Kernicterus
For patient information, click here
| Kernicterus | |
 | |
|---|---|
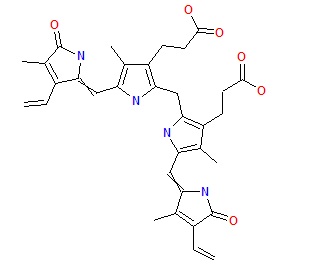
| Bilirubin | |
| ICD-10 | P57 |
| ICD-9 | 773.4, 774.7 |
| DiseasesDB | 7161 |
| MedlinePlus | 003243 |
| MeSH | D007647 |
|
WikiDoc Resources for Kernicterus |
|
Articles |
|---|
|
Most recent articles on Kernicterus Most cited articles on Kernicterus |
|
Media |
|
Powerpoint slides on Kernicterus |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Kernicterus at Clinical Trials.gov Clinical Trials on Kernicterus at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Kernicterus
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Kernicterus Discussion groups on Kernicterus Patient Handouts on Kernicterus Directions to Hospitals Treating Kernicterus Risk calculators and risk factors for Kernicterus
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Kernicterus |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Kernicterus is damage to the brain centers of infants caused by increased levels of unconjugated-indirect bilirubin which is free (not bound to albumin). This may be due to several underlying pathologic processes. Newborn babies are often polycythemic, meaning they have too many red blood cells. When they break down the cells, one of the byproducts is bilirubin, which circulates in the blood and causes jaundice. Alternately, Rh incompatibility between mother and fetus may cause hemolysis of fetal red blood cells, thereby releasing unconjugated bilirubin into the fetal blood. Since the fetal blood brain barrier is not fully formed, some of this released bilirubin enters the brain and interferes with normal neuronal development. Kernicterus may also be found in infants as a symptom of Crigler-Najjar syndrome type I, a hereditary hyperbilirubinemia that is fatal within 18 months of life.
In adults and older children, jaundice is harmless in and of itself. However, the tissues protecting the brain (the blood-brain barrier) are immature in newborns. Bilirubin penetrates the brain and is deposited in the basal ganglia, causing irreversible damage. Depending on the level of exposure, the effects range from unnoticeable to severe brain damage.
Some medications, such as the antibiotic co-trimoxazole (a combination of trimethoprim/sulfamethoxazole) may induce this disorder in the baby, either when taken by the mother or given directly to the baby, due to displacement of bilirubin from binding sites on serum albumin. The bilirubin is then free to pass into the Central Nervous System, because the baby's blood-brain barrier is not fully developed.
The word origantes from the German kern, nucleus, kernel, and the Greek ikterus, jaundice.[1]
References
- ↑ Anja M. Hafkamp (2006). "Oral treatment of unconjugated hyperbilirubinemia" (PDF). PhD thesis. Department of Pediatrics; Center for Liver, Digestive and Metabolic Diseases; University Medical Center Groningen. pp. p. 21. Retrieved 2008-09-06.
Template:Certain conditions originating in the perinatal period