Carotid artery stenosis echocardiography or ultrasound
|
Carotid artery stenosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
ACC/AHA Guideline Recommendations |
|
Periprocedural Management of Patients Undergoing Carotid Endarterectomy |
|
Atherosclerotic Risk Factors in Patients With Vertebral Artery Disease |
|
Occlusive Disease of the Subclavian and Brachiocephalic Arteries |
|
Case Studies |
|
Carotid artery stenosis echocardiography or ultrasound On the Web |
|
American Roentgen Ray Society Images of Carotid artery stenosis echocardiography or ultrasound |
|
FDA on Carotid artery stenosis echocardiography or ultrasound |
|
CDC on Carotid artery stenosis echocardiography or ultrasound |
|
Carotid artery stenosis echocardiography or ultrasound in the news |
|
Blogs on Carotid artery stenosis echocardiography or ultrasound |
|
Risk calculators and risk factors for Carotid artery stenosis echocardiography or ultrasound |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
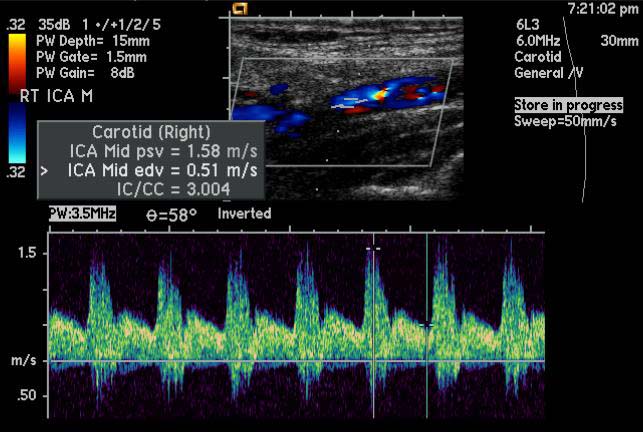
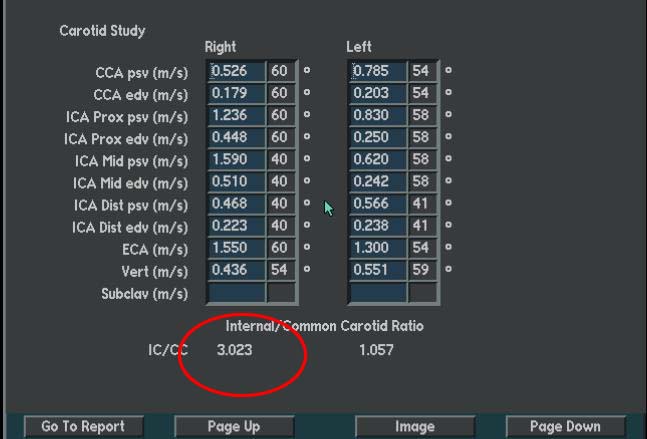
Carotid stenosis is usually diagnosed by ultrasound scan of the neck arteries. This is the first imaging option and usually used for follow up and observation as it involves no radiation and no contrast agents that may cause allergic reactions.
Carotid duplex ultrasound
- Carotid duplex ultrasound is the test of choice to evaluate carotid disease.
- Grading:
- Mild - < 40% stenosis
- Moderate - 40 - 69% stenosis
- Severe - 70 - 99% stenosis
Ultrasound Criteria for Carotid Artery Stenosis
- Normal:
- ICA PSV is less than 125 cm/sec and no plaque or intimal thickening is visible sonographically.
- Additional criteria include ICA/CCA PSV ratio < 2.0 and ICA EDV < 40 cm/sec.
- <50% ICA stenosis:
- ICA PSV is less than 125 cm/sec and plaque or intimal thickening is visible sonographically.
- Additional criteria include ICA/CCA PSV ratio < 2.0 and ICA EDV < 40 cm/sec.
- 50%–69% ICA stenosis:
- ICA PSV is 125–230 cm/sec and plaque is visible sonographically.
- Additional criteria include ICA/CCA PSV ratio of 2.0–4.0 and ICA EDV of 40–100 cm/sec.
- >=70% ICA stenosis but less than near occlusion
- ICA PSV is greater than 230 cm/sec and visible plaque and luminal narrowing are seen at gray-scale and color Doppler US (The higher the Doppler parameter lies above the threshold of 230 cm/sec, the greater the likelihood of severe disease).
- Additional criteria include ICA/CCA PSV ratio > 4 and ICA EDV > 100 cm/sec.
- Vear occlusion of the ICA:
- Velocity parameters may not apply, since velocities may be high, low, or undetectable.
- Diagnosis is established primarily by demonstrating a markedly narrowed lumen at color or power Doppler US (35).
- Total occlusion of the ICA
- No detectable patent lumen at gray-scale US and no flow with spectral, power, and color Doppler US. [1]
Guideline on the Management of Patients With Extracranial Carotid and Vertebral Artery Disease: Duplex Ultrasonography to Evaluate Asymptomatic Patients With Known or Suspected Carotid Stenosis[2] (DO NOT EDIT)
| Class I |
| "1. In asymptomatic patients with known or suspected carotid stenosis, duplex ultrasonography, performed by a qualified technologist in a certified laboratory, is recommended as the initial test to detect hemodynamically significant carotid stenosis. (Level of Evidence: C) " |
| Class III |
| " Carotid duplex ultrasonography is not recommended " |
| "1. For routine screening of asymptomatic patients who have no risk factors for atherosclerosis. (Level of Evidence: C) " |
| "2. For routine evaluation of patients with neurological or psychiatric disorders unrelated to focal cerebral ischemia. (Level of Evidence: C) " |
| "3. For patients without risk factors for atherosclerotic carotid disease and no disease on initial vascular testing. (Level of Evidence: C) " |
| Class IIa |
| " It is reasonable to" |
| "1. Perform duplex ultrasonography to detect hemodynamically significant carotid stenosis in asymptomatic patients with carotid bruit. (Level of Evidence: C)" |
| "1. Repeat duplex ultrasonography annually, by a qualified technologist in a certified laboratory, to assess progression or regression of disease and response to therapy in patients with previous atherosclerotic stenosis greater than 50%. Once stability is established over an extended period or candidacy for intervention has changed, longer intervals or termination of surveillance may be appropriate. (Level of Evidence: C)" |
| Class IIb |
| " Duplex ultrasonography to detect hemodynamically significant carotid stenosis may be considered" |
| "1. In asymptomatic patients with symptomatic peripheral arterial disease, coronary artery disease or atherosclerotic aortic aneurysm. (Level of Evidence: C)" |
| "2. To detect carotid stenosis in asymptomatic patients without evidence of atherosclerosis who have greater than or equal to 2 of the following: hypertension, hyperlipidemia, tobacco smoking, or family history of atherosclerosis before age 60 in a first degree relative or ischemic stroke. (Level of Evidence: C)" |
Examples
{{#ev:youtube|nkCmbY_oLAo}}
References
- ↑ Edward G. Grant, Carol B. Benson, Gregory L. Moneta, Andrei V. Alexandrov, J. Dennis Baker, Edward I. Bluth, Barbara A. Carroll, Michael Eliasziw, John Gocke, Barbara S. Hertzberg, Sandra Katanick, Laurence Needleman, John Pellerito, Joseph F. Polak, Kenneth S. Rholl, Douglas L. Wooster, and Eugene Zierler. Carotid Artery Stenosis: Gray-Scale and Doppler US Diagnosis—Society of Radiologists in Ultrasound Consensus Conference. Radiology published online September 18, 2003.
- ↑ Brott TG, Halperin JL, Abbara S, Bacharach JM, Barr JD, Bush RL; et al. (2011). "2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American Stroke Association, American Association of Neuroscience Nurses, American Association of Neurological Surgeons, American College of Radiology, American Society of Neuroradiology, Congress of Neurological Surgeons, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of NeuroInterventional Surgery, Society for Vascular Medicine, and Society for Vascular Surgery". Circulation. 124 (4): 489–532. doi:10.1161/CIR.0b013e31820d8d78. PMID 21282505.