T wave alternans
|
WikiDoc Resources for T wave alternans |
|
Articles |
|---|
|
Most recent articles on T wave alternans Most cited articles on T wave alternans |
|
Media |
|
Powerpoint slides on T wave alternans |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on T wave alternans at Clinical Trials.gov Trial results on T wave alternans Clinical Trials on T wave alternans at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on T wave alternans NICE Guidance on T wave alternans
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on T wave alternans Discussion groups on T wave alternans Patient Handouts on T wave alternans Directions to Hospitals Treating T wave alternans Risk calculators and risk factors for T wave alternans
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for T wave alternans |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editors-In-Chief: Richard L. Verrier, PhD, FACC, and Tuomo Nieminen, MD, PhD
Assistant Editors-in-Chief: Jose Roberto Pegler and Caio Tavares, Medical Students, University of São Paulo, Brazil, in research program at Beth Israel Deaconess Medical Center
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [1] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
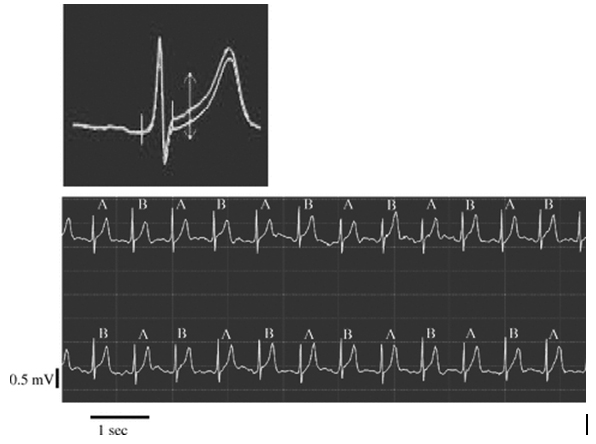
T-wave alternans is a beat-to-beat alternation in the repolarization cycle of the heartbeat. It can be observed in the electrocardiogram (ECG) as a difference in the amplitude and morphology of the ST-segment and/or the T wave among successive odd and even beats in an ABAB pattern (Figure).
(Reprinted with permission from John Wiley & Sons, Inc., from Minkkinen et al, “Enhanced predictive power of quantitative TWA during routine exercise testing in the Finnish Cardiovascular Study,” published in J Cardiovasc Electrophysiol 2009; 20: 408-415.)(1)
Interest is focused on this phenomenon because of its promise in identifying individuals with elevated risk for lethal heart rhythm disturbances and sudden cardiac death, the leading cause of death in the industrially developed world. See video of the ABAB pattern of TWA, which heralds the onset of ventricular fibrillation during myocardial ischemia. The arrhythmia was successfully terminated by defibrillation countershock. [Insert video here]
History of T Wave Alternans
Hering, in 1908, was the first to observe and describe visible macroscopic TWA and its association with increased susceptibility to ventricular tachyarrhythmias.(2) The advent of digital signal processing techniques allowed identification and measurement of nonvisible levels of TWA.
Influence of Physiological Interventions on TWA
TWA is a reflection of spatial gradients in repolarization among neighboring myocardial regions, provoking heterogeneity of repolarization.(3) Its occurrence indicates that the myocardial substrate is altered by pathophysiological processes or pharmacologic agents. At a cellular level, impaired calcium cycling (4) and action potential duration restitution (5,6) are implicated.
TWA magnitude is amplified in parallel with elevated risk of arrhythmias caused by increased heart rate, coronary artery occlusion and reperfusion,(7-9) sympathetic nerve stimulation,(7) mental stress in patients with implantable cardioverter defibrillators (ICDs),(10) and proarrhythmic agents.(11) Heart rate is not the sole determinant of TWA, as raising heart rate by fixed rate pacing does not induce the same levels of TWA as imposing adrenergic factors or myocardial ischemia to reach the same heart rate.(12) Vagus nerve stimulation, pharmacologic blockade of beta-adrenergic receptors,(13) sodium channels,(14, 15) or the angiotensin II receptor,(16) sympathetic denervation,(7) and spinal cord stimulation (17) decrease TWA levels and reduce risk of arrhythmia.
Microvolt TWA and Test Methods
In the 1980’s, Drs. Richard J. Cohen, Joseph M. Smith, David S. Rosenbaum, and colleagues at Massachusetts Institute of Technology and Massachusetts General Hospital (18, 19) and Drs. Richard L. Verrier and Bruce D. Nearing at Georgetown University School of Medicine and later at Beth Israel Deaconess Medical Center, Harvard Medical School,(7-9) applied signal processing techniques to detect visually indiscernible levels of TWA and established that at a microvolt level, TWA discloses risk for lethal cardiac arrhythmias and sudden cardiac death. TWA monitoring can provide valuable information to support overall decision-making to implant an ICD.(20) Recently, Verrier and Nieminen reviewed the body of evidence that indicates the potential value of TWA in guiding medical therapy and detecting risk for proarrhythmia.(11)
Two techniques for TWA analysis currently cleared by the United States Food and Drug Administration for risk stratification for arrhythmic death are the Spectral Method, which emanated from Dr. Cohen’s laboratory and is commercialized by Cambridge Heart, Inc. and Cardiac Sciences, Inc. and the Modified Moving Average method, which resulted from Drs. Verrier and Nearing’s collaboration and is commercialized by GE Healthcare, Inc. and in Europe by Getemed AG.
Spectral Method (SM)
The Fast Fourier Transform is employed to analyze 128 consecutive beats from the J-point to the end of the T wave and produces a power spectrum at 0.5 cycle/beat (on every other beat), which is defined as the alternans power. Since the Spectral Method requires a graded heart-rate increase to a target heart rate, it is usually performed during bicycle ergometry or treadmill exercise. Specialized electrodes are required for noise reduction.
Interpreting Results of Spectral Method
If the TWA level calculated by the Spectral Method exceeds 1.9µV, then the test is considered positive.(21) These patients should be referred to a cardiac electrophysiologist for further evaluation. Results below 1.9µV are interpreted as negative. Several prospective studies have demonstrated that a negative TWA test result with the Spectral Method confirms a low level of risk for an arrhythmic episode, since the test displays a negative predictive value ≥97%,(20, 22) indicating that a negative test correctly identifies ≥97% of patients with diminished risk of developing a lethal cardiac arrhythmia or sudden cardiac death during the next year to two years. Test results may be indeterminate for technical reasons (noise from muscle, respiration, or movement artifact) or because of patient factors (inability to reach a target heart rate of 105-110 beats/min, excessive ectopy, or nonsustained TWA). Indeterminate test results due to patient factors indicate a level of the risk that is equivalent to or greater than a positive test result,(23) and these patients should be immediately retested.
Prognostic Value of the Spectral Method
While the usefulness of the test has been demonstrated in patients with congestive heart failure, ischemic cardiomyopathy, or previous myocardial infarction, its utility in patients with nonischemic dilated cardiomyopathy, in the early post-myocardial infarction period, or in hereditary channelopathies remains unclear.(24)
Modified Moving Average (MMA) Method
This approach employs the noise-rejection principle of recursive averaging.(9) It was designed to allow TWA measurement during routine exercise stress testing [link to exercise stress testing] and ambulatory ECG monitoring [link to ambulatory ECG monitoring], as it circumvents the requirement of heart-rate stabilization and uses standard precordial leads. The algorithm continuously streams odd and even beats into separate bins and creates median complexes for each bin. The complexes are then superimposed and the peak difference between the odd and even median complexes at any point from the J point to the end of the T wave is defined as the TWA value and is updated every 10 to 15 seconds. The influence of new incoming beats is controlled through use of an adjustable update factor; the sensitive 1/8 update factor is recommended. Artifacts due to respiration and motion are reduced by software.
The MMA method reports TWA values in microvolts and presents high-resolution templates of superimposed beats to display the alternation pattern and permit visual overreading to verify the automated TWA measurement. See “How-To Video for TWA Analysis in Ambulatory ECGs.” [Insert video link here.] For more details, see the following from GE Healthcare, Inc.
Interpreting Results of Modified Moving Average Method
Higher TWA values indicate greater risk along a continuum. TWA ≥20µV indicates elevated risk and is particularly useful in combination with other noninvasive markers.(1, 25, 26) TWA ≥46µV as a single cutpoint indicates significantly increased risk.(27-29) Higher optimized values ≥65µV are associated with higher levels of risk, reported in terms of hazard ratios.(28, 30)
Prognostic Value of Modified Moving Average Method
Predictive accuracy of the MMA method for arrhythmic death and cardiovascular mortality has been demonstrated in a population referred for a clinically indicated exercise test (1, 26, 28, 31, 32) and in patients with coronary artery disease,(25, 33) recent or old myocardial infarction,(27, 34) congestive heart failure,(29) and ischemic and nonischemic cardiomyopathy.(30) The largest investigation of MMA-based TWA is the Finnish Cardiovascular Study (FINCAVAS), which enrolled generally low-risk patients who were referred for routine, symptom-limited exercise testing.(1, 26, 28, 31, 32) The MMA technique is also compatible with ambulatory ECG monitoring,(27, 29, 30, 34) atrial pacing, ECG monitoring of immediate post-exercise recovery,(25, 26, 32, 33) and by implantable devices including ICDs.
Comparison of Spectral and Modified Moving Average Methods
TWA values reported by MMA are typically 4- to 10-fold higher than Spectral Method test results. This difference is mainly attributable to the fact that the Spectral Method reports the average TWA level across the entire JT segment for 128 beats, whereas the MMA method reports the peak TWA value for each 15 seconds at any point within the JT interval.
Spectral and MMA analyses have been found in prospective investigations to exhibit similar hazard ratios for predicting sudden cardiac death and cardiovascular mortality when tested in the same population of post-MI patients with better-preserved left ventricular ejection fraction,(25) in matched populations,(30, 35) or in overall hazard ratios.(22, 24) A high negative predictive accuracy of ≥97% is found with both methods.
Clinical Significance
One proposed application of TWA testing has been to identify patients who would not benefit from implantation of an ICD,which rescues patients from a lethal arrhythmia. The current guidelines for ICD implantation state that the main parameter to be analyzed is left ventricular ejection fraction, a measure that does not reveal direct information about the electrical substrate of the heart. Interventional trials have not demonstrated that TWA test results are sufficiently accurate for denying ICD implantation to an otherwise suitable candidate patient,(36-38) as TWA did not predict appropriate ICD discharge in the MASTER trial (37) or in the TWA substudy of SCD-HeFT trial.(38) However, it is well-recognized that ICD discharge may not be an appropriate surrogate endpoint for sudden cardiac death.
A second proposed application of TWA testing is in guiding medical therapy, since many agents that have been shown to reduce incidence of arrhythmias, sudden cardiac death, or cardiovascular mortality also diminish TWA magnitude clinically.(11) These include agents that block beta-adrenergic receptors (13, 39, 40) and angiotensin II receptors.(16, 41) Proarrhythmic effects of cardiovascular and noncardiovascular agents are also indicated by TWA.(11) Thus, drug-induced changes in TWA magnitude may provide an indication of therapeutic efficacy on an individual patient basis.
Frontiers of TWA testing include improvement in prediction based on quantification of TWA magnitude, risk stratification among patients with preserved ejection fraction, the patient group with the highest number of sudden cardiac deaths, and combined use with other noninvasive risk markers to optimize identification of patients whose risk for lethal arrhythmias and sudden cardiac death is elevated. The potential combination parameters include heart rate turbulence,(25, 42) heart rate recovery,(26, 43) or exercise capacity.(32, 44)
Reimbursement for T-Wave Alternans Testing
The 2006 decision summary from the U.S. Center for Medicare and Medicaid Services regarding reimbursement for T-wave alternans testing (CAG-00293N) states: “CMS has determined that there is sufficient evidence to conclude that Microvolt T-wave Alternans (MTWA) diagnostic testing is reasonable and necessary for the evaluation of patients at risk of sudden cardiac death, only when the spectral analytic method is used, and CMS is issuing the following national coverage determination (NCD) for this indication. Microvolt T-wave Alternans (MTWA) diagnostic testing is covered for the evaluation of patients at risk of sudden cardiac death, only when the spectral analytic method is used.” Potential reimbursement for the Modified Moving Average method will be under consideration shortly.
References
1. Minkkinen M, Kähönen M, Viik J, Nikus K, Lehtimäki T, Lehtinen R, Kööbi T, Turjanmaa V, Kaiser W, Verrier RL, Nieminen T. Enhanced predictive power of quantitative TWA during routine exercise testing in the Finnish Cardiovascular Study. J Cardiovasc Electrophysiol 2009; 20: 408-415.
2. Hering HE. Das Wesen des Herzalternans. Muenchener Med Wochenschr 1908; 4:1417-1421.
3. Verrier RL, Kumar K, Nearing BD. Basis for sudden cardiac death prediction by T-wave alternans from an integrative physiology perspective. Heart Rhythm 2009; 6:416-422.
4. Cutler MJ, Rosenbaum DS. Explaining the clinical manifestations of T wave alternans in patients at risk for sudden cardiac death. Heart Rhythm 2009 Mar; 6 (Suppl 3):S22-S28.
5. Weiss JN, Karma A, Shiferaw Y, Chen PS, Garfinkel A, Qu Z. From pulsus to pulseless: The saga of cardiac alternans. Circ Res 2006 May 26; 98:1244-1253.
6. Bayer JD, Narayan SM, Lalani GG, Trayanova NA. Rate-dependent action potential alternans in human heart failure implicates abnormal intracellular calcium handling. Heart Rhythm 2010 Aug; 7(8):1093-1101.
7. Nearing BD, Huang AH, Verrier RL. Dynamic tracking of cardiac vulnerability by complex demodulation of the T-wave. Science 1991; 252:437-440.
8. Nearing BD, Oesterle SN, Verrier RL. Quantification of ischaemia-induced vulnerability by precordial T-wave alternans analysis in dog and human. Cardiovasc Res 1994; 28:1440-49.
9. Nearing BD, Verrier RL. Modified moving average method for T-wave alternans analysis with high accuracy to predict ventricular fibrillation. J Appl Physiol 2002; 92:541-49.
10. Kop WJ, Krantz DS, Nearing BD, Gottdiener JS, Quigley JF, O’Callahan M, Delnegro AA, Friehling TD, Karasik P, Suchday S, Levine J, Verrier RL. Effects of acute mental and exercise stress on T-wave alternans in patients with implantable cardioverter defibrillators and controls. Circulation 2004; 109:1864-69.
11. Verrier RL, Nieminen T. T-wave alternans as a therapeutic marker for antiarrhythmic agents. J Cardiovasc Pharmacol 2010; 55(6):544-554.
12. Kovach JA, Nearing BD, Verrier RL. An angerlike behavioral state potentiates myocardial ischemia-induced T-wave alternans in canines. J Am Coll Cardiol 2001; 37:1719-725.
13. Klingenheben T, Gronefeld G, Li YG, Hohnloser SH. Effect of metoprolol and d,l-sotalol on microvolt-level T-wave alternans. Results of a prospective, double-blind, randomized study. J Am Coll Cardiol 2001; 38:2013-9.
14. Kavesh NG, Shorofsky SR, Sarang SE, Gold MR. The effect of procainamide on T wave alternans. J Cardiovasc Electrophysiol 1999 May; 10:649-54.
15. Nieminen T, Nanbu DY, Datti IP, Vaz GR, Tavares CAM, Pegler JRM, Nearing BD, Belardinelli L, Verrier RL. Antifibrillatory effect of ranolazine during severe coronary stenosis in the intact porcine model. Heart Rhythm, in press.
16. Kubo S, Yoshida A, Kitamura H, Yokoyama M. Acute effects of angiotensin II receptor blocker on ventricular repolarization alternans in chronic heart failure. Kobe J Med Sci 2008 Feb 8; 53:365-74.
17. Issa ZF, Zhou X, Ujhelyi MR, et al. Thoracic spinal cord stimulation reduces the risk of ischemic ventricular arrhythmias in a postinfarction heart failure canine model. Circulation 2005 Jun 21; 111:3217-20.
18. Smith JM, Clancy EA, Valeri CR, Ruskin JM, Cohen RJ. Electrical alternans and cardiac electrical instability. Circulation 1988; 77:110-121.
19. Rosenbaum DS, Jackson LE, Smith JM, Garan H, Ruskin JN, Cohen RJ. Electrical alternans and vulnerability to ventricular arrhythmias. N Engl J Med 1994 Jan 27; 330:235-41.
20. Bloomfield DM, Steinman RC, Namerow PB, et al. Microvolt T-wave alternans distinguishes between patients likely and patients not likely to benefit from implanted cardiac defibrillator therapy: A solution to the Multicenter Automatic Defibrillator Implantation Trial (MADIT) II conundrum. Circulation 2004 Oct 5; 110:1885-9.
21. Bloomfield DM, Hohnloser SH, Cohen RJ. Interpretation and classification of microvolt T wave alternans tests. J Cardiovasc Electrophysiol 2002 May; 13:502-12.
22. Gehi AK, Stein RH, Metz LD, Gomes JA. Microvolt T-wave alternans for the risk stratification of ventricular tachyarrhythmic events: A meta-analysis. J Am Coll Cardiol 2005 Jul 5; 46:75-82.
23. Kaufman ES, Bloomfield DM, Steinman RC, et al. "Indeterminate" microvolt T-wave alternans tests predict high risk of death or sustained ventricular arrhythmias in patients with left ventricular dysfunction. J Am Coll Cardiol 2006 Oct 3; 48:1399-404.
24. Nieminen T, Verrier RL. Usefulness of T-wave alternans in sudden death risk stratification and guiding medical therapy. Ann Noninvasiv Electrocardiol 2010: 15(3):276-288.
25. Exner DV, Kavanagh KM, Slawnych MP, et al. Noninvasive risk assessment early after a myocardial infarction the REFINE study. J Am Coll Cardiol 2007 Dec 11; 50:2275-84.
26. Leino J, Minkkinen M, Nieminen T, Lehtimäki T, Viik J, Lehtinen R, Nikus K, Kööbi T, Turjanmaa V, Verrier RL, Kähönen M. Combined assessment of heart rate recovery and T-wave alternans during routine exercise testing improves prediction of total and cardiovascular mortality: The Finnish Cardiovascular Study. Heart Rhythm 2009; 6:1765-1771.
27. Verrier RL, Nearing BD, LaRovere MT, Pinna GD, Mittleman MA, Bigger JT, Schwartz PJ for the ATRAMI Investigators. Ambulatory ECG-based tracking of T-wave alternans in post-myocardial infarction patients to assess risk of cardiac arrest or arrhythmic death. J Cardiovasc Electrophysiol 2003; 14:705-711.
28. Nieminen T, Lehtimäki T, Viik J, Lehtinen R, Nikus K, Kööbi T, Niemelä K, Turjanmaa V, Kaiser W, Huhtala H, Verrier RL, Huikuri H, Kähönen M. T-wave alternans predicts mortality in a population undergoing a clinically indicated exercise test. Eur Heart J 2007; 28:2332-37.
29. Stein PK, Sanghavi D, Domitrovich PP, Mackey RA, Deedwania P. Ambulatory ECG-based T-wave alternans predicts sudden cardiac death in high-risk post-MI patients with left ventricular dysfunction in the EPHESUS study. J Cardiovasc Electrophysiol 2008 Oct; 19:1037-42.
30. Sakaki K, Ikeda T, Miwa Y, et al. Time-domain T-wave alternans measured from Holter electrocardiograms predicts cardiac mortality in patients with left ventricular dysfunction: A prospective study. Heart Rhythm 2009 Mar; 6:332-7.
31. Leino J, Verrier RL, Minkkinen M, Lehtimäki T, Viik J, Lehtinen R, Nikus K, Kööbi T, Turjanmaa V, Kähönen M, Nieminen T. Importance of regional specificity of T-wave alternans in assessing risk for cardiovascular mortality and sudden cardiac death during routine exercise testing. Heart Rhythm, in press.
32. Minkkinen M, Nieminen T, Verrier RL, Leino J, Lehtimäki T, Viik J, Lehtinen R, Nikus K, Kööbi T, Turjanmaa V, Kähönen M. High predictivity for mortality with combined analysis of exercise capacity, heart rate recovery and T-wave alternans during routine exercise testing. Heart Rhythm 2009; 6 [suppl]:S92.
33. Slawnych MP, Nieminen T, Kahonen M, et al. Post-exercise assessment of cardiac repolarization alternans in patients with coronary artery disease using the modified moving average method. J Am Coll Cardiol 2009 Mar 31; 53:1130-7.
34. Maeda S, Nishizaki M, Yamawake N, et al. Ambulatory ECG-based T-wave alternans and heart rate turbulence predict high risk of arrhythmic events in patients with old myocardial infarction. Circ J 2009 Dec; 73:2223-8.
35. Ikeda T, Saito H, Tanno K, et al. T-wave alternans as a predictor for sudden cardiac death after myocardial infarction. Am J Cardiol 2002 Jan 1; 89:79-82.
36. Costantini O, Hohnloser SH, Kirk MM, et al. The ABCD (Alternans Before Cardioverter Defibrillator) trial: Strategies using T-wave alternans to improve efficiency of sudden cardiac death prevention. J Am Coll Cardiol 2009 Feb 10; 53:471-9.
37. Gold MR, Ip JH, Costantini O, et al. Role of microvolt T-wave alternans in assessment of arrhythmia vulnerability among patients with heart failure and systolic dysfunction: Primary results from the T-wave Alternans Sudden Cardiac Death in Heart Failure Trial substudy. Circulation 2008 Nov 11; 118:2022-8.
38. Chow T, Kereiakes DJ, Onufer J, et al. Does microvolt T-wave alternans testing predict ventricular tachyarrhythmias in patients with ischemic cardiomyopathy and prophylactic defibrillators? The MASTER (Microvolt T-wave Alternans Testing for Risk Stratification of Post-Myocardial Infarction Patients) trial. J Am Coll Cardiol 2008 Nov 11; 52:1607-15.
39. Olsson G, Wikstrand J, Warnold I, et al. Metoprolol-induced reduction in postinfarction mortality: Pooled results from five double-blind randomized trials. Eur Heart J 1992 Jan; 13:28-32.
40. Chan PS, Gold MR, Nallamothu BK. Do beta-blockers impact microvolt T-wave alternans testing in patients at risk for ventricular arrhythmias? A meta-analysis. J Cardiovasc Electrophysiol 2010 Sept; 21: 1009–14.
41. Domanski MJ, Exner DV, Borkowf CB, Geller NL, Rosenberg Y, Pfeffer MA. Effect of angiotensin converting enzyme inhibition on sudden cardiac death in patients following acute myocardial infarction. A meta-analysis of randomized clinical trials. J Am Coll Cardiol 1999 Mar; 33:598-604.
42. Bauer A, Malik M, Schmidt G, et al. Heart rate turbulence: Standards of measurement, physiological interpretation, and clinical use: International Society for Holter and Noninvasive Electrocardiology consensus. J Am Coll Cardiol 2008 Oct 21; 52:1353-65.
43. Cole CR, Blackstone EH, Pashkow FJ, Snader CE, Lauer MS. Heart-rate recovery immediately after exercise as a predictor of mortality. N Engl J Med 1999 Oct 28; 341:1351-7.
44. Kokkinos P, Myers J, Kokkinos JP, et al. Exercise capacity and mortality in black and white men. Circulation 2008 Feb 5; 117:614-22.
External Links
- Cambrdige Heart Manufacturer of Microvolt T-wave Alternans Systems
- GE Healthcare Manufacturer of Marquette MMA T-wave Alternans Stress Test and Holter Systems