Ventricular tachycardia electrocardiogram
|
Ventricular tachycardia Microchapters |
|
Differentiating Ventricular Tachycardia from other Disorders |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Ventricular tachycardia electrocardiogram On the Web |
|
to Hospitals Treating Ventricular tachycardia electrocardiogram |
|
Risk calculators and risk factors for Ventricular tachycardia electrocardiogram |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-in Chief: Avirup Guha, M.B.B.S.[2]; Priyamvada Singh, M.D. [3]
Overview
The diagnosis of ventricular tachycardia almost completely depends on EKG findings. The details are illustrated below. It is important to differentiate it from other wide complex tachycardias. The rate is > 100 beats per minute, and is usually 150-200 beats per minute. The QRS complex is wide (>140 milliseconds). AV dissociation is always present, but is evident in only 20% of cases of VT.
Electrocardiogram
Brugada Criteria
- The Brugada criteria is the commonest algorithm used to diagnose ventricular tachycardia.
- In Brugada's algorithm four criteria for VT are sequentially assessed.
- If any one of the four criteria are fulfilled diagnosis of VT is made.
- If none of the criteria are fulfilled a diagnosis of SVT is made.
- The four criteria are as follow:
- Check for concordance in the precordial leads. Concordance is said to be present when the QRS complexes in all the leads V1 to V6 are monophasic (all positive or all negative) with the same polarity. If any of the precordial leads has a biphasic QRS concordance is absent.
- If the longest RS interval in any lead is >100 msec and R wave is wider than S wave a diagnosis of VT can be made.
- If longest RS interval is less than 100 msec, presence of AV dissociation can lead to a diagnosis of VT.
- If longest RS interval is less than 100 msec, and AV dissociation is not present then the QRS morphology is used to make the diagnosis. QRS morphology criteria consistent with VT must be present in leads V1 or V2 and in lead V6. A VT with RBBB morphology is here when the QRS polarity in lead V1 and V2 are poisitive whereas, a LBBB pattern occurs with a negative QRS polarity. If either the V1-V2 or the V6 criteria are not consistent with VT, an diagnosis of SVT is made.
Diagnostic Electrocardiographic Findings
- Abnormal and wide QRS complexes with secondary ST segment and T wave changes.
- Usual QRS duration is > 0.12 seconds, may be shorter if the ectopic focus is located in the ventricular septum.
- The secondary ST segment and T wave changes are in a direction that is opposite the major deflection of the QRS.
- A ventricular rate between 140 and 200 BPM.
- When the rate is >200 and has a sine wave appearance, it is called ventricular flutter.
- When the rate is <110 BPM it is called non-paroxysmal VT.
- A regular or slightly irregular (up to 0.03 seconds) rhythm.
- Abrupt onset and termination.
- AV dissociation
- Atrial rate slower than ventricular rate.
- No relationship between atrial activity and ventricular activity.
- There can be VA conduction.
- The RP interval is >0.11 seconds.
- Occurs in about 50% of cases.
- Uncommon when the ventricular rate is rapid (only 1/7 when the rate was>200).
- Axis
- Northwest quadrant is almost always VT in adults.
- In someone with a normal QRS in sinus rhythm, a LBBB-like wide complex tachycardia with a right axis (+90 to +180) is always VT because activation in LBBB aberration always goes from right to left.
- Concordance
- If all the precordial leads are positive (R) or negative (QS) the rhythm is very likely VT
- V1-V2 morphology
- RBBB morphology
- RsR' or rsR' in V1 favors SVT, whereas a monophasic R, Rr', qR, or RS favors VT.
- RBBB aberration the initial forces of the QRS are the same as in the narrow complex sinus rhythm.
- LBBB morphology
- V1 and V2 require analysis because the initial forces in V1 are often isoelectric.
- R wave in V1 or V2 ≥40 msec favors VT.
- The time from the onset of the QRS to the nadir of the S wave in V1 or V2 is ≥70 msec, VT is likely in the absence of Na channel blocking agents.
- RBBB morphology
- V6 morphology
- RBBB morphology - QS or rS favors VT. Although this can be influenced by axis (it is almost always seen in VT with left axis deviation, but is seen in only approximately 50% of VT with a normal axis, even in the same patient).
- LBBB morphology - a qR or QS is highly predictive of VT
- Capture beats.
- Occurs when a supraventricular impulse is conducted and captures the ventricle.
- They are rare.
- Fusion beats.
Ventricular Tachycardia
- Ventricular tachycardia originates from a ventricular focus
- Lasts more than 30 seconds
- Broad QRS complexes: rate of >90 beats/minute
Paroxysmal Ventricular Tachycardia
- Rapid succession of three or more ectopic beats.
- Sustained if it lasts longer than 30 seconds.
- Called incessant if the tachycardia is recurrent and the episodes are interrupted by only a few sinus beats.
EKG Examples
Shown below is an EKG with a rapid ventricular rate of about 170/min with wide QRS complexes in lead II depicting ventricular tachycardia.
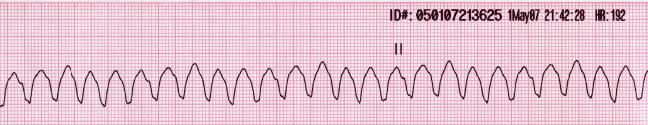
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an EKG depicting a wide complex tachycardia with a left bundle branch morphology at a rate of about 160/min. The R wave in lead V2 is broad, and the time from the beginning of the QRS in lead V2 to the peak of the S wave is longer than 80 ms. No P wave activity is clearly seen. This EKG suggests ventricular tachycardia.
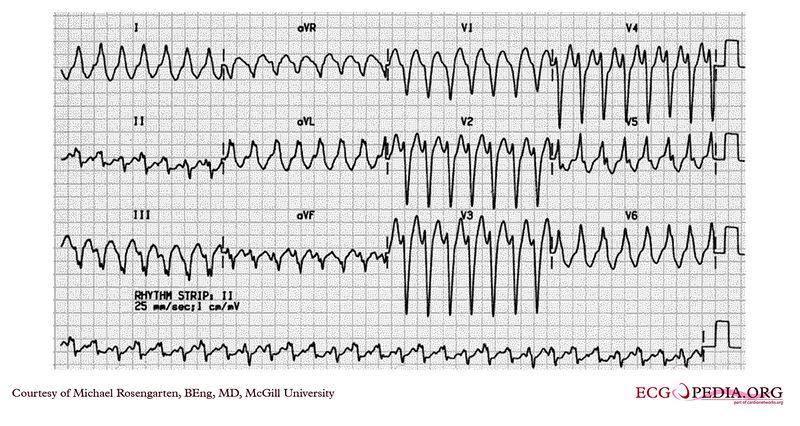
Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/File:E334.jpg
Shown below is an EKG with a rapid ventricular rate of nearly 190 beats per minute with wide QRS complexes depicting ventricular tachycardia.
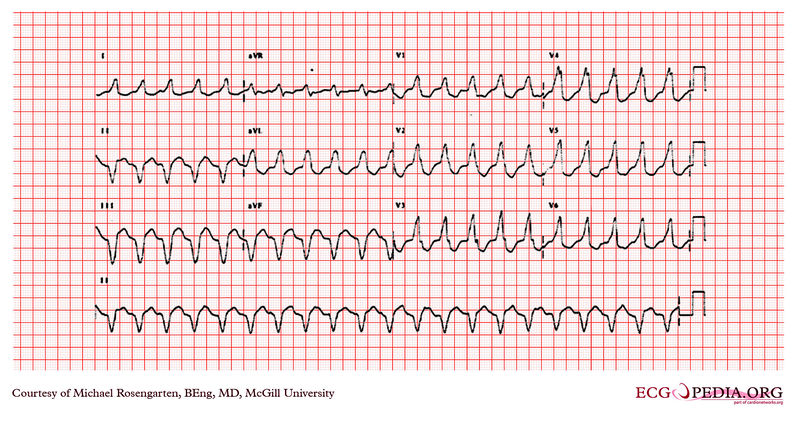
Copyleft image obtained courtesy of ECGpedia,http://en.ecgpedia.org/wiki/File:E253.jpg
Shown below is an EKG with a rapid ventricular rate of about 190/min with wide QRS complex in all leads depicting ventricular tachycardia.
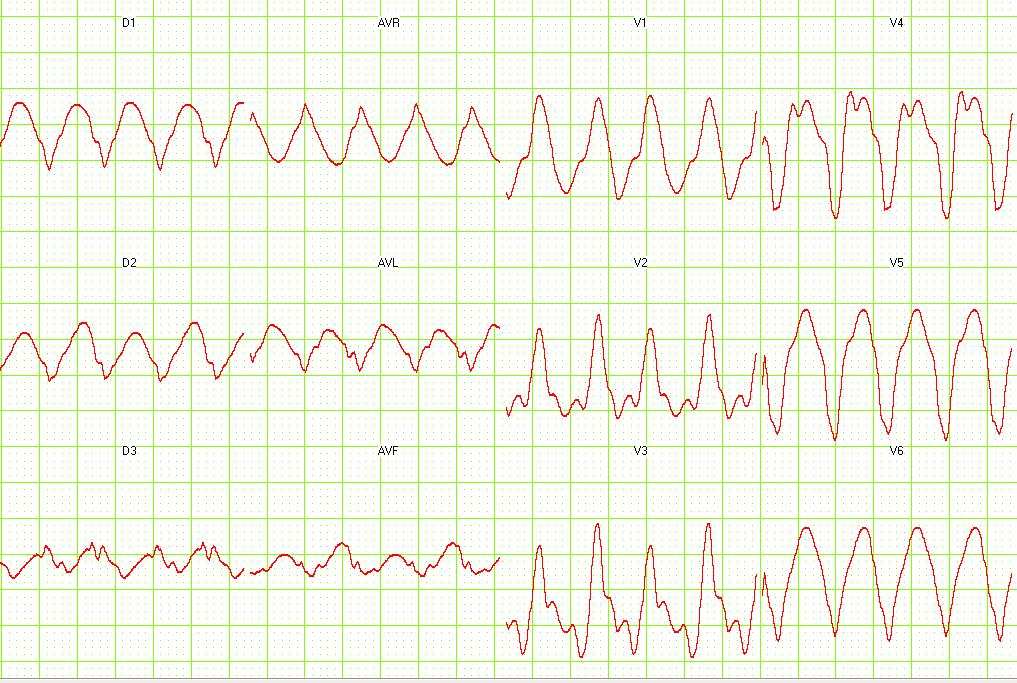
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
For more EKG examples of ventricular tachycardia, click here.
References
- ↑ Chou's Electrocardiography in Clinical Practice Third Edition, pp. 398-409.
- ↑ Sailer, Christian, Wasner, Susanne. Differential Diagnosis Pocket. Hermosa Beach, CA: Borm Bruckmeir Publishing LLC, 2002:194 ISBN 1591032016
- ↑ Hammill S. C. Electrocardiographic diagnoses: Criteria and definitions of abnormalities, Chapter 18, MAYO Clinic, Concise Textbook of Cardiology, 3rd edition, 2007 ISBN 0-8493-9057-5