Testicular torsion
| Testicular torsion - wd1 | |
 | |
|---|---|
| ICD-10 | N44 |
| ICD-9 | 608.2 |
| OMIM | 187400 |
| DiseasesDB | 12984 |
| eMedicine | med/2780 |
| MeSH | D013086 |
Template:Search infobox Steven C. Campbell, M.D., Ph.D.
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [1] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
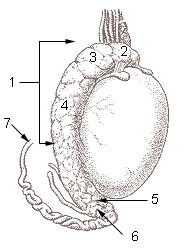
In testicular torsion the spermatic cord that provides the blood supply to a testicle is twisted, cutting off the blood supply, often causing orchalgia. Prolonged testicular torsion will result in the death of the testicle and surrounding tissues.
It is also believed that torsion occurring during fetal development can lead to the so-called neonatal torsion or vanishing testis, and is one of the causes of an infant being born with monorchism.
Risk factors
In most males, the testicles are attached to the inner lining of the scrotum. Males whose attachment is higher up are at risk of testicular torsion. This condition is known as a bell clapper deformity (as in the central piece of a bell) and is a major cause of testicular torsion. A male who notices the ability of either or both testicles to freely rotate within the scrotum should be aware that he is at risk of testicular torsion. Testicles that are in a much lower position and/or in a slightly rotated position in the scrotal sack are a visual indicator of this risk.
Torsions are sometimes called "winter syndrome". This is because they often happen in winter, when it is cold outside. The scrotum of a man who has been lying in a warm bed is relaxed. When he arises, his scrotum is exposed to the colder room air. If the spermatic cord is twisted while the scrotum is loose, the sudden contraction that results from the abrupt temperature change can trap the testicle in that position. The result is a testicular torsion.
Prevalence
While torsion is more frequent among adolescents, it should be considered in all cases where there is testicular pain. Torsion occurs more frequently in patients who do not have evidence of inflammation or infection. Two risk factors are trauma and strenuous physical activity.
Diagnosis
Emergency testing for torsion may be indicated when the onset of pain is sudden and/or severe, or the test results available during the initial examination do not enable a diagnosis of urethritis or urinary tract infection to be made. A doppler ultrasound scan of the scrotum, if available, is of immense help in the diagnosis by showing the presence or absence of blood flow to the testicle. Dizziness and nausea are often present when there is an absence of blood supply to the testicle, as well as a tremendous amount of pain. If the diagnosis is questionable, an expert should be consulted immediately, because testicular viability may be compromised. If physical examination suggests a compromised blood supply and the patient has had such symptoms for a significant period of time, medical personnel may choose to bring the patient directly to surgery without an ultrasound since the time required for ultrasound testing could affect testicular viability.
Color Doppler sonography (color printout of an ultrasound echo test) is used to identify the absence of blood flow typically found in a twisted testicle, which distinguishes the condition from epididymitis. [1]
Urinalysis (analyzing chemical composition of urine) can be used to rule out bacterial infections.
Surgical exploration may be necessary if diagnosis cannot be made using other methods. If there is the slightest hint of a torsion of the testicle, then doctors will perform surgery; even if the testicle turns out not to have twisted, they will still protect it by attaching the testicle to the scrotum wall.
Treatment
With prompt diagnosis and treatment the testicle can be saved in a high number of cases.[2]
Testicular torsion is a medical emergency that needs immediate treatment. If treated within 6 hours, there is nearly a 100% chance of saving the testicle. Within 12 hours this rate decreases to 70%, within 24 hours is 20%, and after 24 hours the rate approaches 0. (eMedicineHealth) Once the testicle is dead it must be removed to prevent gangrenous infection.
A simple and minor surgery will correct and prevent testicular torsion. It can be done in an emergency situation after determination that the testicle is cut off from blood supply or as an outpatient procedure for patients who have experienced frequent episodes with testicular torsion. If necessary, the surgeon will first untwist the testicle(s). The surgeon will then permanently suture the testicles to the inner lining of the scrotum. If only one testicle has been problematic, the surgeon may suture both testicles as a preventative effort.
References
- ↑ Arce J, Cortés M, Vargas J (2002). "Sonographic diagnosis of acute spermatic cord torsion. Rotation of the cord: a key to the diagnosis". Pediatr Radiol. 32 (7): 485–91. PMID 12107581.
- ↑ Cattolica E, Karol J, Rankin K, Klein R (1982). "High testicular salvage rate in torsion of the spermatic cord". J Urol. 128 (1): 66–8. PMID 7109074.
External links
Adapted from the public domain document Centers for Disease Control and Prevention. 1998 Guidelines for Treatment of Sexually Transmitted Diseases. MMWR 1998;47(No. RR-1) at http://wonder.cdc.gov/wonder/STD/STD98TG/STD98T12.HTM and other sources.
Template:Diseases of the pelvis, genitals and breasts Template:SIB
de:Hodentorsion it:Torsione del testicolo nl:Torsio testis fi:Kiveksen kiertyminen