Doxycycline (oral)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Kiran Singh, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Doxycycline (oral) is an antibiotic that is FDA approved for the treatment of inflammatory lesions (papules and pustules) of rosacea. Common adverse reactions include anorexia,nausea,vomiting, diarrhea, dysphagia,edema, urticaria, hemolytic anaemia, neutropenia, eosinophilia.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indication
- ORACEA is indicated for the treatment of only inflammatory lesions (papules and pustules) of rosacea in adult patients. No meaningful effect was demonstrated for generalized erythema (redness) of rosacea.
Limitations of Use
- This formulation of doxycycline has not been evaluated in the treatment or prevention of infections. ORACEA should not be used for treating bacterial infections, providing antibacterial prophylaxis, or reducing the numbers or eliminating microorganisms associated with any bacterial disease.
- To reduce the development of drug-resistant bacteria as well as to maintain the effectiveness of other antibacterial drugs, ORACEA should be used only as indicated.
- Efficacy of ORACEA beyond 16 weeks and safety beyond 9 months have not been established.
- ORACEA has not been evaluated for the treatment of the erythematous, telangiectatic, or ocular components of rosacea.
Dosage
General Dosing Information
- One ORACEA Capsule (40 mg) should be taken once daily in the morning on an empty stomach, preferably at least one hour prior to or two hours after meals.
- Administration of adequate amounts of fluid along with the capsules is recommended to wash down the capsule to reduce the risk of esophageal irritation and ulceration.
Important Considerations for Dosing Regimen
- The dosage of ORACEA differs from that of doxycycline used to treat infections. Exceeding the recommended dosage may result in an increased incidence of side effects including the development of resistant organisms.
Dosage Forms And Strengths
- 40 mg beige opaque capsule imprinted with “GLD 40”
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
- Acinetobacter infection: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses.
- Acinetobacter infection: severe infections, 100 mg ORALLY every 12 hours.
- Acne vulgaris; Adjunct: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses.
- Acne vulgaris; Adjunct: severe infections, 100 mg ORALLY every 12 hours.
- Actinomycotic infection: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses.
- Actinomycotic infection: severe infections, 100 mg ORALLY every 12 hours.
- Amebic infection - Intestinal infectious disease: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses.
- Amebic infection - Intestinal infectious disease: severe infections, 100 mg ORALLY every 12 hours [2]
- Anthrax: (inhalational, postexposure) 100 mg ORALLY every 12 hours for 60 days; in combination with 1 to 2 additional antibiotics.
- Anthrax: (cutaneous, postexposure) 100 mg ORALLY every 12 hours for 60 days; (cutaneous, naturally occurring) 100 mg every 12 hours for 7 to 10 days.
- Bartonellosis: (bacillary angiomatosis, peliosis hepatis, bacteremia, osteomyelitis in patients with HIV) 100 mg ORALLY every 12 hours for at least 3 months (guideline dosing).
- Bartonellosis: (CNS infection or severe infections in patients with HIV) 100 mg ORALLY every 12 hours, with or without rifampin 300 mg ORALLY or IV every 12 hours for 4 months.
- Bartonellosis: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses; for severe infections, 100 mg ORALLY every 12 hours.
- Brucellosis; Adjunct: 200 mg ORALLY daily for 6 weeks in combination with streptomycin (clinical trial dosing).
- Brucellosis; Adjunct: 100 mg ORALLY every 12 hours on day 1, then 100 mg ORALLY daily OR 100 mg ORALLY every 12 hours for more severe infections (manufacturer dosing).
- Chancroid: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses.
- Chancroid: severe infections, 100 mg ORALLY every 12 hours.
- Chlamydial infection: 100 mg ORALLY twice daily for 7 days.
- Cholera: 300 mg ORALLY as a single dose or 100 mg ORALLY twice a day for 3 days.
- Clostridial infection: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses.
- Clostridial infection: severe infections, 100 mg ORALLY every 12 hours.
- Epididymitis: 100 mg ORALLY every twice daily for 10 days plus ceftriaxone 250 mg IM as a single dose.
- Gonorrhea, Uncomplicated: (infection of the cervix, urethra, or rectum) 100 mg ORALLY twice daily for 7 days plus a single dose of either IM ceftriaxone 250 mg or ORAL cefixime 400 mg.
- Gonorrhea, Uncomplicated: (infection of the pharynx) 100 mg ORALLY twice daily for 7 days plus a single dose of ceftriaxone 250 mg IM.
- Gonorrhea, Uncomplicated: (except anorectal infections in men) 100 mg ORALLY every 12 hours for 7 days or 300 mg single dose followed in 1 hour by another 300 mg single dose (manufacturer dosing)
- Granuloma inguinale: 100 mg ORALLY twice daily for at least 21 days and lesions are healed completely.
- Human anaplasmosis: 100 mg twice daily ORALLY for 10 days for human granulocytic anaplasmosis alone or concomitant Lyme disease.
- Inclusion conjunctivitis: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses.
- Inclusion conjunctivitis: severe infections, 100 mg ORALLY every 12 hours.
- Infection by Campylobacter fetus: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses.
- Infection by Campylobacter fetus: severe infections, 100 mg ORALLY every 12 hours.
- Infection due to Enterobacteriaceae: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses.
- Infection due to Enterobacteriaceae: severe infections, 100 mg ORALLY every 12 hours.
- Infection due to Escherichia coli: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses.
- Infection due to Escherichia coli: severe infections, 100 mg ORALLY every 12 hours.
- Infection of skin AND/OR subcutaneous tissue: (methicillin-susceptible Staphylococcus aureus or MRSA) 100 mg ORALLY twice daily (guideline dosing).
- Infective endocarditis: (documented Bartonella endocarditis, culture positive) 100 mg ORALLY every 12 hours for 6 weeks AND gentamicin sulfate 1 mg/kg IV/IM every 8 hours for 2 weeks.
- Infective endocarditis: (suspected Bartonella endocarditis, culture negative) 100 mg ORALLY every 12 hours for 6 weeks, in combination with ceftriaxone sodium 2 g IV/IM every 24 hours for 6 weeks AND gentamicin sulfate 1 mg/kg IV/IM every 8 hours for 2 weeks.
- Infective proctitis: 100 mg ORALLY twice daily for 7 days plus ceftriaxone 250 mg IM as a single dose .
- Inhalational anthrax, Postexposure; Prophylaxis: 100 mg ORALLY every 12 hours for at least 60 days.
- Late latent syphilis, or latent syphilis of unknown duration; Penicillin allergy: 100 mg ORALLY twice daily for 28 days.
- Listeriosis: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses.
- Listeriosis: severe infections, 100 mg ORALLY every 12 hours.
- Lyme disease: 100 mg twice daily ORALLY for 14 days (range, 10 to 21 days) in early localized or early disseminated Lyme disease associated with erythema migrans; for 14 days (range, 14 to 21 days) in Lyme carditis to complete a course of therapy or to treat ambulatory patients; for 14 days (range, 14 to 21 days) for seventh cranial-nerve palsy with no CNS involvement; for 28 days for Lyme arthritis without neurological involvement; for 14 days (range, 10 to 21 days) for borrelial lymphocytoma; for 21 days for acrodermatitis chronica atrophicans.
- Lyme disease: (intolerant of beta-lactam agents) 200 to 400 mg/day ORALLY in 2 divided doses for 14 days (range, 10 to 28 days) for Lyme meningitis or seventh-cranial-nerve palsy with CNS involvement; for 14 days (range, 14 to 21 days) for Lyme carditis for the initial treatment of hospitalized patients.
- Lyme disease; Prophylaxis: 200 mg ORALLY as a single dose .
- Lymphogranuloma venereum: 100 mg ORALLY twice daily for 21 days.
- Malaria; Adjunct: (uncomplicated) 100 mg ORALLY twice daily for 7 days; give in combination with quinine sulfate 650 mg ORALLY 3 times daily for 3 days (or 7 days if infection is acquired in Southeast Asia) (guideline dosing).
- Malaria; Adjunct: (severe) 100 mg ORALLY twice daily for 7 days; give in combination with quinidine gluconate 10 mg/kg IV loading dose over 1 to 2 hours then 0.02 mg/kg/min IV continuous infusion for at least 24 hours, and continue for 3 days if infection acquired in Africa or South America or 7 days if infection is acquired in Southeast Asia; may switch to oral quinine once parasite density is less than 1% (guideline dosing).
- Malaria; Prophylaxis: 100 mg ORALLY once a day beginning 1 to 2 days prior to travel, continued during travel, and for 4 weeks after travel to malarious area .
- Nongonococcal cervicitis: 100 mg ORALLY twice daily for 7 days.
- Nongonococcal urethritis: 100 mg ORALLY twice daily for 7 days.
- Operative procedure on female genital system including obstetrics - Postoperative infection; * Prophylaxis: (hysterosalpingography or chromotubation) 100 mg ORALLY twice daily for 5 days.
- Operative procedure on female genital system including obstetrics - Postoperative infection; Prophylaxis: (surgical abortion) 100 mg ORALLY 1 hour prior and 200 mg after procedure.
- Pelvic inflammatory disease: 100 mg ORALLY every 12 hours in combination with cefoxitin 2 g IV every 6 hours or cefotetan 2 g IV every 12 hours (recommended) or ampicillin/sulbactam 3 g IV every 6 hours (alternative); other alternative is doxycycline 100 mg ORALLY twice daily with or without metronidazole 500 mg ORALLY twice daily for 14 days plus a single IM dose of either ceftriaxone 250 mg or cefoxitin 2 g (for cefoxitin, also give probenecid 1 g orally as a single dose).
- Plague: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses.
- Plague: severe infections, 100 mg ORALLY every 12 hours.
- Psittacosis: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses.
- Psittacosis: severe infections, 100 mg ORALLY every 12 hours.
- Q fever: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses.
- Q fever: severe infections, 100 mg ORALLY every 12 hours.
- Relapsing fever: 100 mg ORALLY twice a day for a total of 5 to 10 days.
- Respiratory tract infection: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses; severe infections, 100 mg ORALLY every 12 hours.
- Respiratory tract infection: (acute uncomplicated bacterial rhinosinusitis; initial empiric therapy alternative) 100 mg ORALLY twice daily OR 200 mg ORALLY daily for 5 to 7 days (guideline dosing).
- Rocky Mountain spotted fever: 100 mg ORALLY every 12 hours; treat for at least 3 days following resolution of fever and until clinical improvement is observed; total duration is typically 7 to 14 days OR 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses; for more severe infections, 100 mg ORALLY every 12 hours.
- Rosacea, inflammatory lesions (papules and pustules): 40 mg ORALLY once daily in the morning (1 hour before or 2 hours after a meal).
- Sexually transmitted infectious disease; Prophylaxis - Victim of sexual aggression: 100 mg ORALLY twice daily for 7 days plus metronidazole 2 g ORALLY as a single dose plus either ceftriaxone 250 mg IM or cefixime 400 mg orally as a single dose.
- Shigellosis: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses.
- Shigellosis: severe infections, 100 mg ORALLY every 12 hours.
- Spotted fevers: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses.
- Spotted fevers: severe infections, 100 mg ORALLY every 12 hours.
- Staphylococcal infection of skin: (tablet) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses [22]
- Staphylococcal infection of skin: (tablet) severe infections, 100 mg ORALLY every 12 hours, including for MRSA-associated purulent cellulitis
- Syphilis, Primary, secondary, or early latent; Penicillin allergy: early, 100 mg ORALLY twice daily for 14 days
- Syphilis, Primary, secondary, or early latent; Penicillin allergy: infection of over one year's duration, 100 mg ORALLY every 12 hours for 4 weeks
- Tularemia, Postexposure: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses
- Tularemia, Postexposure: severe infections, 100 mg ORALLY every 12 hours
- Typhus group rickettsial disease: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses
- Typhus group rickettsial disease: severe infections, 100 mg ORALLY every 12 hours
- Urinary tract infectious disease: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses
- Urinary tract infectious disease: severe infections, 100 mg ORALLY every 12 hours [3]
- Vincent's infection: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses
- Vincent's infection: severe infections, 100 mg ORALLY every 12 hours
- Yaws: 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses
- Yaws: severe infections, 100 mg ORALLY every 12 hours
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of doxycycline in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of doxycycline in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
- Use of drugs in the tetracycline class, including doxycycline, is not recommended in infants and children younger than 8 years.
- Doxycycline extended-release capsule formulation (Oracea(TM)) is not recommended for use in children of any age.
- Acinetobacter infection: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses or 100 mg ORALLY every 12 hours if severe infection.
- Acne vulgaris; Adjunct: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses or severe infections, 100 mg ORALLY every 12 hours if severe infection.
- Actinomycotic infection: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses or 100 mg ORALLY every 12 hours if severe infection.
- Amebic infection - Intestinal infectious disease: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) use adult dose.
- Anthrax: (older than 8 years, under 45 kg) 2.2 mg/kg ORALLY every 12 hours for 60 days, in combination with 1 to 2 additional antibiotics; (older than 8 years, over 45 kg) use adult dose
- Bartonellosis: (cutaneous bacillary angiomatosis in patients with HIV) 2 to 4 mg/kg/day (MAX 100 to 200 mg/day) ORALLY once daily or divided into 2 doses/day for 3 months (guideline dosing).
- Bartonellosis: (bacillary peliosis, osteomyelitis, severe or CNS infections in patients with HIV) 2 to 4 mg/kg/day (MAX 100 to 200 mg/day) ORALLY once daily or divided into 2 doses/day for 4 months; add rifampin 20 mg/kg (MAX 600 mg/day) ORALLY or IV once daily or divided into 2 doses/day for CNS and severe infections (guideline dosing).
- Bartonellosis: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses, or continue 100 mg ORALLY every 12 hours for severe infections (manufacturer dosing).
- Brucellosis; Adjunct: (older than 8 years) 2 to 4 mg/kg ORALLY per day in 2 divided doses for at least 6 weeks; MAX 200 mg/day; monotherapy not recommended, use in conjunction with rifampin (guideline dosing).
- Brucellosis; Adjunct: (older than 8 years) 45 kg or less, 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 up to 4.4 mg/kg/day (if severe infection) ORALLY in 1 to 2 divided doses; 45 kg or greater, 100 mg ORALLY every 12 hours on day 1, then 100 mg ORALLY daily (manufacturer dosing) [6]
- Chancroid: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses or 100 mg ORALLY every 12 hours if severe infection.
- Chlamydial infection: (8 years or older) 100 mg ORALLY twice daily for 7 days.
- Clostridial infection: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses or 100 mg ORALLY every 12 hours if severe infection.
- Gonorrhea, Uncomplicated: (greater than 45 kg; infection of the cervix, urethra, or rectum) 100 mg ORALLY twice daily for 7 days plus a single dose of either IM ceftriaxone 250 mg or ORAL cefixime 400 mg (guideline dosing).
- Gonorrhea, Uncomplicated: (greater than 45 kg, infection of the pharynx) 100 mg ORALLY twice daily for 7 days plus a single dose of IM ceftriaxone 250 mg.
- Human anaplasmosis: (8 years or older) 4 mg/kg per day ORALLY in 2 divided doses for 10 days for human granulocytic anaplasmosis alone or concomitant Lyme disease; maximum 100 mg/dose [10]
- Human anaplasmosis: (severely ill, younger than 8 years without concomitant Lyme disease) 4 mg/kg per day ORALLY in 2 divided doses for 4 to 5 days (eg; for approximately 3 days after resolution of fever); maximum 100 mg/dose .
- Human anaplasmosis: (severely ill, younger than 8 years with concomitant Lyme disease) 4 mg/kg per day ORALLY in 2 divided doses for 4 to 5 days (eg; for approximately 3 days after resolution of fever); maximum 100 mg/dose; amoxicillin or cefuroxime axetil should be used after the conclusion of the course of doxycycline to complete a 14-day total course .
- Inclusion conjunctivitis: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses or 100 mg ORALLY every 12 hours if severe infection .
- Infection by Campylobacter fetus: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses or 100 mg ORALLY every 12 hours for severe infection.
- Infection due to Enterobacteriaceae: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses or 100 mg ORALLY every 12 hours if severe infection.
- Infection due to Escherichia coli: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses or 100 mg ORALLY every 12 hours if severe infection.
- Infective endocarditis: (documented Bartonella endocarditis, culture positive) 1 to 2 mg/kg ORALLY (MAX dose: 100 mg) every 12 hours for 6 weeks AND gentamicin sulfate 1 mg/kg IV/IM every 8 hours for 2 weeks.
- Infective endocarditis: (suspected Bartonella endocarditis, culture negative) 1 to 2 mg/kg ORALLY (MAX dose: 100 mg) every 12 hours for 6 weeks AND ceftriaxone sodium 100 mg/kg (MAX dose: 2 g) IV/IM every 24 hours for 6 weeks AND gentamicin sulfate 1 mg/kg IV/IM every 8 hours for 2 weeks
- Inhalational anthrax, Postexposure; Prophylaxis: (under 45 kg) 2.2 mg/kg (maximum, 100 mg/dose) ORALLY every 12 hours for at least 60 days; (older than 8 years AND over 45 kg) 100 mg ORALLY every 12 hours for at least 60 days.
- Listeriosis: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses or 100 mg ORALLY every 12 hours if severe infection.
- Lyme disease: (8 years or older) 4 mg/kg ORALLY in 2 divided doses for 14 days (range, 10 to 21 days) in early localized or early disseminated Lyme disease associated with erythema migrans; for 14 days (range, 14 to 21 days) in Lyme carditis to complete a course of therapy or to treat ambulatory patients; for 14 days (range, 14 to 21 days) for seventh-cranial-nerve palsy with no CNS involvement; for 28 days for Lyme arthritis without neurological involvement; for 14 days (range, 10 to 21 days) for borrelial lymphocytoma; for 21 days for acrodermatitis chronica atrophicans; maximum daily dose, 200 mg.
- Lyme disease: (8 years or older, intolerant of beta-lactam agents) 4 to 8 mg/kg/day ORALLY in 2 divided doses for 14 days (range, 10 to 28 days) for Lyme meningitis or seventh-cranial-nerve palsy with CNS involvement; for 14 days (range, 14 to 21 days) for Lyme carditis for the initial treatment of hospitalized patients; maximum daily dose, 200 to 400 mg.
- Lyme disease; Prophylaxis: (older than 8 years) 4 mg/kg ORALLY as a single dose; maximum 200 mg.
- Malaria; Adjunct: (uncomplicated, 8 years or older) 2.2 mg/kg (MAX: 100 mg) ORALLY every 12 hours for 7 days; give in combination with quinine sulfate 10 mg/kg ORALLY 3 times daily for 3 days (or 7 days if infection is acquired in Southeast Asia) (guideline dosing).
- Malaria; Adjunct: (severe, 8 years or older, weight 45 kg or greater) 100 mg ORALLY twice daily for 7 days; give in combination with quinidine gluconate 10 mg/kg IV loading dose over 1 to 2 hours then 0.02 mg/kg/min IV continuous infusion for at least 24 hours, and continue for 3 days if infection acquired in Africa or South America or 7 days if infection is acquired in Southeast Asia; may switch to oral quinine once parasite density is less than 1% (guideline dosing).
- Malaria; Adjunct: (severe, 8 years or older, weight less than 45 kg) 2.2 mg/kg ORALLY every 12 hours for 7 days; give in combination with quinidine gluconate 10 mg/kg IV loading dose over 1 to 2 hours then 0.02 mg/kg/min IV continuous infusion for at least 24 hours and continue for 3 days if infection acquired in Africa or South America or 7 days if infection is acquired in Southeast Asia, may switch to oral quinine once parasite density is less than 1% (guideline dosing).
- Malaria; Prophylaxis: (older than 8 years) 2 mg/kg ORALLY (up to 100 mg/day) once a day beginning 1 to 2 days prior to travel, continued during travel, and for 4 weeks after travel to malarious area.
- Plague: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) use adult dose.
- Psittacosis: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses or 100 mg ORALLY every 12 hours if severe infection.
- Q fever: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses or 100 mg ORALLY every 12 hours if severe infection.
- Relapsing fever: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses for a total of 5 to 10 days.
- Relapsing fever: (older than 8 years, over 45 kg) 100 mg ORALLY twice a day for a total of 5 to 10 days.
- Respiratory tract infection: (older than 8 years; 45 kg or less) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 mg/kg/day ORALLY in 1 to 2 divided doses; severe infections, may use up to 4.4 mg/kg/day.
- Respiratory tract infection: (older than 8 years; over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses; severe infections, 100 mg ORALLY every 12 hours.
- Rocky Mountain spotted fever: (over 45 kg) 100 mg ORALLY every 12 hours; treat for at least 3 days following resolution of fever and until clinical improvement is observed; total duration is typically 7 to 14 days [21] OR (older than 8 years, over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses; for more severe infections, 100 mg ORALLY every 12 hours.
- Rocky Mountain spotted fever: (under 45 kg) 2.2 mg/kg ORALLY twice daily; treat for at least 3 days following resolution of fever and until clinical improvement is observed; total duration is typically 7 to 14 days [21] OR (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY divided in 2 doses on day 1, then 2.2 mg/kg/day ORALLY in 1 to 2 divided doses; for more severe infections, up to 4.4 mg/kg/day may be used.
- Rosacea, inflammatory lesions (papules and pustules): 40 mg ORALLY once daily in the morning (1 hour before or 2 hours after a meal).
- Shigellosis: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses or 100 mg ORALLY every 12 hours if severe infection.
- Spotted fevers: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) use adult dose.
- Staphylococcal infection of skin: (older than 8 years, 45 kg or less) for MRSA-associated purulent cellulitis, 4 mg/kg/day ORALLY divided every 12 hours (guideline dosing).
- Staphylococcal infection of skin: (older than 8 years, over 45 kg) for MRSA-associated purulent cellulitis.
- Tularemia, Postexposure: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 up to 4.4 mg/kg/day (if severe infection) ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses or 100 mg ORALLY every 12 hours if severe infection .
- Typhus group rickettsial disease: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses or 100 mg ORALLY every 12 hours if severe infection.
- Urinary tract infectious disease: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses or 100 mg ORALLY every 12 hours if severe infection.
- Vincent's infection: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day 1, then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses or 100 mg ORALLY every 12 hours if severe infection.
- Yaws: (older than 8 years, under 45 kg) 4.4 mg/kg ORALLY in 1 to 2 divided doses on day, 1 then 2.2 to 4.4 mg/kg/day ORALLY in 1 to 2 divided doses; (older than 8 years, over 45 kg) 100 mg ORALLY every 12 hours on day 1, then 100 mg/day ORALLY in 1 to 2 divided doses or 100 mg ORALLY every 12 hours if severe infection.
Non–Guideline-Supported Use
There is limited information regarding FDA-Labeled Use of doxycycline in pediatric patients.
Contraindications
- This drug is contraindicated in persons who have shown hypersensitivity to doxycycline or any of the other tetracyclines.
Warnings
Teratogenic Effects
- ORACEA should not be used during pregnancy.
- Doxycycline, like other tetracycline-class antibiotics, can cause fetal harm when administered to a pregnant woman. If any tetracycline is used during pregnancy or if the patient becomes pregnant while taking these drugs, the patient should be informed of the potential hazard to the fetus and treatment stopped immediately.
- The use of drugs of the tetracycline-class during tooth development (last half of pregnancy, infancy, and childhood up to the age of 8 years) may cause permanent discoloration of the teeth (yellow-gray-brown). This adverse reaction is more common during long-term use of the drug but has been observed following repeated short-term courses. Enamel hypoplasia has also been reported. Tetracycline drugs, therefore, should not be used during tooth development unless other drugs are not likely to be effective or are contraindicated.
- All tetracyclines form a stable calcium complex in any bone-forming tissue. A decrease in fibula growth rate has been observed in premature human infants given oral tetracycline in doses of 25 mg/kg every 6 hours. This reaction was shown to be reversible when the drug was discontinued.
- Results of animal studies indicate that tetracyclines cross the placenta, are found in fetal tissues, and can cause retardation of skeletal development on the developing fetus. Evidence of embryotoxicity has been noted in animals treated early in pregnancy.
Pseudomembranous Colitis
- Clostridium difficile associated diarrhea (CDAD) has been reported with nearly all antibacterial agents, including doxycycline, and may range in severity from mild to fatal colitis.
- Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
- C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
- If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
Metabolic Effects
- The anti-anabolic action of the tetracyclines may cause an increase in BUN. While this is not a problem in those with normal renal function, in patients with significantly impaired function, higher serum levels of tetracycline-class antibiotics may lead to azotemia, hyperphosphatemia, and acidosis. If renal impairment exists, even usual oral or parenteral doses may lead to excessive systemic accumulations of the drug and possible liver toxicity. Under such conditions, lower than usual total doses are indicated, and if therapy is prolonged, serum level determinations of the drug may be advisable.
Photosensitivity
- Photosensitivity manifested by an exaggerated sunburn reaction has been observed in some individuals taking tetracyclines. Although this was not observed during the duration of the clinical studies with ORACEA, patients should minimize or avoid exposure to natural or artificial sunlight (tanning beds or UVA/B treatment) while using ORACEA. If patients need to be outdoors while using ORACEA, they should wear loose-fitting clothes that protect skin from sun exposure and discuss other sun protection measures with their physician.
Autoimmune Syndromes
- Tetracyclines have been associated with the development of autoimmune syndromes. Symptoms may be manifested by fever, rash , arthralgia, and malaise. In symptomatic patients, liver function tests, ANA, CBC, and other appropriate tests should be performed to evaluate the patients. Use of all tetracycline-class drugs should be discontinued immediately.
Tissue Hyperpigmentation
- Tetracycline-class drugs are known to cause hyperpigmentation. Tetracycline therapy may induce hyperpigmentation in many organs, including nails, bone, skin, eyes, thyroid, visceral tissue, oral cavity (teeth, mucosa, alveolar bone), sclerae and heart valves. Skin and oral pigmentation has been reported to occur independently of time or amount of drug administration, whereas other pigmentation has been reported to occur upon prolonged administration. Skin pigmentation includes diffuse pigmentation as well as over sites of scars or injury.
Pseudotumor cerebri
- Pseudotumor cerebri (benign intracranial hypertension) in adults has been associated with the use of tetracyclines. The usual clinical manifestations are headache and blurred vision. Bulging fontanels have been associated with the use of tetracyclines in infants. While both of these conditions and related symptoms usually resolve after discontinuation of the tetracycline, the possibility for permanent sequelae exists. Patients should be questioned for visual disturbances prior to initiation of treatment with tetracyclines and should be routinely checked for papiledema while on treatment.
Development of Drug Resistant Bacteria
- Bacterial resistance to tetracyclines may develop in patients using ORACEA. Because of the potential for drug-resistant bacteria to develop during the use of ORACEA, it should only be used as indicated.
Superinfection
- As with other antibiotic preparations, use of ORACEA may result in overgrowth of non-susceptible microorganisms, including fungi. If superinfection occurs, ORACEA should be discontinued and appropriate therapy instituted. Although not observed in clinical trials with ORACEA, the use of tetracyclines may increase the incidence of vaginal candidiasis. ORACEA should be used with caution in patients with a history of or predisposition to Candida overgrowth.
Laboratory Monitoring
- Periodic laboratory evaluations of organ systems, including hematopoietic, renal and hepatic studies should be performed. Appropriate tests for autoimmune syndromes should be performed as indicated.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- Adverse Reactions in Clinical Trials of ORACEA: In controlled clinical trials of adult subjects with mild to moderate rosacea, 537 subjects received ORACEA or placebo over a 16-week period. The following table summarizes selected adverse reactions that occurred in the clinical trials at a rate of >1% for the active arm:

Adverse Reactions for Tetracyclines: The following adverse reactions have been observed in patients receiving tetracyclines at higher, antimicrobial doses:
- Gastrointestinal: anorexia, nausea, vomiting, diarrhea, glossitis, dysphagia, enterocolitis, and inflammatory lesions (with vaginal candidiasis) in the anogenital region. Hepatotoxicity has been reported rarely. Rare instances of esophagitis and esophageal ulcerations have been reported in patients receiving the capsule forms of the drugs in the tetracycline-class. Most of the patients experiencing esophagitis and/or esophageal ulceration took their medication immediately before lying down.
- Skin: maculopapular and erythematous rashes. Exfoliative dermatitis has been reported but is uncommon. Photosensitivity is discussed above .
- Renal toxicity: rise in BUN has been reported and is apparently dose-related.
- Hypersensitivity reactions: urticaria , angioneurotic edema, anaphylaxis, anaphylactoid purpura, serum sickness, pericarditis, and exacerbation of systemic lupus erythematosus.
- Blood: hemolytic anemia, thrombocytopenia, neutropenia, and eosinophilia have been reported.
Postmarketing Experience
- Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. The following adverse reactions have been identified during postapproval use of ORACEA.
• Nervous system: pseudotumor cerebri (benign intracranial hypertension), headache
Drug Interactions
Anticoagulants
- Because tetracyclines have been shown to depress plasma prothrombin activity, patients who are on anticoagulant therapy may require downward adjustment of their anticoagulant dosage.
Penicillin
- Since bacteriostatic drugs may interfere with the bactericidal action of penicillin, it is advisable to avoid giving tetracycline-class drugs in conjunction with penicillin.
Methoxyflurane
- The concurrent use of tetracycline and methoxyflurane has been reported to result in fatal renal toxicity.
Antacids and Iron Preparations
- Absorption of tetracyclines is impaired by bismuth subsalicylate, proton pump inhibitors, antacids containing aluminum, calcium or magnesium and iron-containing preparations.
Low Dose Oral Contraceptives
- Doxycycline may interfere with the effectiveness of low dose oral contraceptives. To avoid contraceptive failure, females are advised to use a second form of contraceptive during treatment with doxycycline.
Oral Retinoids
- There have been reports of pseudotumor cerebri (benign intracranial hypertension) associated with the concomitant use of isotretinoin and tetracyclines. Since both oral retinoids, including isotretinoin and acitretin, and the tetracyclines, primarily minocycline, can cause increased intracranial pressure, the concurrent use of an oral retinoid and a tetracycline should be avoided.
Barbiturates and Anti-epileptics
- Barbiturates, carbamazepine, and phenytoin decrease the half-life of doxycycline.
Drug/Laboratory Test Interactions
- False elevations of urinary catecholamine levels may occur due to interference with the fluorescence test
Use in Specific Populations
Pregnancy
- Teratogenic Effects: Pregnancy Category D. Results from animal studies indicate that doxycycline crosses the placenta and is found in fetal tissues.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of doxycycline in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of doxycycline during labor and delivery.
Nursing Mothers
- Tetracyclines are excreted in human milk. Because of the potential for serious adverse reactions in infants from doxycycline, ORACEA should not be used in mothers who breastfeed.
Pediatric Use
- ORACEA should not be used in infants and children less than 8 years of age. ORACEA has not been studied in children of any age with regard to safety or efficacy, therefore use in children is not recommended.
Geriatic Use
- Clinical studies of ORACEA did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and concomitant disease or other drug therapy.
Gender
There is no FDA guidance on the use of doxycycline with respect to specific gender populations.
Race
There is no FDA guidance on the use of doxycycline with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of doxycycline in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of doxycycline in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of doxycycline in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of doxycycline in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
Monitoring
There is limited information regarding Monitoring of doxycycline in the drug label.
IV Compatibility
There is limited information regarding IV Compatibility of doxycycline in the drug label.
Overdosage
- In case of overdosage, discontinue medication, treat symptomatically, and institute supportive measures. Dialysis does not alter serum half-life and thus would not be of benefit in treating cases of overdose.
Pharmacology
Mechanism of Action
- The mechanism of action of ORACEA in the treatment of inflammatory lesions of rosacea is unknown.
Structure
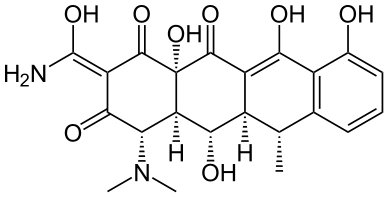
- ORACEA (doxycycline, USP) Capsules 40 mg are hard gelatin capsule shells filled with two types of doxycycline beads (30 mg immediate release and 10 mg delayed release) that together provide a dose of 40 mg of anhydrous doxycycline (C22H24N2O8).
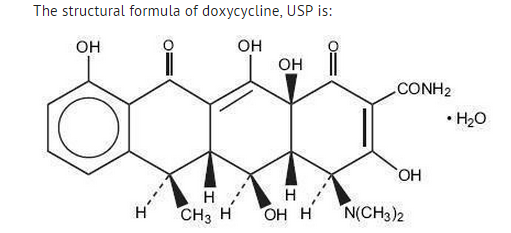
- With an empirical formula of C22H24N2O8•H2O and a molecular weight of 462.46. The chemical designation for doxycycline is 2-Naphthacenecar-boxamide,4-(dimethylamino)-1,4,4a,5,5a,6,11,12a-octahydro-3,5,10,12,12a-pentahydroxy-6-methyl-1,11-dioxo-, [4S-(4α, 4aα, 5α, 5aα, 6α,12aα)]-, monohydrate. It is very slightly soluble in water.
- Inert ingredients in the formulation are: hypromellose, iron oxide red, iron oxide yellow, methacrylic acid copolymer, polyethylene glycol, Polysorbate 80, sugar spheres, talc, titanium dioxide, and triethyl citrate. Active ingredients: Each capsule contains doxycycline, USP in an amount equivalent to 40 mg of anhydrous doxycycline.
Pharmacodynamics
There is limited information regarding pharmacodynamics of doxycycline in the drug label.
Pharmacokinetics
- ORACEA capsules are not bioequivalent to other doxycycline products. The pharmacokinetics of doxycycline following oral administration of ORACEA was investigated in 2 volunteer studies involving 61 adults. Pharmacokinetic parameters for ORACEA following single oral doses and at steady-state in healthy subjects are presented in Table 2.
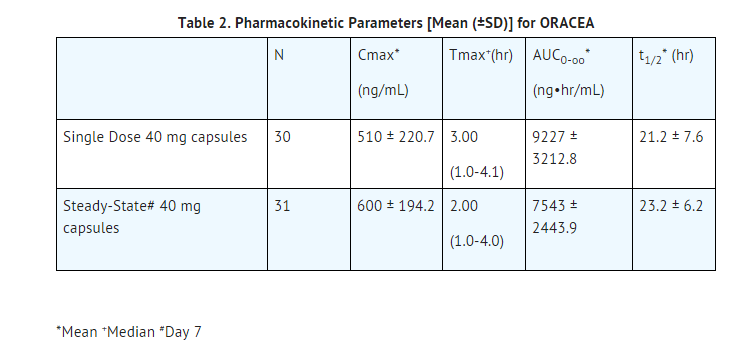
- Absorption: In a single-dose food-effect study involving administration of ORACEA to healthy volunteers, concomitant administration with a 1000 calorie, high-fat, high-protein meal that included dairy products, resulted in a decrease in the rate and extent of absorption (Cmax and AUC) by about 45% and 22%, respectively, compared to dosing under fasted conditions. This decrease in systemic exposure can be clinically significant, and therefore if ORACEA is taken close to meal times, it is recommended that it be taken at least one hour prior to or two hours after meals.
- Distribution: Doxycycline is greater than 90% bound to plasma proteins.
- Metabolism: Major metabolites of doxycycline have not been identified. However, enzyme inducers such as barbiturates, carbamazepine, and phenytoin decrease the half-life of doxycycline.
- Excretion: Doxycycline is excreted in the urine and feces as unchanged drug. It is reported that between 29% and 55.4% of an administered dose can be accounted for in the urine by 72 hours. Terminal half-life averaged 21.2 hours in subjects receiving a single dose of ORACEA.
Special Populations
- Geriatric: Doxycycline pharmacokinetics have not been evaluated in geriatric patients.
- Pediatric: Doxycycline pharmacokinetics have not been evaluated in pediatric patients.
- Gender: The pharmacokinetics of ORACEA were compared in 16 male and 14 female subjects under fed and fasted conditions. While female subjects had a higher Cmax and AUC than male subjects, these differences were thought to be due to differences in body weight/lean body mass.
- Race: Differences in doxycycline pharmacokinetics among racial groups have not been evaluated.
- Renal Insufficiency: Studies have shown no significant difference in serum half-life of doxycycline in patients with normal and severely impaired renal function. Hemodialysis does not alter the serum half-life of doxycycline.
- Hepatic Insufficiency: Doxycycline pharmacokinetics have not been evaluated in patients with hepatic insufficiency.
- Gastric Insufficiency:In a study in healthy volunteers (N=24) the bioavailability of doxycycline is reported to be reduced at high pH. This reduced bioavailability may be clinically significant in patients with gastrectomy, gastric bypass surgery or who are otherwise deemed achlorhydric.
Drug Interactions:
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Doxycycline was assessed for potential to induce carcinogenesis in a study in which the compound was administered to Sprague-Dawley rats by gavage at dosages of 20, 75, and 200 mg/kg/day for two years. An increased incidence of uterine polyps was observed in female rats that received 200 mg/kg/day, a dosage that resulted in a systemic exposure to doxycycline approximately 12.2 times that observed in female humans who use ORACEA [exposure comparison based upon area under the curve (AUC) values]. No impact upon tumor incidence was observed in male rats up to at 200 mg/kg/day, or in females at the lower dosages studied.
- Doxycyline was assessed for potential to induce carcinogenesis in CD-1 mice by gavage at dosages 20, 75, and 150 mg/kg/day in males and at dosages of 20, 100, and 300 mg/kg/day in females. No impact upon tumor incidence was observed in male and female mice at systemic exposures approximately 4.2 and 8.3 times that observed in humans, respectively.
- Doxycycline demonstrated no potential to cause genetic toxicity in an in vitro point mutation study with mammalian cells (CHO/HGPRT forward mutation assay) or in an in vivo micronucleus assay conducted in CD-1 mice. However, data from an in vitro mammalian chromosomal aberration assay conducted with CHO cells suggest that doxycycline is a weak clastogen. Oral administration of doxycycline to male and female Sprague-Dawley rats adversely affected fertility and reproductive performance, as evidenced by increased time for mating to occur, reduced sperm motility, velocity, and concentration, abnormal sperm morphology, and increased pre-and post-implantation losses. Doxycycline induced reproductive toxicity at all dosages that were examined in this study, as even the lowest dosage tested (50 mg/kg/day) induced a statistically significant reduction in sperm velocity. Note that 50 mg/kg/day is approximately 3.6 times the amount of doxycycline contained in the recommended daily dose of ORACEA when compared on the basis of AUC estimates. Although doxycycline impairs the fertility of rats when administered at sufficient dosage, the effect of ORACEA on human fertility is unknown.
Clinical Studies
- The safety and efficacy of ORACEA in the treatment of only inflammatory lesions (papules and pustules) of rosacea was evaluated in two randomized, placebo-controlled, multi-centered, double-blind, 16-week Phase 3 trials involving 537 subjects (total of 269 subjects on ORACEA from the two trials) with rosacea (10 to 40 papules and pustules and two or fewer nodules). Pregnant and nursing women, subjects <18 years of age, and subjects with ocular rosacea and/or blepharitis/meibomianitis who require ophthalmologic treatment were excluded from trial. Mean baseline lesion counts were 20 and 21 for ORACEA and placebo subject groups respectively.
- At Week 16, subjects in the ORACEA group were evaluated using co-primary endpoints of mean reduction in lesion counts and a dichotomized static Investigators Global Assessment of Clear or Almost Clear (defined as 1 to 2 small papules or pustules) when compared to the placebo group in both Phase 3 trials.
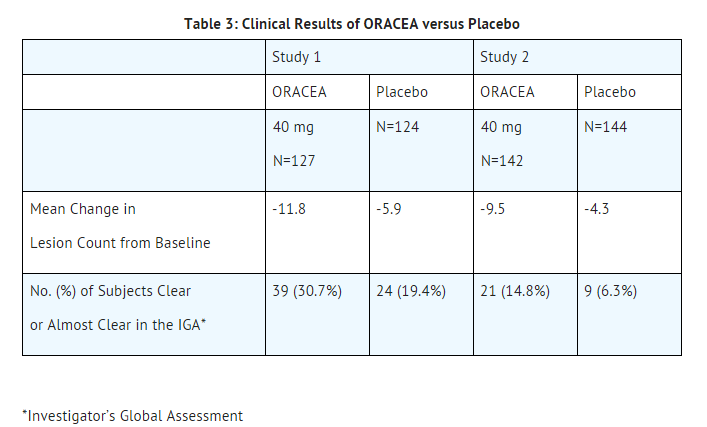
- Subjects treated with ORACEA did not demonstrate significant improvement in erythema when compared to those treated with placebo.
How Supplied
- ORACEA (beige opaque capsule imprinted with “GLD 40”) containing doxycycline, USP in an amount equivalent to 40 mg of anhydrous doxycycline. Bottle of 30 (NDC 0299-3822-30).
Storage
- All products are to be stored at controlled room temperatures of 15°C - 30°C (59°F - 86°F) and dispensed in tight, light-resistant containers (USP).
- Keep out of reach of children
Images
Drug Images
{{#ask: Page Name::Doxycycline (oral) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Doxycycline (oral) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
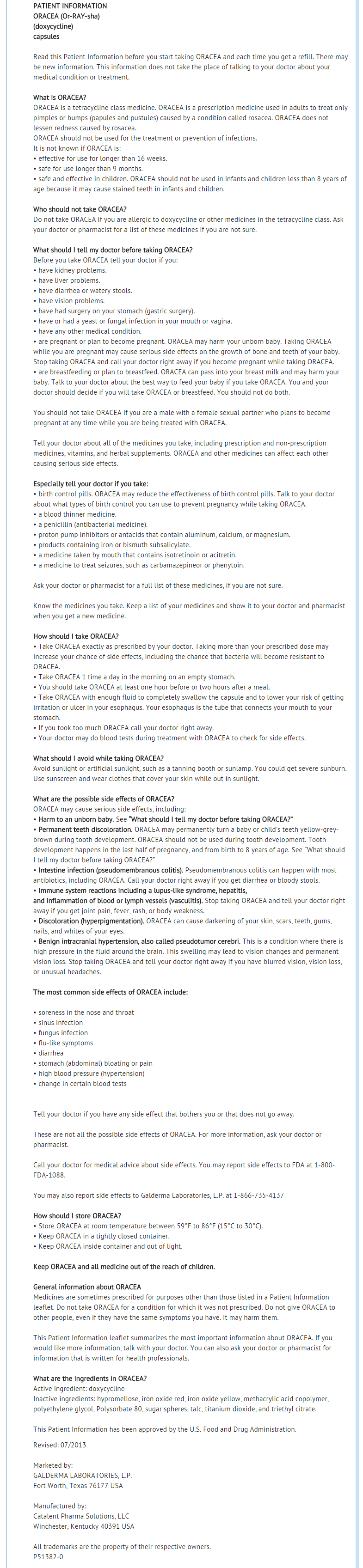
Patient Counseling Information
Patients taking ORACEA Capsules 40 mg should receive the following information and instructions:
- It is recommended that ORACEA not be used by individuals of either gender who are attempting to conceive a child
- It is recommended that ORACEA not be used by pregnant or breast feeding women.
- Patients should be advised that pseudomembranous colitis can occur with doxycycline therapy. If patients develop watery or bloody stools, they should seek medical attention.
- Patients should be advised that pseudotumor cerebri can occur with doxycycline therapy. If patients experience headache or blurred vision they should seek medical attention.
- Photosensitivity manifested by an exaggerated sunburn reaction has been observed in some individuals taking tetracyclines, including doxycycline. Patients should minimize or avoid exposure to natural or artificial sunlight (tanning beds or UVA/B treatment) while using doxycycline. If patients need to be outdoors while using doxycycline, they should wear loose-fitting clothes that protect skin from sun exposure and discuss other sun protection measures with their physician. Treatment should be discontinued at the first evidence of sunburn.
- Concurrent use of doxycycline may render oral contraceptives less effective.
- Autoimmune syndromes, including drug-induced lupus-like syndrome, autoimmune hepatitis, vasculitis and serum sickness have been observed with tetracycline-class drugs, including doxycycline. Symptoms may be manifested by arthralgia, fever, rash and malaise. Patients who experience such symptoms should be cautioned to stop the drug immediately and seek medical help.
- Patients should be counseled about discoloration of skin, scars, teeth or gums that can arise from doxycycline therapy.
- Take ORACEA exactly as directed. Increasing doses beyond 40 mg every morning may increase the likelihood that bacteria will develop resistance and will not be treatable by other antibacterial drugs in the future.
Precautions with Alcohol
- Alcohol- doxycycline interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
ORACEA
Look-Alike Drug Names
There is limited information regarding Doxycycline (oral) Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Page Name=Doxycycline (oral)
|Pill Name=No image.jpg
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Label Page=Doxycycline (oral) |Label Name=ORACEA pic01.jpg
}}
{{#subobject:
|Label Page=Doxycycline (oral) |Label Name=Doxycycline ingredients and appearance.png
}}