Paroxysmal AV block Electrophysiologic studies
Overview
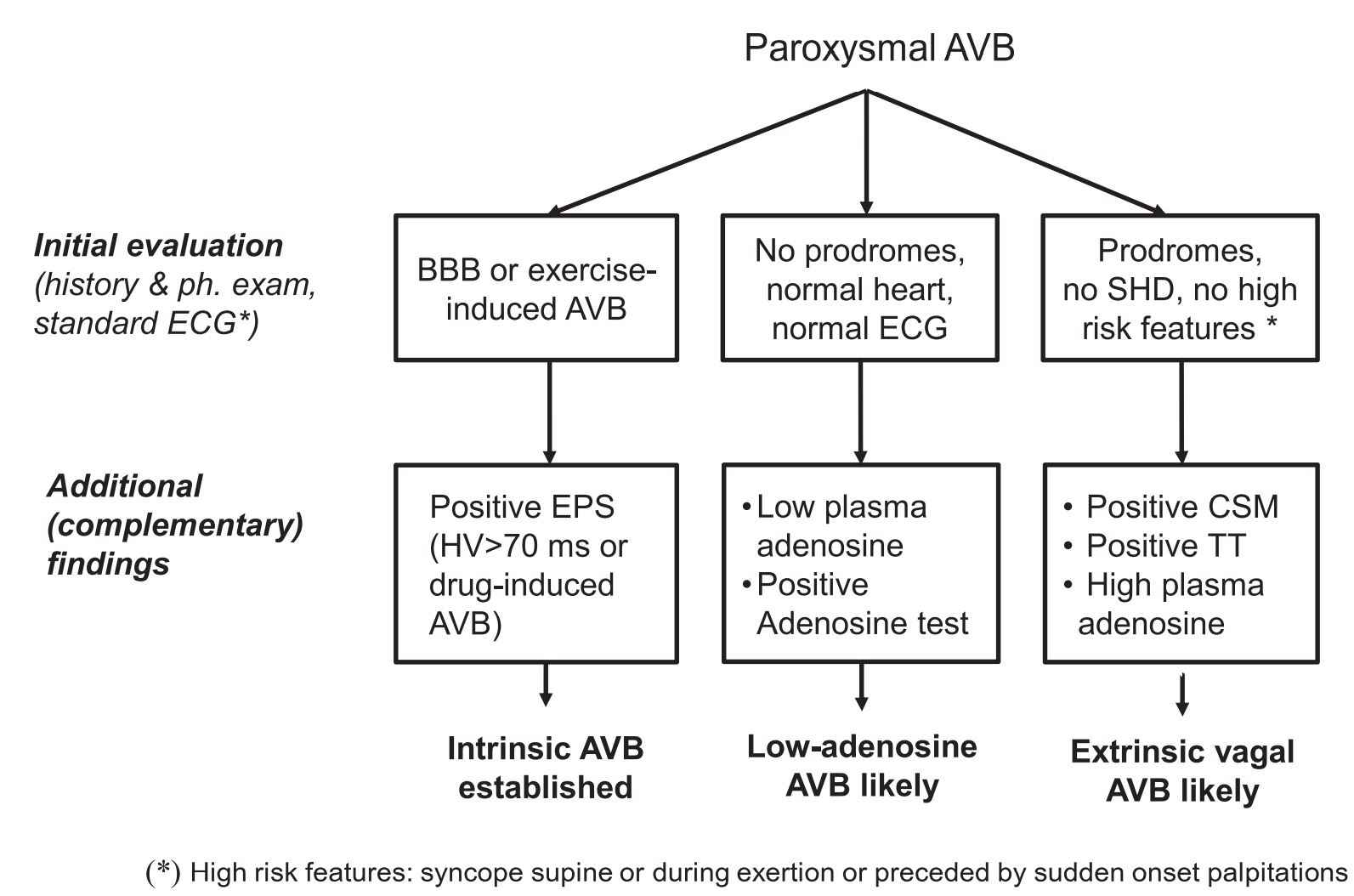
An EPS is an invasive catheter based procedure that is employed to detect and anatomically locate conduction disorders. An increased HH interval is seen in intrinsic paroxysmal AV Block.
Electrophysiologic studies (EPS)
- The decision to perform an EPS requires a global risk assessment.
- The application of this study is most important in diagnosing I-AVB.
- According to the European Society of Cardiology, indications for EPS are as follows :
- In patients with syncope and previous myocardial infarction or other scar related conditions, EPS is indicated when syncope remains unexplained after non- invasive evaluation.
- In patients with syncope and asymptomatic sinus bradycardia, EPS may be considered in a few instances where no invasive tests (eg. ECG monitoring) have failed to show a correlation between syncope and bradycardia.
- In patients with syncope preceded by sudden and brief palpitations, EPS may be considered when syncope remains unexplained after non invasive evaluation. "ESC Guidelines on Syncope (Diagnosis and Management of)".
EPS guided therapy
- In patients with unexplained syncope and bifasicular bundle branch block, a pacemaker is indicated in the presence of either a baseline H-V interval of more than or equal to 70ms, or second or third degree His- Purkinje block during incremental atrial pacing, or with pharmacological challenge.
- In patients with unexplained syncope and previous myocardial infarction or scar related condition, it is recommended to manage induction of sustained monomorphic ventricular tachycardia according to the current European Society of Cardiology Guidelines for Ventricular Arrhythmias.
- In patients without structural heart disease with syncope preceded by sudden and brief palpitations, it is recommended to manage the induction of rapid SVT or VT, which reproduces hypotensive or spontaneous symptoms, with appropriate therapy according to the current European Society of Cardiology Guidelines.
- In patients with syncope and asymptomatic sinus bradycardia, a pacemaker should be considered is a prolonged sinus node recovery time is present."ESC Guidelines on Syncope (Diagnosis and Management of)".
- A 42 month follow up was performed by Gronda et al in 155 patients, majority of whom had a history of previous syncope.
- Electrophysiologic study findings of basal HV greater than or equal to 65 ms , HV value greater than or equal to 120 ms or 2nd-3rd degree atrioventricular block during ajmaline test and HV prolonged greater than 10 ms or 2nd-3rd degree atrioventricular block during atrial pacing correlated to an increased risk of developing advanced atrioventricular block below the AV node.[1]
2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay
| Recommendation for Electrophysiology Testing |
| "1. In patients with symptoms suspected to be attributable to bradycardia, an electrophysiology study (EPS) may be considered in selected patients for diagnosis of, and elucidation of bradycardia mechanism, if initial noninvasive evaluation is nondiagnostic(Level of Evidence: C-LD)[2]" |
- An EPS is an invasive catheter based procedure that is employed to detect and anatomically locate conduction disorders.
- It is well tolerated, has a low complication risk and not usually employed as a first line study in the diagnosis of bradycardia related disorders. [2]
References
- ↑ Gronda M, Magnani A, Occhetta E, Sauro G, D'Aulerio M, Carfora A; et al. (1984). "Electrophysiological study of atrio-ventricular block and ventricular conduction defects. Prognostic and therapeutical implications". G Ital Cardiol. 14 (10): 768–73. PMID 6519386.
- ↑ 2.0 2.1 Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR; et al. (2019). "2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society". J Am Coll Cardiol. 74 (7): 932–987. doi:10.1016/j.jacc.2018.10.043. PMID 30412710.