|
|
| (40 intermediate revisions by 6 users not shown) |
| Line 1: |
Line 1: |
| | __NOTOC__ |
| {{Infobox_Disease | | | {{Infobox_Disease | |
| Name = {{PAGENAME}} | | | Name = {{PAGENAME}} | |
| Image = AV nodal reentrant tachycardia.png | | | Image = AV nodal reentrant tachycardia.png | |
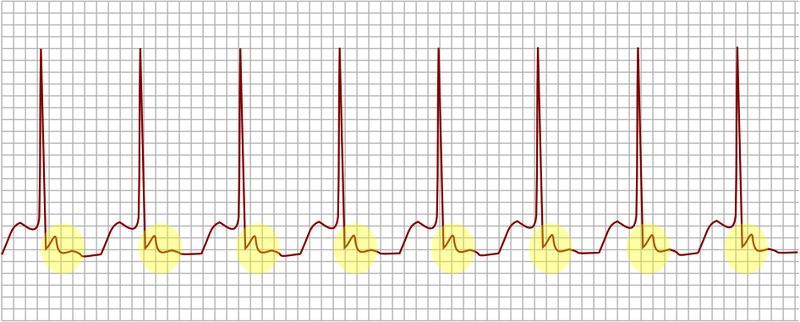
| Caption = AV nodal reentrant tachycardia. In yellow, is evidenced the P wave that falls after the QRS complex.| | | Caption = AV nodal reentrant tachycardia, uncommon variant with antegrade conduction down the slow pathway. In yellow, is evidenced the P wave that falls after the QRS complex.| |
| DiseasesDB = | | | DiseasesDB = | |
| ICD10 = {{ICD10|I|47|1|i|30}} | | | ICD10 = {{ICD10|I|47|1|i|30}} | |
| Line 15: |
Line 16: |
| }} | | }} |
| {{AVNRT}} | | {{AVNRT}} |
| {{CMG}} | | {{CMG}} : {{AE}} {{RG}} |
|
| |
|
| {{SK}} AVNRT; AV node reentrant tachycardia; AV nodal reentry tachycardia; AV node reentry tachycardia; atrioventricular node reentrant tachycardia; atrioventricular nodal reentry tachycardia; atrioventricular node reentry tachycardia; | | {{SK}} AVNRT; AV node reentrant tachycardia; AV nodal reentry tachycardia; AV node reentry tachycardia; atrioventricular node reentrant tachycardia; atrioventricular nodal reentry tachycardia; atrioventricular node reentry tachycardia; junctional reciprocating tachycardia; reciprocal or reciprocating AV nodal reentrant tachycardia |
|
| |
|
| ==Overview== | | ==[[AVNRT overview|Overview]]== |
| AV nodal reentrant tachycardia is a type of [[tachycardia]] (fast rhythm) of the [[heart]]. It is one of several types of [[supraventricular tachycardia]] ([[SVT]]), and like all [[SVTs]] the electrical impulse originates proximal to the [[bundle of HIS]]. In the case of AVNRT, the electrical impulse originates in the [[AV node]] and the immediately surrounding tissue. AVNRT is the most common cause of [[supraventricular tachycardia]].
| |
|
| |
|
| ==[[AVNRT historical perspective|Historical Perspective]]== | | ==[[AVNRT historical perspective|Historical Perspective]]== |
|
| |
|
| ==Pathophysiology== | | ==[[AVNRT classification|Classification]]== |
| AVNRT occurs when a [[cardiac arrhythmia#re-entry|reentry]] circuit forms within or just next to the [[AV node|atrioventricular node]]. The circuit usually involves two anatomical pathways: the fast pathway and the slow pathway, which are both in the [[right atrium]]. The slow pathway (which is usually targeted for ablation) is located inferiorly and slightly posterior to the [[AV node]], often following the anterior margin of the [[coronary sinus]]. The fast pathway is usually located just superior and posterior to the [[AV node]]. These pathways are formed from tissue that behaves very much like the AV node, and some authors regard them as ''part of'' the AV node. In the usual form of AVNRT, the conduction from the atrium to the ventricle is down the slow pathway, and the retrograde conduction from the ventricle to the atrium is up the fast pathway.
| |
|
| |
|
| ===Electrophysiologic Triggers=== | | ==[[AVNRT pathophysiology|Pathophysiology]]== |
| ====Premature Atrial Complex====
| |
| The most common trigger for an episode of AVNRT is when an [[atrial premature complex]] (APC) approaches the fast pathway, and is blocked due to the longer refractory period of this pathway, and instead conducts down the slow pathway. As the impulse goes down the slow pathway, the fast pathway recovers, and allows the impulse to conduct backward or retrograde toward the atrium. It then re-enters the atrial entrance of the slow pathway and the cycle repeats itself.
| |
|
| |
|
| ====Premature Ventricular Complex==== | | ==[[AVNRT causes|Causes]]== |
| The second most common mechanism whereby AVNRT is triggered is via the entry of a [[premature ventricular complex]] down either the slow conducting pathway (similar to a [[premature atrial complex]] above) or down the rapidly conducting pathway.
| |
|
| |
|
| ==Classification== | | ==[[AVNRT differential diagnosis|Differentiating AVNRT from other Disorders]]== |
| There are several types of AVNRT. The "common form" or "usual" AVNRT utilizes the slow AV nodal pathway as the anterograde limb of the circuit and the fast AV nodal pathway as the retrograde limb. The reentry circuit can be reversed such that the fast AV nodal pathway is the anterograde limb and the slow AV nodal pathway is the retrograde limb. This, not surprisingly is referred to as the "uncommon form" of AVNRT. However, there is also a third type of AVNRT that utilizes the slow AV nodal pathway as the anterograde limb and left atrial fibers that approach the AV node from the left side of the inter-atrial septum as the retrograde limb. This is known as atypical, or [[Slow-Slow AVNRT]].
| |
|
| |
|
| ===Common AVNRT=== | | ==[[AVNRT epidemiology and demographics|Epidemiology and Demographics]]== |
| In common AVNRT, the anterograde conduction is via the slow pathway and the retrograde conduction is via the fast pathway ([["slow-fast" AVNRT]]). This accounts for 80%-90% of cases of AVNRT.
| |
|
| |
|
| Because the retrograde conduction is via the fast pathway, stimulation of the atria (which produces the inverted P wave) will occur at the same time as stimulation of the ventricles (which causes the QRS complex). As a result, the inverted P waves may not be seen on the surface [[ECG]] since they are buried with the QRS complexes. Often the [[retrograde p-wave]] is visible, but also in continuity with the QRS complex, appearing as a "pseudo R prime" wave in lead V1 or a "pseudo S" wave in the inferior leads.
| | ==[[AVNRT risk factors|Risk Factors]]== |
|
| |
|
| ===Uncommon AVNRT=== | | ==[[AVNRT natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
| In uncommon AVNRT, the anterograde conduction is via the fast pathway and the retrograde conduction is via the slow pathway ([["fast-slow" AVNRT]]). Multiple slow pathways can exist so that both anterograde and retrograde conduction are over slow pathways. ([["slow-slow" AVNRT]]).
| |
| | |
| Because the retrograde conduction is via the slow pathway, stimulation of the atria will be delayed by the slow conduction tissue and will typically produce an inverted P wave that falls after the QRS complex on the surface [[ECG]].
| |
| | |
| ===Detailed Chapters on AVNRT Variants===
| |
| #[[AVNRT Slow/Fast]]
| |
| #[[AVNRT Fast/Slow]]
| |
| #[[AVNRT Slow/Slow]]
| |
| #[[AVNRT Slow/Fast Left Variant]]
| |
| | |
| ==Risk Factors==
| |
| Underlying structural heart disease is generally absent. Often, there is no precipitant of an episode. Risk factors for precipitation of AVNRT include:
| |
| *[[Alcohol]]
| |
| *[[Caffeine]]
| |
| *[[Chocolate]]
| |
| *[[Hyperthyroidism]]
| |
| *[[Hypokalemia]]
| |
| *[[Hypomagnesemia]]
| |
| *[[Myocardial ischemia]]
| |
| *[[Psychological stress]]
| |
| *[[Tea]]
| |
| *[[Theobromine]] in foods like tea, coffee and chocolate
| |
| *[[Theophylline]]
| |
| | |
| ==Differentiating Supraventricular Tachycardias==
| |
| [[Supraventricular tachycardias]] must be differentiated from each other because the managment strategies may vary:
| |
| | |
| ===[[Atrial Fibrillation]]===
| |
| *''Rate'': 110 to 180 bpm
| |
| *''Rhythm'': Irregularly irregular
| |
| *''[[P waves]]'': Absent, fibrillatory waves
| |
| *''[[PR interval]]'': Absent
| |
| *''[[QRS complex]]'': Less than 0.12 seconds, consistent, and normal in morphology in the absence of abberant conduction
| |
| *''Response to Maneuvers'': Does not break with [[adenosine]] or [[vagal maneuvers]]
| |
| *''Epidemiology and Demographics'': More common in the elderly, following [[bypass surgery]], in mitral valve disease, [[hyperthyroidism]]
| |
| | |
| ===[[Atrial Flutter]]===
| |
| *''Rate'': 75 (4:1 block), 100 (3:1 block) and 150 (2:1 block) bpm, but 150 is most common
| |
| *''Rhythm'': Regular
| |
| *''[[P waves]]'': Sawtooth pattern of [[P waves]] at 250 to 350 beats per minute
| |
| *''[[PR interval]]'': Varies depending upon the magnitude of the block, but is short
| |
| *''[[QRS complex]]'': Less than 0.12 seconds, consistent, and normal in morphology
| |
| *''Response to Maneuvers'': Conduction may vary in response to drugs and maneuvers dropping the rate from 150 to 100 or to 75 bpm
| |
| *''Epidemiology and Demographics'': More common in the elderly, after alcohol
| |
| | |
| ===[[AV Nodal Reentry Tachycardia]]===
| |
| *''Rate'': In adults the range is 140-250 bpm, but in children the rate can exceed 250 bpm.
| |
| *''Rhythm'': Regular
| |
| *''[[P waves]]'': The [[p wave]] is usually superimposed on or buried within the [[QRS complex]]
| |
| *''[[PR interval]]'': The [[PR interval]] cannot be calculated as the [[p wave]] is generally obscured by the [[QRS complex]]. In uncommon AVNRT, the [[p wave]] can appear after the [[QRS complex]] and before the [[T wave]], and in atypical AVNRT, the [[p wave]] can appear just before the [[QRS complex]].
| |
| *''[[QRS complex]]'': Less than 0.12 seconds, consistent, and normal in morphology in the absence of abberant conduction, [[QRS alternans]] may be present
| |
| *''Response to Maneuvers'': May break with [[adenosine]] or [[vagal maneuvers]]
| |
| *''Epidemiology and Demographics'': Accounts for 60%-70% of all SVTs. 80% to 90% of cases are due to antegrade conduction down a slow pathway and retrograde up a fast pathway.
| |
| | |
| ===[[AV Reciprocating Tachycardia]]===
| |
| *''Rate'': More rapid than AVNRT
| |
| *''Rhythm'':
| |
| *''[[P waves]]'':
| |
| *''[[PR interval]]'':
| |
| *''[[QRS complex]]'': Less than 0.12 seconds, consistent, and normal in morphology
| |
| *''Response to Maneuvers'': May break with [[adenosine]] or [[vagal maneuvers]]
| |
| *''Epidemiology and Demographics'': More common in males, whereas AVNRT is more common in females, Occurs at a younger age
| |
| | |
| ===[[Junctional Tachycardia]]===
| |
| *''Rate'': > 60 beats per minute
| |
| *''Rhythm'': Regular
| |
| *''[[P waves]]'': Usually inverted, may be burried in the QRS complex
| |
| *''[[PR interval]]'': The [[p wave]] is usually buried in the [[QRS complex]]
| |
| *''[[QRS complex]]'': Less than 0.12 seconds, consistent, and normal in morphology
| |
| *''Response to Maneuvers'': Does not break with [[adenosine]] or [[vagal maneuvers]]
| |
| *''Epidemiology and Demographics'': Common after [[heart surgery]], [[digoxin toxicity]], as an escape rhythm in [[AV block]]
| |
| | |
| ===[[Multifocal Atrial Tachycardia]]===
| |
| | |
| *''Rate'': Atrial rate is > 100 beats per minute (bpm)
| |
| *''Rhythm'':
| |
| *''[[P waves]]'': [[P waves]] of varying morphology from at least three different foci, absence of one dominant atrial pacemaker, can be mistaken for [[atrial fibrillation]] if the [[P waves]] are of low amplitude
| |
| *''[[PR interval]]'': Variable [[PR interval]]s, [[RR interval]]s, and [[PP interval]]s
| |
| *''[[QRS complex]]'': Less than 0.12 seconds, consistent, and normal in morphology
| |
| *''Response to Maneuvers'': Does not terminate with [[adenosine]] or [[vagal maneuvers]]
| |
| *''Epidemiology and Demographics'': * High incidence in the elderly and in those with [[COPD]]
| |
| | |
| ===[[Sinus Node Reentry Tachycardia]]===
| |
| *''Rate'':
| |
| *''Rhythm'':
| |
| *''[[P waves]]'': Upright [[P waves]] precede each regular, narrow [[QRS]] complex
| |
| *''[[PR interval]]'':
| |
| *''[[QRS complex]]'': Less than 0.12 seconds, consistent, and normal in morphology
| |
| *''Response to Maneuvers'': Although it cannot be distinguished on the surface 12 lead EKG from [[sinus tachycardia]], SA node reentry tachycardia does often terminate with [[vagal maneuvers]] unlike [[sinus tachycardia]].
| |
| *''Epidemiology and Demographics'':
| |
| | |
| ===[[Sinus tachycardia]]===
| |
| *''Rate'': Greater than 100.
| |
| *''Rhythm'': Regular.
| |
| *''[[P waves]]'': Upright, consistent, and normal in morphology (if no atrial disease)
| |
| *''[[PR interval]]'': Between 0.12–0.20 seconds and shortens with increasing heart rate
| |
| *''[[QRS complex]]'': Less than 0.12 seconds, consistent, and normal in morphology
| |
| *''Response to Maneuvers'':
| |
| *''Epidemiology and Demographics'':
| |
| | |
| ===[[Ventricular Tachycardia]]===
| |
| *''Rate'':
| |
| *''Rhythm'': Generally regular
| |
| *''[[P waves]]'': Normal morphology, upright, but dissociated from the QRS complex (i.e. "march through" the [[QRS complex]])
| |
| *''[[PR interval]]'':
| |
| *''[[QRS complex]]'': Wide and greater than 0.12 seconds
| |
| *''Response to Maneuvers'': Does not terminate in response to [[adenosine]] or [[vagal maneuvers]]
| |
| *''Epidemiology and Demographics'':
| |
| *''Risk Factors:'': Occurs in the context of [[myocardial ischemia]], [[myocardial infarction]], [[congestive heart failure]], drug toxicity, and inhereted [[channelopathies]]
| |
| | |
| ===[[Wolff-Parkinson-White syndrome]]===
| |
| *''Pathophysiology'': Anatomically and functionally, the fast and slow pathways of AVNRT should not be confused with the accessory pathways that give rise to [[Wolff-Parkinson-White syndrome]] ([[WPW]]) syndrome or [[AV reentrant tachycardia|atrioventricular re-entrant tachycardia]] ([[AVRT]]). In AVNRT, the fast and slow pathways are located within the [[right atrium]] in close proximity to or within the [[AV node]] and exhibit electrophysiologic properties similar to AV nodal tissue. Accessory pathways that give rise to [[WPW]] syndrome and [[AVRT]] are located in the atrioventricular valvular rings, they provide a direct connection between the atria and ventricles, and have electrophysiologic properties similar to ventricular [[myocardium]].
| |
| *''Rate'':
| |
| *''Rhythm'':
| |
| *''[[P waves]]'': In WPW with orthodromic conduction due to a bypass tract, the [[p wave]] generally follows the [[QRS]] complex, whereas in [[AVNRT]], the [[p wave]] is generally buried in the [[QRS]] complex.
| |
| *''[[PR interval]]'':
| |
| *''[[QRS complex]]'': In WPW there is a [[delta wave]] and evidence of ventricular preexcitation if there is conduction to the ventrilce via antegrade conduction down an accessory pathway. It should be noted, however, that in some patients with WPW, a delta wave and pre-excitation may not be present because bypass tracts do not conduct antegrade.
| |
| *''Response to Maneuvers'': May break in response to [[procainamide]], [[adenosine]], [[vagal maneuvers]]
| |
| *''Epidemiology and Demographics'':
| |
| *''Risk Factors'': None, an inhereted disorder
| |
| | |
| ==Epidemiology and Demographics==
| |
| AV nodal reentrant tachycardia is the most common regular supraventricular tachycardia and accounts for 60% to 70% of these cases.
| |
| | |
| ===Sex===
| |
| The ratio of female to male involvement is 3:1
| |
| | |
| ===Age===
| |
| There is no age predilection.
| |
| | |
| ==Natural History, Complications, Prognosis==
| |
| ===Natural History===
| |
| The rhythm often ceases abruptly and spontaneously. An episode generally last seconds to hours.
| |
| | |
| ===Complications===
| |
| *Some patients will develop [[syncope]] during episodes of AVRNT. The mechanism of syncope may be due to a reduction of [[cardiac output]] and [[hemodynamic compromise]] as a result of the short ventricular filling time or alternatively it may be due to transient [[asystole]] due to tachycardia-mediated suppression of the sinus node when the rhythm terminates. Those patients who do become symptomatic during episodes of AVNRT (i.e. have [[syncope]]) should avoid activities where the occurrence of [[hemodynamic compromise]] would endanger their safety or that of others (like driving).
| |
| *In patients with underlying [[ischemic heart disease]], demand-related [[myocardial ischemia]], [[angina]] and even [[myocardial infarction]] and/or [[congestive heart failure]] can occur.
| |
| *[[Tachycardia mediated cardiomyopathy]]
| |
| | |
| ===Prognosis===
| |
| AVNRT is rarely life threatening and in the absence of underlying structural heart disease, the prognosis is good. Radiofrequency ablation is curative in 95% of cases.
| |
|
| |
|
| ==Diagnosis== | | ==Diagnosis== |
| ===Symptoms===
| | [[AVNRT history and symptoms|Symptoms]] | [[AVNRT physical examination|Physical Examination]] | [[AVNRT laboratory findings|Laboratory Findings]] | [[AVNRT electrocardiogram|Electrocardiogram]] |
| The following symptoms may be present:
| |
| *Sudden onset and sudden offset of rapid [[palpitations]] is common
| |
| *[[Dizziness]] and rarely [[syncope]], especially at the onset of the episode of tachycardia
| |
| *Neck "pounding" may occur as a result of the [[right atrium]] contracting against a closed atrioventricular valve and [[Cannon a waves]]<ref name="pmid18775049">{{cite journal | author = Laurent G, Leong-Poi H, Mangat I, Korley V, Pinter A, Hu X, So PP, Ramadeen A, Dorian P | title = Influence of ventriculoatrial timing on hemodynamics and symptoms during supraventricular tachycardia | journal = [[Journal of Cardiovascular Electrophysiology]] | volume = 20 | issue = 2 | pages = 176–81 | year = 2009 | month = February | pmid = 18775049 | doi = 10.1111/j.1540-8167.2008.01276.x | url = http://onlinelibrary.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=1045-3873&date=2009&volume=20&issue=2&spage=176 | issn = | accessdate = 2012-09-05}}</ref><ref>Gursoy S, Steurer G, Brugada J, et al. Brief report: the hemodynamic mechanism of pounding in the neck in atrioventricular nodal reentrant tachycardia. N Engl J Med. Sep 10 1992;327(11):772-4.</ref> and the simultaneous occurrence of the atrial and ventricular contractions.
| |
| *[[Chest pain]] and [[angina]] if the patient has [[ischemic heart disease]]
| |
| *[[Dyspnea]]
| |
| *[[Polyuria]] can occur after the episode breaks. It has been hypothesized that this is due to the release of [[atrial natriuretic peptide]]
| |
| | |
| ===Physical Examination===
| |
| ====Pulse====
| |
| The heart rate is typically regular and between 140-280 bpm. In adults the range is 140-250 bpm, but in children the rate can exceed 250 bpm.
| |
| | |
| ====Systolic Blood Pressure====
| |
| *[[Hypotension]] may be present in some cases.
| |
| | |
| ====Neck====
| |
| *[[Cannon a waves]] may be present in some cases
| |
| | |
| ====Lungs====
| |
| *[[Rales]] may be present in some patients with [[congestive heart failure]]
| |
| | |
| ===Laboratory Studies===
| |
| Depending upon the patient's history and demographics, the following laboratory studies should be considered:
| |
| * [[Thyroid function tests]] ([[TFTs]]) - an [[hyperthyroidism|overactive thyroid]] may increase the risk of AVNRT
| |
| * [[Electrolyte]]s - [[hypokalemia]], [[hypomagnesemia]] may predispose to AVNRT
| |
| * [[Cardiac marker]]s - if there is a concern that [[myocardial infarction]] (a [[heart attack]]) has occurred either as a cause or as a result of the AVNRT; this is usually only the case if the patient has experienced ischemic [[chest pain]]
| |
| | |
| ===Electrocardiogram===
| |
| An [[electrocardiogram]] performed during the occurrence of symptoms may confirm the diagnosis of AVNRT.
| |
| | |
| ====Slow-Fast AVNRT (Common AVNRT)====
| |
| *This form of AVNRT accounts for 80% to 90% of cases of AVNRT.
| |
| *The [[retrograde P wave]] that is conducted retrograde up the fast pathway is usually burried within the QRS but less frequently may be observed at the end of the [[QRS complex]] as a pseudo r’ wave in lead V1 or an [[S wave]] in leads II, III or aVF.
| |
| | |
| ====Fast-Slow AVNRT (Uncommon AVNRT)====
| |
| [[File:Fast slow AVNRT.JPG]]
| |
| *This form of AVNRT Accounts for 10% of cases of AVNRT
| |
| *In this form of AVNRT, the impulse is first conducted antegrade down the Fast AV nodal pathway and is then conducted retrograde up the Slow AV nodal pathway.
| |
| *In contrast to Common AVNRT, a [[retrograde P wave]] may be observed after the [[QRS complex]] before the [[T wave]]
| |
| | |
| ====Slow-Slow AVNRT (Atypical AVNRT)====
| |
| * This form of AVNRT accounts for 1-5% of cases of AVNRT
| |
| * In this form of AVNRT, the impulse is first conducted antegrade down the Slow AV nodal pathway and retrograde up the Slow left atrial fibres approaching the AV node.
| |
| * The [[p wave]] may appear just before the [[QRS complex]], and this makes it hard to distinguish the rhythm from [[sinus tachycardia]].
| |
| | |
| ====Aberrant Conduction====
| |
| It is not uncommon for there to be a wide [[QRS complex]] due to aberrant conduction due to underlying conduction system disease. This can make it difficult to distinguish AVNRT from VT. The distinguishing features include:
| |
| *AVNRT is associated with a [[QRS complex]] morphology resembles a typical [[bundle branch block]]
| |
| *AVNRT is not associated with [[AV dissociation]] where there is variable coupling of the [[p wave]] and the [[QRS complex]]
| |
| *AVNRT is associated with [[Cannon a waves]]
| |
| *AVNRT is not associated with [[capture beats]] or [[fusion beats]]
| |
| *AVNRT may convert with [[adenosine]] or [[vagal maneuvers]]
| |
| | |
| An electrophysiologic study may be needed to confirm AVNRT prior to ablation.
| |
| | |
| ===Holter Monitor / Event Recorder===
| |
| If the patient complains of recurrent [[palpitations]] and no arrhythmia is present on the resting EKG, then a [[Holter Monitor]] or [[Cardiac Event Monitor]] should be considered.
| |
|
| |
|
| ==Treatment== | | ==Treatment== |
| An episode of [[supraventricular tachycardia]] (SVT) due to AVNRT can be terminated by any action that transiently blocks the [[AV node]]. Various methods are possible.
| | [[AVNRT treatment overview|Overview]] | [[AVNRT patient position|Patient Position]] | [[AVNRT vagal maneuvers|Vagal Maneuvers]] | [[AVNRT medical therapy|Medical Therapy]] | [[AVNRT cardioversion|Cardioversion]] | [[AVNRT electrophysiologic testing and radiofrequency ablation|Electrophysiologic Testing and Radiofrequency Ablation]] | [[AVNRT prevention|Prevention]] |
| | |
| ===Patient Position===
| |
| Place the patient in a supine position to improve cerebral perfusion and reduce the odds of [[syncope]]. Placing the patient in [[Trendelenburg position]] may actually terminate the rhythm.
| |
| | |
| ===Vagal maneuvers===
| |
| Some people with known AVNRT may be able to stop their attack by using various tricks to activate the [[vagus nerve]]. This includes [[carotid sinus massage]] (pressure on the [[carotid sinus]] in the neck), submersion of the face in ice water to trigger the [[diving reflex]], putting the patient in [[Trendelenburg position]] or the [[Valsalva maneuver]] (increasing the pressure in the chest by attempting to exhale against a closed airway). [[Vagel maneuvers]] are contraindicated in the presence of [[hypotension]].
| |
| | |
| ===Medication===
| |
| Medical therapy can be initiated with AV nodal slowing drugs: | |
| | |
| ====First Line Therapy====
| |
| =====[[Adenosine]]=====
| |
| | |
| =====[[Beta blocker]]s=====
| |
| | |
| ====Second Line Therapy====
| |
| Numerous other antiarrhythmic drugs may be effective if the more commonly used medications have not worked; these include [[flecainide]] or [[amiodarone]]. Both adenosine and beta blockers may cause [[Bronchoconstriction|tightening of the airways]], and are therefore used with caution in people who are known to have [[asthma]]. Calcium channel blockers should be avoided if there is a [[wide complex tacycardia]] and the diagnosis of AVNRT is not clearly established in so far as [[calcium channel blockers]] should be avoided in [[ventricular tachycardia]]. If the diagnosis of AVNRT is established, then non-dihydropyridine [[calcium channel blocker]]s (such as [[verapamil]]) may be administered to terminate the rhythm is other agents are not effective.
| |
| | |
| ===Cardioversion===
| |
| In very rare instances, [[cardioversion]] (the electrical restoration of a normal heart rhythm) is needed in the treatment of AVNRT. This would normally only happen if all other treatments have been ineffective, or if the fast heart rate is poorly tolerated (e.g. the development of [[heart failure]] symptoms, [[hypotension]] ([[low blood pressure]]) or [[unconsciousness]]).
| |
| | |
| ===Electrophysiology and Radiofrequency Ablation===
| |
| After being diagnosed with AVNRT, patients can also undergo an electrophysiology (EP) study to confirm the diagnosis. [[Catheter ablation]] of the slow pathway, if successfully carried out, and cures 95% of patients with AVNRT. The risk of complications is quite low.
| |
| | |
| ===Prevention===
| |
| Triggers such as [[alcohol]] and caffeine should be avoided.
| |
| | |
| ==References==
| |
| {{Reflist|2}}
| |
| | |
| ==See also==
| |
| *[[AV Reentrant tachycardia]]
| |
| *[[Supraventricular tachycardia]]
| |
| *[[Cardiac electrophysiology]]
| |
| *[[Clinical cardiac electrophysiology]]
| |
|
| |
|
| {{WikiDoc Help Menu}} | | {{WikiDoc Help Menu}} |
| {{WikiDoc Sources}} | | {{WikiDoc Sources}} |
| | [[CME Category::Cardiology]] |
|
| |
|
| [[Category:Electrophysiology]] | | [[Category:Electrophysiology]] |
| [[Category:Cardiology]] | | [[Category:Cardiology]] |
| | [[Category:Arrhythmia]] |
| [[Category:Emergency medicine]] | | [[Category:Emergency medicine]] |
| | [[Category:Intensive care medicine]] |