is thought to involve steric hindrance and/or conformational effects to block access of large molecules to the receptor rather than direct interaction with the RGD (arginine-glycine-aspartic acid) binding site of GPIIb/IIIa.
Structure
Abciximab, ReoPro®, is the Fab fragment of the chimeric human-murine monoclonal antibody 7E3. Abciximab binds to the glycoprotein (GP) IIb/IIIa receptor of human platelets and inhibits platelet aggregation. Abciximab also binds to the vitronectin (αvβ3) receptor found on platelets and vessel wall endothelial and smooth muscle cells.
The chimeric 7E3 antibody is produced by continuous perfusion in mammalian cell culture. The 47,615 dalton Fab fragment is purified from cell culture supernatant by a series of steps involving specific viral inactivation and removal procedures, digestion with papain and column chromatography.
ReoPro® is a clear, colorless, sterile, non-pyrogenic solution for intravenous (IV) use. Each single use vial contains 2 mg/mL of Abciximab in a buffered solution (pH 7.2) of 0.01 M sodium phosphate, 0.15 M sodium chloride and 0.001% polysorbate 80 in Water for Injection. No preservatives are added.
Pharmacodynamics
Intravenous administration in humans of single bolus doses of Abciximab from 0.15 mg/kg to 0.30 mg/kg produced rapid dose-dependent inhibition of platelet function as measured by ex vivo platelet aggregation in response to adenosine diphosphate (ADP) or by prolongation of bleeding time. At the two highest doses (0.25 and 0.30 mg/kg) at two hours post injection (the first time point evaluated), over 80% of the GPIIb/IIIa receptors were blocked and platelet aggregation in response to 20 μM ADP was almost abolished. The median bleeding time increased to over 30 minutes at both doses compared with a baseline value of approximately five minutes.
Intravenous administration in humans of a single bolus dose of 0.25 mg/kg followed by a continuous infusion of 10 μg/min for periods of 12 to 96 hours produced sustained high-grade GPIIb/IIIa receptor blockade (≥ 80%) and inhibition of platelet function (ex vivo platelet aggregation in response to 5 μM or 20 μM ADP less than 20% of baseline and bleeding time greater than 30 minutes) for the duration of the infusion in most patients. Similar results were obtained when a weight-adjusted infusion dose (0.125 μg/kg/min to a maximum of 10 μg/min) was used in patients weighing up to 80 kg. Results in patients who received the 0.25 mg/kg bolus followed by a 5 μg/min infusion for 24 hours showed a similar initial receptor blockade and inhibition of platelet aggregation, but the response was not maintained throughout the infusion period. The onset of Abciximab-mediated platelet inhibition following a 0.25 mg/kg bolus and 0.125 μg/kg/min infusion was rapid and platelet aggregation was reduced to less than 20% of baseline in 8 of 10 patients at 10 minutes after treatment initiation.
Low levels of GPIIb/IIIa receptor blockade are present for more than 10 days following cessation of the infusion. After discontinuation of Abciximab infusion, platelet function returns gradually to normal. Bleeding time returned to ≤ 12 minutes within 12 hours following the end of infusion in 15 of 20 patients (75%), and within 24 hours in 18 of 20 patients (90%). Ex vivo platelet aggregation in response to 5 μM ADP returned to ≥ 50% of baseline within 24 hours following the end of infusion in 11 of 32 patients (34%) and within 48 hours in 23 of 32 patients (72%). In response to 20 μM ADP, ex vivo platelet aggregation returned to ≥ 50% of baseline within 24 hours in 20 of 32 patients (62%) and within 48 hours in 28 of 32 patients (88%).
Pharmacokinetics
Following intravenous bolus administration, free plasma concentrations of Abciximab decrease rapidly with an initial half-life of less than 10 minutes and a second phase half-life of about 30 minutes, probably related to rapid binding to the platelet GPIIb/IIIa receptors. Platelet function generally recovers over the course of 48 hours (5,6), although Abciximab remains in the circulation for 15 days or more in a platelet-bound state. Intravenous administration of a 0.25 mg/kg bolus dose of Abciximab followed by continuous infusion of 10 μg/min (or a weight-adjusted infusion of 0.125 μg/kg/min to a maximum of 10 μg/min) produces approximately constant free plasma concentrations throughout the infusion. At the termination of the infusion period, free plasma concentrations fall rapidly for approximately six hours then decline at a slower rate.
Nonclinical Toxicology
In vitro and in vivo mutagenicity studies have not demonstrated any mutagenic effect. Long-term studies in animals have not been performed to evaluate the carcinogenic potential or effects on fertility in male or female animals.
Clinical Studies
Abciximab has been studied in four Phase 3 clinical trials, all of which evaluated the effect of Abciximab in patients undergoing percutaneous coronary intervention (PCI): in patients at high risk for abrupt closure of the treated coronary vessel (EPIC), in a broader group of patients (EPILOG), in unstable angina patients not responding to conventional medical therapy (CAPTURE), and in patients suitable for either conventional angioplasty/atherectomy or primary stent implantation (EPILOG Stent; EPISTENT). Percutaneous intervention included balloon angioplasty, atherectomy, or stent placement. All trials involved the use of various, concomitant heparin dose regimens and, unless contraindicated, aspirin (325 mg) was administered orally two hours prior to the planned procedure and then once daily.
EPIC was a multicenter, double-blind, placebo-controlled trial of Abciximab in patients undergoing percutaneous transluminal coronary angioplasty or atherectomy (PTCA) who were at high risk for abrupt closure of the treated coronary vessel (7). Patients were allocated to treatment with: 1) Abciximab bolus plus infusion for 12 hours; 2) Abciximab bolus plus placebo infusion, or; 3) placebo bolus plus infusion. All patients received concomitant heparin (10,000 to 12,000 U bolus followed by an infusion for 12 hours).
The primary endpoint was the composite of death, myocardial infarction (MI), or urgent intervention for recurrent ischemia within 30 days of randomization. The primary endpoint event rates in the Abciximab bolus plus infusion group were reduced mostly in the first 48 hours and this benefit was sustained through 30 days (7), 6 months (8), and three years (9).
EPILOG was a randomized, double-blind, multicenter, placebo-controlled trial which evaluated Abciximab in a broad population of patients undergoing PCI (excluding patients with myocardial infarction and unstable angina meeting the EPIC high risk criteria) (10). Study procedures emphasized discontinuation of heparin after the procedure with early femoral arterial sheath removal and careful access site management . EPILOG was a three-arm trial comparing Abciximab plus standard-dose heparin, Abciximab plus low-dose heparin, and placebo plus standard-dose heparin. Abciximab and heparin infusions were weight-adjusted in all arms. The Abciximab bolus plus infusion regimen was: 0.25 mg/kg bolus followed by a 0.125 μg/kg/min infusion (to a maximum of 10 μg/min) for 12 hours. The heparin regimen was either a standard-dose regimen (initial 100 U/kg bolus, target ACT ≥ 300 seconds) or a low-dose regimen (initial 70 U/kg bolus, target ACT ≥ 200 seconds).
The primary endpoint of the EPILOG trial was the composite of death or MI occurring within 30 days of PCI. The composite of death, MI, or urgent intervention was an important secondary endpoint. The endpoint events in the Abciximab treatment group were reduced mostly in the first 48 hours and this benefit was sustained through 30 days and six months (10) and one year (11). The (Kaplan-Meier) endpoint event rates at 30 days are shown in Table 1.
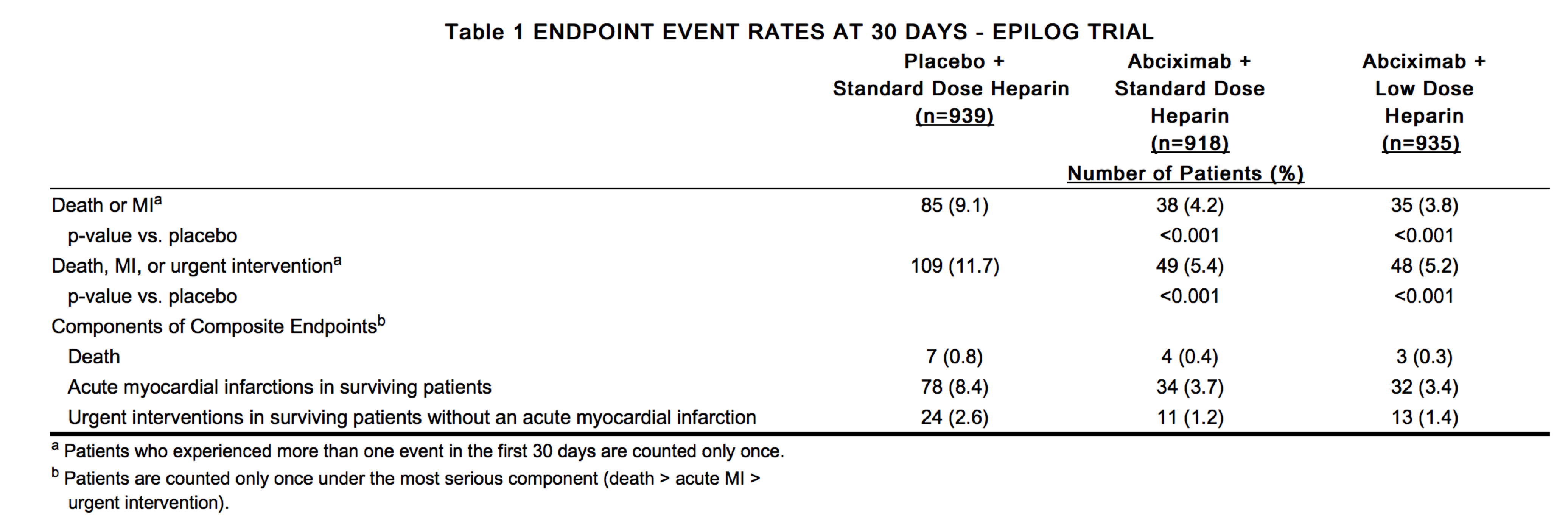
At the six-month follow up visit, the event rate for death, MI, or repeat (urgent or non-urgent) intervention remained lower in the Abciximab treatment arms (22.3% and 22.8%, respectively, for the standard- and low-dose heparin arms) than in the placebo arm (25.8%) and the event rate for death, MI, or urgent intervention was substantially lower in the Abciximab treatment arms (8.3% and 8.4%, respectively, for the standard- and low-dose heparin arms) than in the placebo arm (14.7%). The treatment associated effects continued to persist at the one-year follow up visit. The proportionate reductions in endpoint event rates were similar irrespective of the type of coronary intervention used (balloon angioplasty, atherectomy, or stent placement). Risk assessment using the American College of Cardiology/American Heart Association clinical/morphological criteria had large inter-observer variability. Consequently, a low risk subgroup could not be reproducibly identified in which to evaluate efficacy.
The EPISTENT trial was a randomized, multicenter trial evaluating three different treatment strategies in patients undergoing PCI: conventional PTCA with Abciximab plus low-dose heparin, primary intracoronary stent implantation with Abciximab plus low-dose heparin, and primary intracoronary stent implantation with placebo plus standard-dose heparin (12). The heparin dose was weight-adjusted in all arms. The JJIS Palmaz-Schatz stent was used in over 90% of the patients receiving stents. The two stent arms were blinded with respect to study agent (Abciximab or placebo) and heparin dose; the PCI arm with Abciximab was open-label. The Abciximab bolus plus infusion regimen was the same as that used in the EPILOG trial. The standard-dose and low-dose heparin regimens were the same as those used in the EPILOG trial. All patients were to receive aspirin; ticlopidine, if given, was to be started prior to study agent. Patient and access site management guidelines were the same as those for EPILOG, including a strong recommendation for early sheath removal.
The results demonstrated benefit in both Abciximab arms (i.e., with and without stents) compared with stenting alone on the composite of death, MI, or urgent intervention (repeat PCI or CABG) within 30 days of PCI (12). The (Kaplan-Meier) endpoint event rates at 30 days are shown in Table 2.
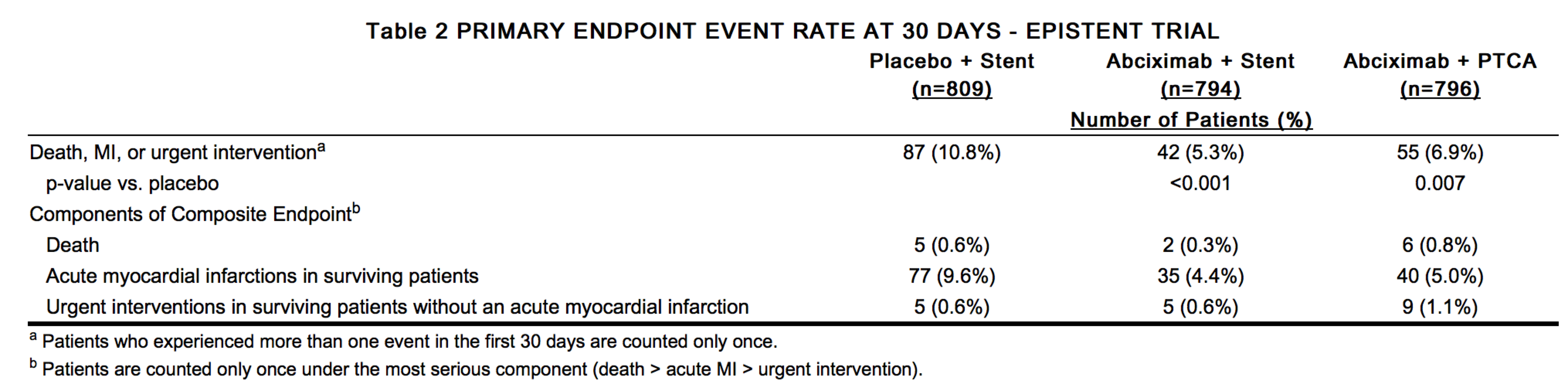
This benefit was maintained at 6 months: 12.1% of patients in the placebo/stent group experienced death, MI, or urgent revascularization compared with 6.4% of patients in the Abciximab/stent group (p<0.001 vs placebo/stent) and 9.2% in the Abciximab/PTCA group (p=0.051 vs placebo/stent). At 6 months, a reduction in the composite of death, MI, or all repeat (urgent or non-urgent) intervention was observed in the Abciximab/stent group compared with the placebo/stent group (15.4% vs 20.4%, p=0.006); the rate of this composite endpoint was similar in the Abciximab/PTCA and placebo/stent groups (22.4% vs 20.4%, p=0.467). (13)
CAPTURE was a randomized, double-blind, multicenter, placebo-controlled trial of the use of Abciximab in unstable angina patients not responding to conventional medical therapy for whom PCI was planned, but not immediately performed (14). The CAPTURE trial involved the administration of placebo or Abciximab starting 18 to 24 hours prior to PCI and continuing until one hour after completion of the intervention.
Patients were assessed as having unstable angina not responding to conventional medical therapy if they had at least one episode of myocardial ischemia despite bed rest and at least two hours of therapy with intravenous heparin and oral or intravenous nitrates. These patients were enrolled into the CAPTURE trial, if during a screening angiogram, they were determined to have a coronary lesion amenable to PCI. Patients received a bolus dose and intravenous infusion of placebo or Abciximab for 18 to 24 hours. At the end of the infusion period, the intervention was performed. The Abciximab or placebo infusion was discontinued one hour following the intervention. Patients were treated with intravenous heparin and oral or intravenous nitrates throughout the 18- to 24-hour Abciximab infusion period prior to the PCI.
The Abciximab dose was a 0.25 mg/kg bolus followed by a continuous infusion at a rate of 10 μg/min. The CAPTURE trial incorporated weight adjustment of the standard heparin dose only during the performance of the intervention, but did not investigate the effect of a lower heparin dose, and arterial sheaths were left in place for approximately 40 hours. The primary endpoint of the CAPTURE trial was the occurrence of any of the following events within 30 days of PCI: death, MI, or urgent intervention. The 30-day (Kaplan-Meier) primary endpoint event rates are shown in Table 3.
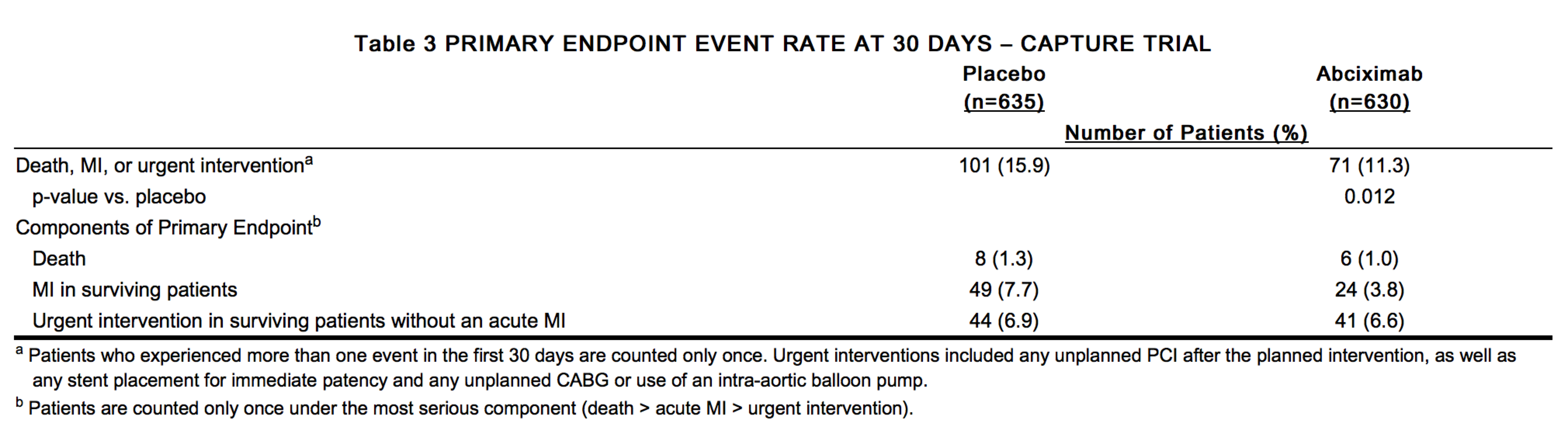
The 30-day results are consistent with the results of the other three trials, with the greatest effects on the myocardial infarction and urgent intervention components of the composite endpoint. As secondary endpoints, the components of the composite endpoint were analyzed separately for the period prior to the PCI and the period from the beginning of the intervention through Day 30. The greatest difference in MI occurred in the post-intervention period: the rates of MI were lower in the Abciximab group compared with placebo (Abciximab 3.6%, placebo 6.1%). There was also a reduction in MI occurring prior to the PCI (Abciximab 0.6%, placebo 2.0%). An Abciximab-associated reduction in the incidence of urgent intervention occurred in the post-intervention period. No effect on mortality was observed in either period. At six months of follow up, the composite endpoint of death, MI, or all repeat intervention (urgent or non-urgent) was not different between the Abciximab and placebo groups (Abciximab 31.0%, placebo 30.8%, p=0.77).
Mortality was uncommon in all four trials. Similar mortality rates were observed in all arms within each trial. Patient follow-up through one year of the EPISTENT trial suggested decreased mortality among patients treated with Abciximab and stent placement compared to patients treated with stent alone (8/794 vs. 19/809, p=0.037). Data from earlier studies with balloon angioplasty were not suggestive of the same benefit. In all four trials, the rates of acute MI were significantly lower in the groups treated with Abciximab. Most of the Abciximab treatment effect was seen in reduction in the rate of acute non-Q-wave MI. Urgent intervention rates were also lower in Abciximab-treated groups in these trials.
Anticoagulation
EPILOG and EPISTENT
Weight-adjusted low dose heparin, weight-adjusted Abciximab, careful vascular access site management and discontinuation of heparin after the procedure with early femoral arterial sheath removal were used.
The initial heparin bolus was based upon the results of the baseline ACT, according to the following regimen:
ACT < 150 seconds: administer 70 U/kg heparin
ACT 150 - 199 seconds: administer 50 U/kg heparin
ACT ≥ 200 seconds: administer no heparin
Additional 20 U/kg heparin boluses were given to achieve and maintain an ACT of ≥ 200 seconds during the procedure.
Discontinuation of heparin immediately after the procedure and removal of the arterial sheath within six hours were strongly recommended in the trials. If prolonged heparin therapy or delayed sheath removal was clinically indicated, heparin was adjusted to keep the APTT at a target of 60 to 85 seconds (EPILOG) or 55 to 75 seconds (EPISTENT).
CAPTURE trial
Anticoagulation was initiated prior to the administration of Abciximab. Anticoagulation was initiated with an intravenous heparin infusion to achieve a target APTT of 60 to 85 seconds. The heparin infusion was not uniformly weight adjusted in this trial. The heparin infusion was maintained during the Abciximab infusion and was adjusted to achieve an ACT of 300 seconds or an APTT of 70 seconds during the PCI. Following the intervention, heparin management was as outlined above for the EPILOG trial.
How Supplied
Abciximab (ReoPro®) 2 mg/mL is supplied in 5 mL vials containing 10 mg (NDC 0002-7140-01).
Storage
Vials should be stored at 2 to 8 °C (36 to 46 °F). Do not freeze. Do not shake. Do not use beyond the expiration date. Discard any unused portion left in the vial
Images
Drug Images
{{#ask: Page Name::Abciximab |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Abciximab |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
FDA Package Insert for Abciximab contains no information regarding Patient Information.
Precautions with Alcohol
Alcohol-Abciximab interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
There is limited information regarding Abciximab Brand Names in the drug label.
Look-Alike Drug Names
There is limited information regarding Abciximab Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Giri S, Mitchel J, Azar RR, Kiernan FJ, Fram DB, McKay RG et al. (2002) Results of primary percutaneous transluminal coronary angioplasty plus abciximab with or without stenting for acute myocardial infarction complicated by cardiogenic shock. Am J Cardiol 89 (2):126-31. PMID: 11792329
- ↑ Duda SH, Tepe G, Luz O, Ouriel K, Dietz K, Hahn U et al. (2001) Peripheral artery occlusion: treatment with abciximab plus urokinase versus with urokinase alone--a randomized pilot trial (the PROMPT Study). Platelet Receptor Antibodies in Order to Manage Peripheral Artery Thrombosis. Radiology 221 (3):689-96. DOI:10.1148/radiol.2213010400 PMID: 11719664
- ↑ Abciximab in Ischemic Stroke Investigators (2000) Abciximab in acute ischemic stroke. A randomized, double-blind, placebo-controlled, dose-escalation study. Stroke 31 (3):601-9. PMID: 10700492
- ↑ (2000) Trial of abciximab with and without low-dose reteplase for acute myocardial infarction. Strategies for Patency Enhancement in the Emergency Department (SPEED) Group. Circulation 101 (24):2788-94. PMID: 10859283
- ↑ Williams RV, Wilke VM, Tani LY, Minich LL (2002) Does Abciximab enhance regression of coronary aneurysms resulting from Kawasaki disease? Pediatrics 109 (1):E4. PMID: 11773572
{{#subobject:
|Label Page=Abciximab |Label Name=Abciximab label 01.jpg
}}
{{#subobject:
|Label Page=Abciximab |Label Name=Abciximab panel 01.jpg
}}