Sotalol
{{DrugProjectFormSinglePage |authorTag=Alonso Alvarado, M.D. [1] |genericName=Sotalol |aOrAn=a |drugClass=Template:Beta-adrenergic blocker, Template:Antiarrhythmic |indication=ventricular arrhythmias, symptomatic atrial fibtillation, symptomatic atriall flutter |hasBlackBoxWarning=Yes |adverseReactions=bradyarrhythmia, chest pain, lightheadedness, palpitations, rash, nausea, dizziness, headache, dyspnea, fatigue |blackBoxWarningTitle=WARNING |blackBoxWarningBody=INDUCED ARRHYTHMIA: To minimize the risk of induced arrhythmia, patients initiated or re-initiated on sotalol hydrochloride tablets (AF) should be placed for a minimum of three days (on their maintenance dose) in a facility that can provide cardiac resuscitation, continuous electrocardiographic monitoring and calculations of creatinine clearance. For detailed instructions regarding dose selection and special cautions for people with renal impairment. Sotalol is also indicated for the treatment of documented life-threatening ventricular arrhythmias and is marketed under the brand name Betapace (sotalol hydrochloride). Sotalol hydrochloride tablets, however, must not be substituted for Betapace AF (sotalol hydrochloride tablets, USP (AF)) because of significant differences in labeling (i.e. patient package insert, dosing administration and safety information). |fdaLIADAdult======Condition 1=====
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
|offLabelAdultGuideSupport======Condition 1=====
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Condition 2
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
|offLabelAdultNoGuideSupport======Condition 1=====
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Condition 3
- Dosing Information
- (Dosage)
|fdaLIADPed======Condition 1=====
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
|offLabelPedGuideSupport======Condition 1=====
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Condition 2
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
|offLabelPedNoGuideSupport======Condition 1=====
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Condition 3
- Dosing Information
- (Dosage)
|contraindications=* Bronchial asthma.
- Sinus bradycardia.
- Second degree AV block and third degree AV block, unless a functioning pacemaker is present.
- Congenital or acquired long QT syndromes.
- Cardiogenic shock.
- Uncontrolled congestive heart failure.
- Hypersensitivity to Betapace.
|warnings======Conidition 1=====
(Description) |clinicalTrials=======Central Nervous System======
- (list/description of adverse reactions)
Cardiovascular
- (list/description of adverse reactions)
Respiratory
- (list/description of adverse reactions)
Gastrointestinal
- (list/description of adverse reactions)
Hypersensitive Reactions
- (list/description of adverse reactions)
Miscellaneous
- (list/description of adverse reactions)
Condition 2
Central Nervous System
- (list/description of adverse reactions)
Cardiovascular
- (list/description of adverse reactions)
Respiratory
- (list/description of adverse reactions)
Gastrointestinal
- (list/description of adverse reactions)
Hypersensitive Reactions
- (list/description of adverse reactions)
Miscellaneous
- (list/description of adverse reactions)
|postmarketing=(Description) |drugInteractions=* Drug 1
- Drug 2
- Drug 3
- Drug 4
- Drug 5
Drug 1
(Description)
Drug 2
(Description)
Drug 3
(Description)
Drug 4
(Description)
Drug 5
(Description) |useInPregnancyFDA=(Description) |useInPregnancyAUS=(Description) |useInLaborDelivery=(Description) |useInNursing=(Description) |useInPed=(Description) |useInGeri=(Description) |useInGender=(Description) |useInRace=(Description) |useInRenalImpair=(Description) |useInHepaticImpair=(Description) |useInReproPotential=(Description) |useInImmunocomp=(Description) |othersTitle=Others |useInOthers=(Description) |administration=(Oral/Intravenous/etc) |monitoring======Condition 1=====
(Description regarding monitoring, from Warnings section)
Condition 2
(Description regarding monitoring, from Warnings section)
Condition 3
(Description regarding monitoring, from Warnings section) |IVCompat====Solution===
Compatible
- Solution 1
- Solution 2
- Solution 3
Not Tested
- Solution 1
- Solution 2
- Solution 3
Variable
- Solution 1
- Solution 2
- Solution 3
Incompatible
- Solution 1
- Solution 2
- Solution 3
Y-Site
Compatible
- Solution 1
- Solution 2
- Solution 3
Not Tested
- Solution 1
- Solution 2
- Solution 3
Variable
- Solution 1
- Solution 2
- Solution 3
Incompatible
- Solution 1
- Solution 2
- Solution 3
Admixture
Compatible
- Solution 1
- Solution 2
- Solution 3
Not Tested
- Solution 1
- Solution 2
- Solution 3
Variable
- Solution 1
- Solution 2
- Solution 3
Incompatible
- Solution 1
- Solution 2
- Solution 3
Syringe
Compatible
- Solution 1
- Solution 2
- Solution 3
Not Tested
- Solution 1
- Solution 2
- Solution 3
Variable
- Solution 1
- Solution 2
- Solution 3
Incompatible
- Solution 1
- Solution 2
- Solution 3
TPN/TNA
Compatible
- Solution 1
- Solution 2
- Solution 3
Not Tested
- Solution 1
- Solution 2
- Solution 3
Variable
- Solution 1
- Solution 2
- Solution 3
Incompatible
- Solution 1
- Solution 2
- Solution 3
|overdose====Acute Overdose===
Signs and Symptoms
(Description)
Management
(Description)
Chronic Overdose
Signs and Symptoms
(Description)
Management
(Description) |drugBox={{Drugbox2 | verifiedrevid = 420038718 | IUPAC_name = (RS)-N-{4-[1-hydroxy-2-(propan-2-ylamino)ethyl]phenyl}methanesulfonamide | image = SotalolStructure.png | imagename = 1 : 1 mixture (racemate) | drug_name = Sotalol
| tradename = Betapace | Drugs.com = Monograph | MedlinePlus = a693010 | pregnancy_AU = | pregnancy_US = B | pregnancy_category = | legal_status = Rx-only | routes_of_administration = oral
| bioavailability = >95%
| metabolism = Not metabolized[citation needed]
| elimination_half-life = 12 hours
| excretion = Renal
Lactic (In lactating females)
| CASNo_Ref =
| CAS_number_Ref =
| CAS_number = 3930-20-9
| ATC_prefix = C07
| ATC_suffix = AA07
| PubChem = 5253
| DrugBank_Ref =
| DrugBank = DB00489
| ChemSpiderID_Ref =
| ChemSpiderID = 5063
| UNII_Ref =
| UNII = A6D97U294I
| KEGG_Ref =
| KEGG = D08525
| ChEMBL_Ref =
| ChEMBL = 471
| C=12 | H=20 | N=2 | O=3 | S=1
| molecular_weight = 272.3624 g/mol
| smiles = O=S(=O)(Nc1ccc(cc1)C(O)CNC(C)C)C
| InChI = 1/C12H20N2O3S/c1-9(2)13-8-12(15)10-4-6-11(7-5-10)14-18(3,16)17/h4-7,9,12-15H,8H2,1-3H3
| InChIKey = ZBMZVLHSJCTVON-UHFFFAOYAR
| StdInChI_Ref =
| StdInChI = 1S/C12H20N2O3S/c1-9(2)13-8-12(15)10-4-6-11(7-5-10)14-18(3,16)17/h4-7,9,12-15H,8H2,1-3H3
| StdInChIKey_Ref =
| StdInChIKey = ZBMZVLHSJCTVON-UHFFFAOYSA-N
}}
|mechAction=Sotalol hydrochloride has both beta-blocker (Vaughan Williams Class II) and cardiac action potential duration prolongation (Vaughan Williams Class III) antiarrhythmic properties. Sotalol hydrochloride is a racemic mixture of d- and l-sotalol. Both isomers have similar Class III antiarrhythmic effects, while the l-isomer is responsible for virtually all of the beta-blocking activity. The beta-blocking effect of sotalol is non-cardioselective, half maximal at about 80 mg/day and maximal at doses between 320 and 640 mg/day. Sotalol does not have partial agonist or membrane stabilizing activity. Although significant beta-blockade occurs at oral doses as low as 25 mg, significant Class III effects are seen only at daily doses of 160 mg and above.
In children, a Class III electrophysiologic effect can be seen at daily doses of 210 mg/m2 body surface area (BSA). A reduction of the resting heart rate due to the beta-blocking effect of sotalol is observed at daily doses ≥ 90 mg/m2 in children. |structure=Sotalol hydrochloride is an antiarrhythmic drug with Class II (beta-blocker) and Class III (cardiac action potential duration prolongation) properties. It is supplied as a light-blue, capsule-shaped tablet for oral administration. Sotalol hydrochloride is a white, crystalline solid with a molecular weight of 308.8. It is hydrophilic, soluble in water, propylene glycol and ethanol, but is only slightly soluble in chloroform. Chemically, sotalol hydrochloride is d,l-N -[4-[1-hydroxy-2-[(1-methylethyl) amino]ethyl]phenyl]methane-sulfonamide monohydrochloride. The molecular formula is C12H20N2O3 S·HCl and is represented by the following structural formula:

Satolol tablets contain the following inactive ingredients: microcrystalline cellulose, lactose, starch, stearic acid, magnesium stearate, colloidal silicon dioxide, and FD&C blue color #2 (aluminum lake, conc.). |PD=Sotalol hydrochloride prolongs the plateau phase of the cardiac action potential in the isolated myocyte, as well as in isolated tissue preparations of ventricular or atrial muscle (Class III activity). In intact animals it slows heart rate, decreases AV nodal conduction and increases the refractory periods of atrial and ventricular muscle and conduction tissue.
In man, the Class II (beta-blockade) electrophysiological effects of sotalol are manifested by increased sinus cycle length (slowed heart rate]), decreased AV nodal conduction and increased AV nodal refractoriness. The Class III electrophysiological effects in man include prolongation of the atrial and ventricular monophasic action potentials, and effective refractory period prolongation of atrial muscle, ventricular muscle, and atrio-ventricular accessory pathways (where present) in both the anterograde and retrograde directions. With oral doses of 160 to 640 mg/day, the surface ECG shows dose-related mean increases of 40-100 msec in QT and 10-40 msec in QTc. No significant alteration in QRS interval is observed.
In a small study (n=25) of patients with implanted defibrillators treated concurrently with sotalol, the average defibrillatory threshold was 6 joules (range 2-15 joules) compared to a mean of 16 joules for a nonrandomized comparative group primarily receiving amiodarone.
Twenty-five children in an unblinded, multicenter trial with supraventricular tachycardias (SVT) and/or ventricular tachyarrhythmias (VT), aged between 3 days and 12 years (mostly neonates and infants), received an ascending titration regimen with daily doses of 30, 90 and 210 mg/m2 with dosing every 8 hours for a total 9 doses. During steady-state, the respective average increases above baseline of the QTc interval, in msec (%), were 2(+1%), 14(+4%) and 29(+7%) msec at the 3 dose levels. The respective mean maximum increases above baseline of the QTc interval, in msec (%), were 23(+6%), 36(+9%) and 55(+14%) msec at the 3 dose levels. The steadystate percent increases in the RR interval were 3, 9 and 12%. The smallest children (BSA<0.33m2) showed a tendency for larger Class III effects (ΔQTc) and an increased frequency of prolongations of the QTc interval as compared with larger children (BSA≥0.33m2). The beta-blocking effects also tended to be greater in the smaller children (BSA<0.33m2). Both the Class III and beta-blocking effects of sotalol were linearly related with the plasma concentrations. |PK=In healthy subjects, the oral bioavailability of sotalol hydrochloride is 90-100%. After oral administration, peak plasma concentrations are reached in 2.5 to 4 hours, and steady-state plasma concentrations are attained within 2-3 days (i.e., after 5-6 doses when administered twice daily). Over the dosage range 160-640 mg/day sotalol hydrochloride displays dose proportionality with respect to plasma concentrations. Distribution occurs to a central (plasma) and to a peripheral compartment, with a mean elimination half-life of 12 hours. Dosing every 12 hours results in trough plasma concentrations which are approximately one-half of those at peak.
Sotalol hydrochloride does not bind to plasma proteins and is not metabolized. Sotalol hydrochloride shows very little intersubject variability in plasma levels. The pharmacokinetics of the d and l enantiomers of sotalol are essentially identical. Sotalol hydrochloride crosses the blood brain barrier poorly. Excretion is predominantly via the kidney in the unchanged form, and therefore lower doses are necessary in conditions of renal impairment. Age per se does not significantly alter the pharmacokinetics of sotalol, but impaired renal function in geriatric patients can increase the terminal elimination half-life, resulting in increased drug accumulation. The absorption of sotalol hydrochloride was reduced by approximately 20% compared to fasting when it was administered with a standard meal. Since sotalol hydrochloride is not subject to first-pass metabolism, patients with hepatic impairment show no alteration in clearance of sotalol.
The combined analysis of two unblinded, multicenter trials (a single dose and a multiple dose study) with 59 children, aged between 3 days and 12 years, showed the pharmacokinetics of sotalol to be first order. A daily dose of 30 mg/m2 of sotalol was administered in the single dose study and daily doses of 30, 90 and 210 mg/m2 were administered q 8h in the multi-dose study. After rapid absorption with peak levels occurring on average between 2-3 hours following administration, sotalol was eliminated with a mean half life of 9.5 hours. Steady-state was reached after 1-2 days. The average peak to trough concentration ratio was 2. BSA was the most important covariate and more relevant than age for the pharmacokinetics of sotalol.The smallest children (BSA<0.33m2) exhibited a greater drug exposure (+59%) than the larger children who showed a uniform drug concentration profile. The intersubject variation for oral clearance was 22%. |nonClinToxic=No evidence of carcinogenic potential was observed in rats during a 24-month study at 137-275 mg/kg/day (approximately 30 times the maximum recommended human oral dose (MRHD) as mg/kg or 5 times the MRHD as mg/m2) or in mice, during a 24-month study at 4141-7122 mg/kg/ day (approximately 450-750 times the MRHD as mg/kg or 36-63 times the MRHD as mg/m2).
Sotalol has not been evaluated in any specific assay of mutagenicity or clastogenicity. No significant reduction in fertility occurred in rats at oral doses of 1000 mg/kg/ day (approximately 100 times the MRHD as mg/kg or 9 times the MRHD as mg/m2) prior to mating, except for a small reduction in the number of offspring per litter. |clinicalStudies======Prolongation of Time to Recurrence of Symptomatic Atrial Fibrillation/ Flutter=====
Sotalol hydrochloride (AF) has been studied in patients with symptomatic AFIB/AFL in two principal studies, one in patients with primarily paroxysmal AFIB/AFL, the other in patients with primarily chronic AFIB.
In one study, a U.S. multicenter, randomized, placebo-controlled, double-blind, dose-response trial of patients with symptomatic primarily paroxysmal AFIB/AFL, three fixed dose levels of sotalol hydrochloride (AF) (80 mg, 120 mg and 160 mg) twice daily and placebo were compared in 253 patients. In patients with reduced creatinine clearance (40-60 mL/min) the same doses were given once daily. Patients were not randomized for the following reasons: QT >450 msec; creatinine clearance <40 mL/min; intolerance to beta-blockers; bradycardia-tachycardia syndrome in the absence of an implanted pacemaker; AFIB/AFL was asymptomatic or was associated with syncope, embolic CVA or TIA; acute myocardial infarction within the previous 2 months; congestive heart failure; bronchial asthma or other contraindications to beta-blocker therapy; receiving potassium losing diuretics without potassium replacement or without concurrent use of ACE-inhibitors; uncorrected hypokalemia (serum potassium <3.5 meq/L) or hypomagnesemia (serum magnesium <1.5 meq/L); received chronic oral amiodarone therapy for >1 month within previous 12 weeks; congenital or acquired long QT syndromes; history of Torsade de Pointes with other antiarrhythmic agents which increase the duration of ventricular repolarization; sinus rate <50 bpm during waking hours; unstable angina pectoris; receiving treatment with other drugs that prolong the QT interval; and AFIB/AFL associated with the Wolff-Parkinson-White syndrome (WPW). If the QT interval increased to ≥520 msec (or JT ≥430 msec if QRS >100 msec) the drug was discontinued. The patient population in this trial was 64% male, and the mean age was 62 years. No structural heart disease was present in 43% of the patients. Doses were administered once daily in 20% of the patients because of reduced creatinine clearance.
Sotalol hydrochloride (AF) was shown to prolong the time to the first symptomatic, ECG documented recurrence of AFIB/AFL, as well as to reduce the risk of such recurrence at both 6 and 12 months. The 120 mg dose was more effective than 80 mg, but 160 mg did not appear to have an added benefit. Note that these doses were given twice or once daily, depending on renal function. The results are shown in the figure and tables below.

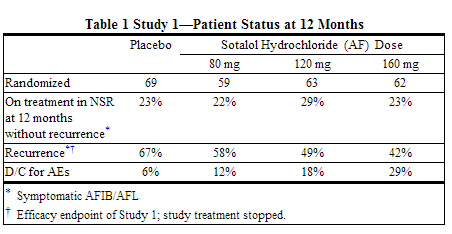
Please note that columns do not add up to 100% due to discontinuations (D/C) for "other" reasons.

Discontinuation because of adverse events was dose related.
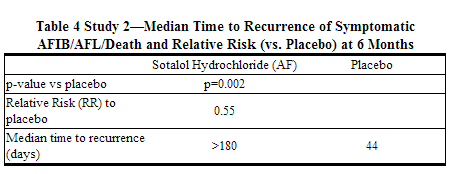
In a second multicenter, randomized, placebo-controlled, double-blind study of 6 months duration in 232 patients with chronic AFIB, sotalol hydrochloride (AF) was titrated over a dose range from 80 mg/day to 320 mg/day. The patient population of this trial was 70% male with a mean age of 65 years. Structural heart disease was present in 49% of the patients. All patients had chronic AFIB for >2 weeks but <1 year at entry with a mean duration of 4.1 months. Patients were excluded if they had significant electrolyte imbalance, QTc >460 msec, QRS >140 msec, any degree of AV block or functioning pacemaker, uncompensated cardiac failure, asthma, significant renal disease (estimated creatinine clearance <50 mL/min), heart rate <50 bpm, myocardial infarction or open heart surgery in past 2 months, unstable angina, infective endocarditis, active pericarditis or myocarditis, ≥ 3 DC cardioversions in the past, medications that prolonged QT interval, and previous amiodarone treatment. After successful cardioversion patients were randomized to receive placebo (n=114) or sotalol hydrochloride (AF) (n=118), at a starting dose of 80 mg twice daily. If the initial dose was not tolerated it was decreased to 80 mg once daily, but if it was tolerated it was increased to 160 mg twice daily. During the maintenance period 67% of treated patients received a dose of 160 mg twice daily, and the remainder received doses of 80 mg once daily (17%) and 80 mg twice daily (16%).
The figure and Tables below show the results of the trial. There was a longer time to ECG-documented recurrence of AFIB and a reduced risk of recurrence at 6 months compared to placebo.


Safety in Patients with Structural Heart Disease
In a multicenter double-blind randomized study reported by D. Julian et al, the effect of sotalol 320 mg once daily was compared with that of placebo in 1456 patients (randomized 3:2, sotalol to placebo) surviving an acute myocardial infarction (MI). Treatment was started 5 to 14 days after infarction. Patients were followed for 12 months. The mortality rate was 7.3% in the sotalol group and 8.9% in the placebo group, not a statistically significant difference. Although the results do not show evidence of a benefit of sotalol in this population, they do not show an added risk in post MI patients receiving sotalol.
|howSupplied=(Description) |fdaPatientInfo=(Patient Counseling Information) |alcohol=Alcohol-Sotalol interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. |lookAlike=* (Paired Confused Name 1a) — (Paired Confused Name 1b)
- (Paired Confused Name 2a) — (Paired Confused Name 2b)
- (Paired Confused Name 3a) — (Paired Confused Name 3b)
|nlmPatientInfo=(Link to patient information page) |drugShortage=Drug Shortage }}