Chlamydia
Template:DiseaseDisorder infobox
|
WikiDoc Resources for Chlamydia |
|
Articles |
|---|
|
Most recent articles on Chlamydia |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Chlamydia at Clinical Trials.gov Clinical Trials on Chlamydia at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Chlamydia
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Chlamydia Discussion groups on Chlamydia Directions to Hospitals Treating Chlamydia Risk calculators and risk factors for Chlamydia
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Chlamydia |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Chlamydia is a common term for Chlamydiae. This term derives from the name of the bacterial genus Chlamydia in the family Chlamydiaceae, order Chlamydiales, class and phylum Chlamydiae, ultimately from Greek χλαμύδος "cloak". There are two genera in Chlamydiaceae: Chlamydia and Chlamydophila. There is still some controversy surrounding the establishment of a second genus as the rationale for this is poorly justified. The genus Chlamydia includes three species: C. trachomatis, C. muridarum, and C. suis. C. trachomatis infection is described below.
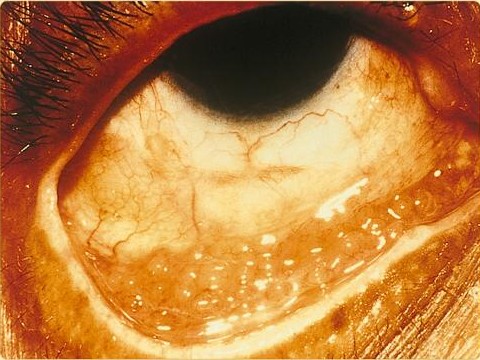
Chlamydia trachomatis is a major infectious cause of human eye and genital disease. C. trachomatis is naturally found living only inside human cells and is one of the most common sexually transmitted infections in people worldwide — about 2.8 million cases of chlamydia infection occur in the United States each year.[1] Not all infected people exhibit symptoms of infection. Between half and three-quarters of all women who have chlamydia have no symptoms and do not know that they are infected. It can be serious but is easily cured with appropriate antibiotics if detected in time. Equally important, chlamydia infection of the eye is the most common cause of preventable blindness in the world. Blindness occurs as a complication of trachoma (chlamydia conjunctivitis).[2]
There are many other species of Chlamydiae that live in the cells of animals (including humans), insects, or protozoa. Two of these species cause lung infection in humans: Chlamydia pneumoniae and Chlamydophila psittaci.
Symptoms

Chlamydia is an asymptomatic disease for 50-70% of the female population. Of those who have an asymptomatic infection that is not detected by their doctor, approximately half will develop pelvic inflammatory disease (PID), a generic term for infection of the uterus, fallopian tubes, and/or ovaries. PID can cause scarring inside the reproductive organs, which can later cause serious complications, including chronic pelvic pain, difficulty becoming pregnant, ectopic (tubal) pregnancy, and other dangerous complications of pregnancy. Chlamydia causes 250,000 to 500,000 cases of PID every year in the U.S. Women infected with chlamydia are up to five times more likely to become infected with HIV, if exposed.[3]
Chlamydia is known as the "Silent Epidemic" because in women, it may not cause any symptoms and will linger for months or years before being discovered. Symptoms that may occur include: unusual vaginal bleeding or discharge, pain in the abdomen, painful sexual intercourse, fever, painful urination or the urge to urinate more frequently than usual.
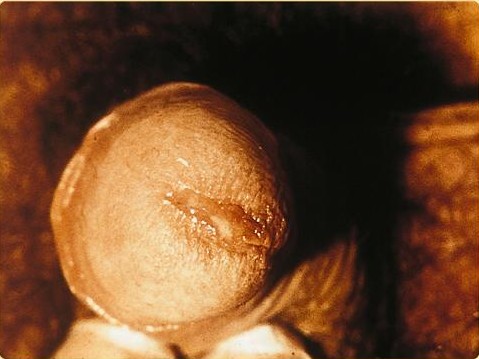
In men, chlamydia is symptomatic in greater than 90% of cases. Symptoms that may occur include: a painful or burning sensation when urinating, an unusual discharge from the penis, swollen or tender testicles, or fever. Discharge, or the purulent exudate, is generally less viscous and lighter in color than for gonorrhea.
Chlamydia in men can spread to the testicles, causing epididymitis, which can cause sterility if not treated within 6 to 8 weeks. Chlamydia causes more than 250,000 cases of epididymitis in the USA each year.
Chlamydia may also cause reactive arthritis, especially in young men. (Some forms of reactive arthritis formerly were known as Reiter's syndrome. The latter term has fallen out of favor owing to revelations about Hans Reiter's Nazi past and in particular his alleged active participation in horrific human experiments in concentration camps.) About 15,000 men develop reactive arthritis due to chlamydia infection each year in the USA, and about 5,000 are permanently affected by it.
As many as half of all infants born to mothers with chlamydia will be born with the disease. Chlamydia can affect infants by causing spontaneous abortion; premature birth; conjunctivitis, which may lead to blindness; and pneumonia. Conjunctivitis due to chlamydia typically occurs one week after birth (Compare with chemical causes (within hours) or gonorrhea (2-5 days)).
Detection
1. Heavy bleeding on periods. The diagnosis of genital chlamydial infections evolved rapidly from the 1990s through 2006. Nucleic acid amplification tests (NAAT), such as polymerase chain reaction (PCR), transcription mediated amplification (TMA), and the DNA strand displacement assay (SDA) now are the mainstays. As of January 2007, the most commonly used and widely studied chlamydia NAATs in the US and many other industrialized countries are Aptima (Gen-Probe), Probe-Tec (Becton-Dickinson), and Amplicor (Roche). The Aptima Combo II assay tests simltaneously for C. trachomatis and Neisseria gonorrhoeae, the cause of gonorrhea. NAAT for chlamydia may be performed on swab specimens collected from the cervix (women) or urethra (men), on self-collected vaginal swabs, or on voided urine. Urine and self-collected swab testing facilitates the performance of screening tests in settings where genital examination is impractical. At present, the NAATs have regulatory approval only for testing urogenital specimens, although rapidly evolving research indicates that the Aptima test may give reliable results on rectal specimens.
Because of improved test accuracy, ease of specimen management, convenience in specimen management, and ease of screening sexually active men and women, the NAATs have largely replaced culture, the historic gold standard for chlamydia diagnosis, and the non-amplified probe tests, such as Pace II (Gen-Probe). The latter test is relatively insensitive, successfully detecting only 60-80% of infections in asymptomatic women, and occasionally giving falsely positive results. Culture remains useful in selected circumstances and is currently the only assay approved for testing non-genital specimens.
Treatment
C. trachomatis infection can be effectively cured with antibiotics once it is detected. Current Centers for Disease Control guidelines provide for the following treatments:
- Azithromycin 1 gram oral as a single dose, or
- Doxycycline 100 milligrams twice daily for seven days.
- Tetracycline
- Erythromycin
Untested Treatments
- Ciprofloxacin 500 milligrams twice daily for 3 days.
- (Although this is not an approved method of treatment, as it is shown to be ineffective and may simply delay symptoms.)
β-lactams are not suitable drugs for the treatment of chlamydia. While they have the ability to halt growth of the organism (i.e. are microbistatic), these antibiotics do not eliminate the bacteria. Once treatment is stopped, the bacteria will begin to grow once more. (See below for Persistence.)
Pathophysiology
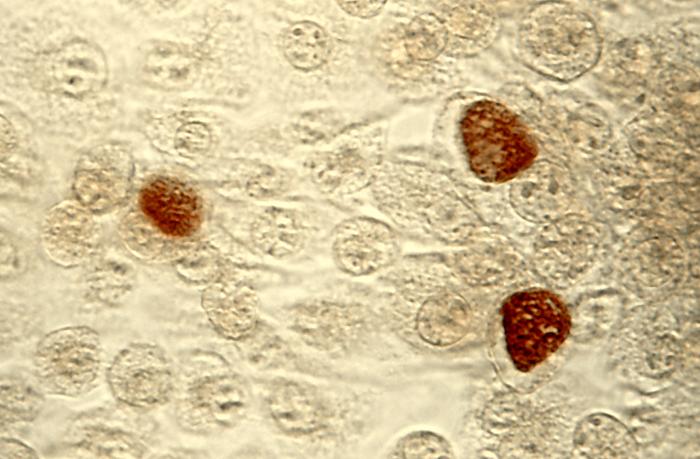
Chlamydial Life Cycle Chlamydiae are obligate, intracellular bacterial pathogens, which means they are unable to replicate outside of a host cell. However, to disseminate effectively, these pathogens have evolved a unique biphasic life cycle wherein they alternate between two functionally and morphologically distinct forms. The elementary body (EB) is infectious but metabolically inert, much like a spore, and can survive for limited amounts of time in the extracellular milieu. Once the EB attaches to a susceptible host cell, it mediates its own internalization through pathogen-specified mechanisms (via type III secretion system) that allows for the recruitment of actin with subsequent engulfment of the bacterium. The internalized EB, within a membrane-bound compartment, immediately begins differentiation into the reticulate body (RB). RBs are metabolically active but non-infectious and, in many regards, resemble normal replicating bacteria. The intracellular bacteria rapidly modifies its membrane-bound compartment into the so-called chlamydial inclusion so as to prevent phagosome-lysosome fusion. According to published data, the inclusion has no interactions with the endocytic pathway and apparently inserts itself into the exocytic pathway as it retains the ability to intercept sphingomyelin-containing vesicles. To date, no one has been able to detect a host cell protein that is trafficked to the inclusion through the exocytic pathway. As the RBs replicate, the inclusion grows as well to accommodate the increasing numbers of organisms. Through unknown mechanisms, RBs begin a differentiation program back to the infectious EBs, which are released from the host cell to initiate a new round of infection. Because of their obligate intracellular nature, chlamydiae has no tractable genetic system, like E. coli, which makes this and related organisms difficult to investigate.
Persistence Chlamydiae have the ability to establish long-term associations with host cells. When an infected host cell is starved for various nutrients such as amino acids (e.g. tryptophan), iron, or vitamins, this has a negative consequence for chlamydiae since the organism is dependent on the host cell for these nutrients. The starved chlamydiae enter a persistent growth state wherein they stop cell division and become morphologically aberrant by increasing in size. Persistent organisms remain viable as they are capable of returning to a normal growth state once conditions in the host cell improve. There is much debate as to whether persistence has in vivo relevance. Many believe that persistent chlamydiae are the cause of chronic chlamydial diseases. Some antibiotics such as β-lactams can also induce a persistent-like growth state, which can contribute to the chronicity of chlamydial diseases.
Diseases caused by Chlamydia trachomatis
Chlamydia trachomatis can cause the following conditions:
Recent genetic discoveries
Recent phylogenetic studies have revealed that chlamydia shares a common ancestor with modern plants, and retains unusual plant-like traits (both genetically and physiologically). In particular, the enzyme L,L-diaminopimelate aminotransferase, which is related to lysine production in plants, is also linked with the construction of chlamydia's cell wall. The genetic encoding for the enzymes is remarkably similar in plants and chlamydia, demonstrating a close common ancestry.
This unexpected discovery may help scientists develop new treatment avenues: if scientists could find a safe and effective inhibitor of L,L-diaminopimelate aminotransferase, they might have a highly effective and extremely specific new antibiotic against chlamydia.
References
- ↑ Chlamydia fact sheet from the Centers for Disease Control and Prevention
- ↑ Belland R, Ojcius D, Byrne G (2004). "Chlamydia". Nat Rev Microbiol. 2 (7): 530 &ndash, 1. PMID 15248311.
External links
| Wikimedia Commons has media related to Chlamydia. |
- "Chlamydia: Questions and Answers" from Planned Parenthood"
- Chlamydia Symptoms and Pictures
- NetDoctor Chlamydia fact sheet
- Links to chlamydia pictures (Hardin MD/Univ of Iowa)
- Resources for research on chlamydial infections
Template:STD/STI Template:Bacterial diseases
ar:كلاميديا da:Klamydia de:Chlamydien he:כלמידיה mk:Хламидија ms:Penyakit kelamin Chlamydia nl:Chlamydia no:Klamydia-infeksjon sl:Klamidioza fi:Klamydia sv:Klamydia ta:கிளமிடியா Template:SIB