Cavernous malformation
| Cavernous malformation | |
 | |
|---|---|
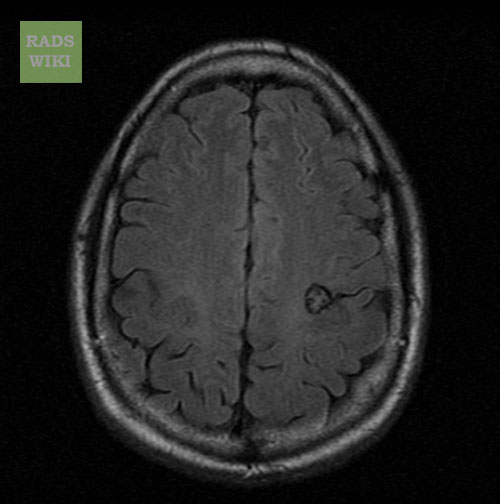
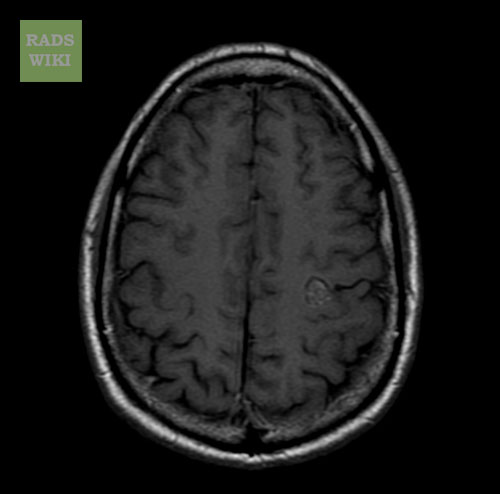
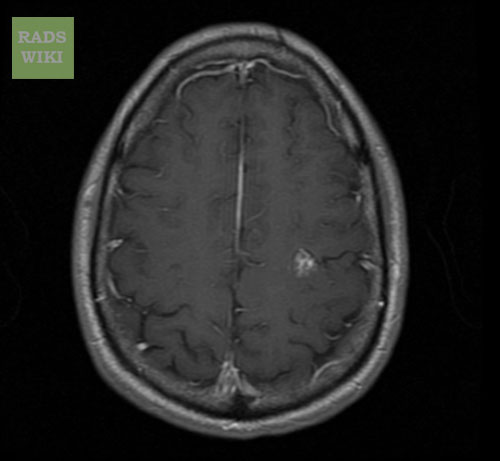
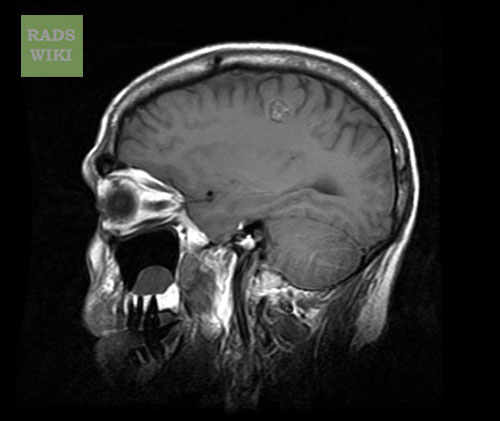
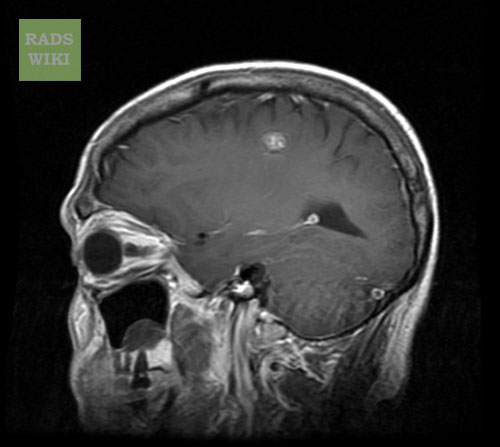
| MRI: Cavernous malformation. (Image courtesy of RadsWiki) |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Cavernous malformations are cavernomas and cavernous angiomas. They are vascular malformations composed of closely approximated endothelial-lined sinusoidal collections without significant amounts of interspersed neural tissue (lack of intervening neural tissue is the only histopathologic characteristic that distinguishes these lesions from capillary telangiectasias).
Cavernous malformations are typically discrete multilobulated lesions that contain hemorrhage in various stages of evolution.
Nearly all cavernous malformations show evidence of recent and remote hemorrhage.
Cavernous malformations vary from several millimeters to several centimeters (usually <3 cm) in diameter.
Epidemiology
With the advent of MRI, cavernous malformation are currently the most commonly identified brain vascular malformations.
Multiple lesions are seen in approximately 15-33% of spontaneous cases.
A familial form of the disorder exists and is inherited as an autosomal dominant trait with variable expression. Multiple lesions are more common in the familial form, occurring in as many as 73% of patients.
Cavernous malformations also appear to be the most common CNS vascular malformation subtype in patients with mixed lesions. The most common combination include a developmental venous anomaly, which is identified in approximately 10-30% of patients with cavernous angiomas.
Risk Stratification
The clinical consequences of hemorrhage vary such that location becomes important.
Small hemorrhages in critical locations can have more severe effects, and thus, they are more likely to produce symptoms (eg, brainstem involvement).
Progressive neurologic deficits are more often associated with cavernous malformations in the infratentorial space and with lesions that demonstrate slow enlargement because of rebleeding episodes.
Diagnosis
Once patients become symptomatic, 40-50% present with seizures, 20% present with focal neurologic deficits, and 10-25% present with intracerebral parenchymal hemorrhage.
Symptoms may progress rapidly, be stable for years; or wax and wane, as in multiple sclerosis.
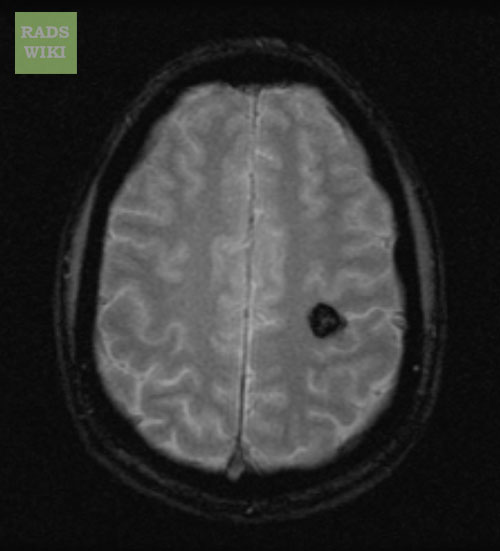
MRI
- Popcorn-like, smoothly circumscribed, well-delineated complex lesions.
- The core is formed by multiple foci of mixed signal intensities, which represents hemorrhage in various stages of evolution.
- The heterogeneous core typically is surrounded completely by a low-signal-intensity hemosiderin rim on T1-weighted images. The hypointensity of this rim becomes more prominent, or blooms, on T2-weighted and gradient-refocused images because of the magnetic susceptibility effects.
- Smaller cavernous malformations may appear as focal hypointense nodules with both T1- and T2-weighted sequences. The small lesions are depicted more clearly and are more numerous on gradient-echo images because of the increased susceptibility effects of the sequences.
Diagnostic Findings
-
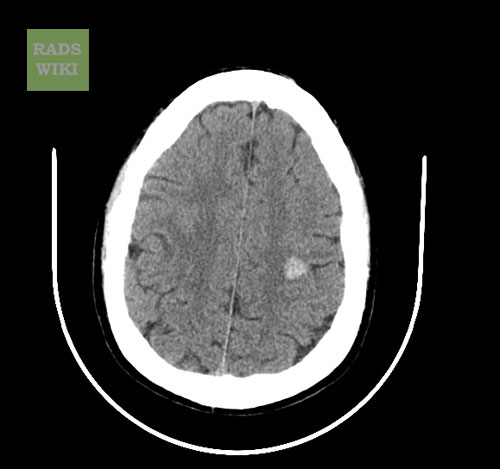
MRI: Cavernous malformation
-
MRI: Cavernous malformation
-
MRI: Cavernous malformation
-
MRI: Cavernous malformation
-
MRI: Cavernous malformation
-
MRI: Cavernous malformation
-
MRI: Cavernous malformation
Prognosis
The risk of hemorrhage is not well established, but it is estimated to be 0.2-2% per lesion per year.
This risk is increased in patients with established prior hemorrhage.
The lesions do not usually produce life-threatening hemorrhages because most hemorrhages associated with the lesions are small and of low pressure.
Cavernous malformations can occur at any age, but they are most likely to become clinically apparent in patients aged 20-40 years.
Frontal and temporal lobes are the most common sites of occurrence, and 80-90% of the lesions are supratentorial.
See Also
External Links
- Goldminer: Cavernoma
- E-medicine Brain, Cavernous Angioma article.