Mitral regurgitation echocardiography: Difference between revisions
No edit summary |
|||
| Line 12: | Line 12: | ||
[[Image:Mitralinsuff TEE.jpg|400px|transesophageal echocardiogram of mitral valve prolapse]] | [[Image:Mitralinsuff TEE.jpg|400px|transesophageal echocardiogram of mitral valve prolapse]] | ||
==ACC/AHA Guidelines- Indications for Transthoracic Echocardiography for Mitral Regurgitation (DO NOT EDIT) <ref name="pmid18848134">{{cite journal| author=Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Faxon DP, Freed MD et al.| title=2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. | journal=J Am Coll Cardiol | year= 2008 | volume= 52 | issue= 13 | pages= e1-142 | pmid=18848134 | doi=10.1016/j.jacc.2008.05.007 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18848134 }} </ref>== | |||
{{cquote| | |||
class i | class i | ||
| Line 51: | Line 47: | ||
class iii | class iii | ||
1. Transesophageal echocardiography is not indicated for routine follow-up or surveillance of asymptomatic patients with native valve MR. (Level of Evidence: C) | 1. Transesophageal echocardiography is not indicated for routine follow-up or surveillance of asymptomatic patients with native valve MR. (Level of Evidence: C)}} | ||
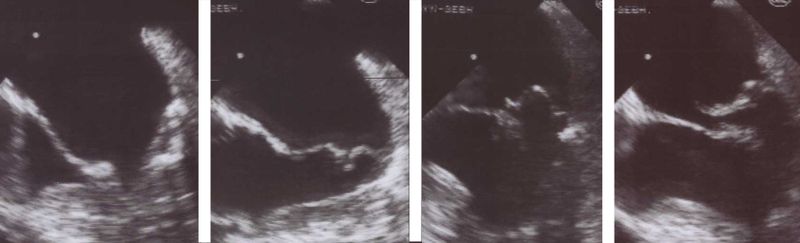
==Aetiology and Morphological Features in 2-D Echocardiography== | ==Aetiology and Morphological Features in 2-D Echocardiography== | ||
Revision as of 18:24, 23 September 2011
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Varun Kumar, M.B.B.S.; Lakshmi Gopalakrishnan, M.B.B.S.
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
The echocardiogram is commonly used to confirm the diagnosis of mitral regurgitation. Color doppler flow on the transthoracic echocardiogram (TTE) will reveal a jet of blood flowing from the left ventricle into the left atrium during ventricular systole.
Because of the inability in getting accurate images of the left atrium and the pulmonary veins on the transthoracic echocardiogram, a transesophageal echocardiogram may be necessary to determine the severity of the mitral regurgitation in some cases.
Factors that suggest severe mitral regurgitation on echocardiography include systolic reversal of flow in the pulmonary veins and filling of the entire left atrial cavity by the regurgitant jet of MR.
ACC/AHA Guidelines- Indications for Transthoracic Echocardiography for Mitral Regurgitation (DO NOT EDIT) [1]
| “ |
class i 1 Transthoracic echocardiography is indicated for baseline evaluation of LV size and function, RV and left atrial size, pulmonary artery pressure, and severity of MR (Table 4) in any patient suspected of having MR. (Level of Evidence: C) 2 Transthoracic echocardiography is indicated for delineation of the mechanism of MR. (Level of Evidence: B) 3 Transthoracic echocardiography is indicated for annual or semiannual surveillance of LV function (estimated by ejection fraction and end-systolic dimension) in asymptomatic patients with moderate to severe MR. (Level of Evidence: C) 4 Transthoracic echocardiography is indicated in patients with MR to evaluate the MV apparatus and LV function after a change in signs or symptoms. (Level of Evidence: C) 5 Transthoracic echocardiography is indicated to evaluate LV size and function and MV hemodynamics in the initial evaluation after MV replacement or MV repair. (Level of Evidence: C) class iia 1. Exercise Doppler echocardiography is reasonable in asymptomatic patients with severe MR to assess exercise tolerance and the effects of exercise on pulmonary artery pressure and MR severity. (Level of Evidence: C) class iii 1. Transthoracic echocardiography is not indicated for routine follow-up evaluation of asymptomatic patients with mild MR and normal LV size and systolic function. (Level of Evidence: C) An initial comprehensive 2D, Doppler echocardiogram is indispensable in the management of the patient with MR. The echocardiogram provides a baseline estimation of LV and left atrial size, an estimation of LV ejection fraction, and approximation of the severity of regurgitation (2). Quantification of the severity of MR (Table 4) (27) is strongly recommended ( [27] , [541] , [545] and [546] ). In the majority of patients, an estimate of pulmonary artery pressure can be obtained from the TR peak velocity (547). Changes from these baseline values are subsequently used to guide the timing of MV surgery. The blood pressure at the time of each study should be documented, because the afterload on the ventricle will affect the measured severity of the MR. The initial transthoracic echocardiogram should disclose the anatomic cause of the MR. A central color flow jet of MR with a structurally normal MV apparatus suggests the presence of functional MR, which may be due to annular dilatation from LV dilatation or tethering of the posterior leaflet because of regional LV dysfunction in patients with ischemic heart disease. An eccentric color flow jet of MR with abnormalities of the MV apparatus indicates organic MR. In patients with organic MR, the echocardiogram should assess the presence of calcium in the annulus or leaflets, the redundancy of the valve leaflets, and the MV leaflet involved (anterior leaflet, posterior leaflet, or bileaflet). These factors will help determine the feasibility of valve repair if surgery is contemplated. The system proposed by Carpentier (548) allows the echocardiographer to focus on the anatomic and physiologic characteristics of the valve that aid the surgeon in planning the repair. The valve dysfunction is described on the basis of the motion of the free edge of the leaflet relative to the plane of the annulus: type I, normal; type II, increased, as in MVP; type IIIA, restricted during systole and diastole, and type IIIB, restricted during systole. The diagnosis of severe MR should be made by correlating the findings on physical examination with the findings from a comprehensive 2D, Doppler echocardiogram. Multiple parameters from the Doppler examination should be used to diagnose severe MR (Table 4) (27), including the color flow jet width and area, the intensity of the continuous-wave Doppler signal, the pulmonary venous flow contour, the peak early mitral inflow velocity, and quantitative measures of effective orifice area and regurgitation volume (2). In addition, there should be enlargement of the left ventricle and left atrium in chronic severe MR. Abnormalities of the MV apparatus are often present if there is severe MR, but ischemic LV dysfunction may also result in severe MR. If a discrepancy is present, or if the patient has poor windows on transthoracic echocardiography, then further evaluation of the severity of MR is required, including cardiac catheterization, magnetic resonance imaging, or transesophageal echocardiography. 3.6.3.4. Indications for Transesophageal Echocardiography (See Also Section 8.1.4.) class i 1 Preoperative or intraoperative transesophageal echocardiography is indicated to establish the anatomic basis for severe MR in patients in whom surgery is recommended to assess feasibility of repair and to guide repair. (Level of Evidence: B) 2 Transesophageal echocardiography is indicated for evaluation of MR patients in whom transthoracic echocardiography provides nondiagnostic information regarding severity of MR, mechanism of MR, and/or status of LV function. (Level of Evidence: B) class iia 1. Preoperative transesophageal echocardiography is reasonable in asymptomatic patients with severe MR who are considered for surgery to assess feasibility of repair. (Level of Evidence: C) class iii 1. Transesophageal echocardiography is not indicated for routine follow-up or surveillance of asymptomatic patients with native valve MR. (Level of Evidence: C) |
” |
Aetiology and Morphological Features in 2-D Echocardiography
Rheumatic Mitral Regurgitation
In rheumatic mitral regurgitation, there is some degree of commissural fusion and thickening of the tips visible in 2 dimensional echocardiography. The movement of the valve leaflets is restricted.
Myxomatous Mitral Valve
The leaflets and chordae are thick and reduntant. Reduced tensile strength leads to progressive elongation or rupture of chordae. Ruptured chordae appear as flail segments. To diagnose mitral valve prolapse, the following criteria should be fulfilled during echocardiography - Movement of any part of either leaflet more than 2mm behind the annular plane in parasternal long axis view and movement of point of co-aptation behind the annular plane in apical 4 chamber view.
Annular Calcification
Mitral annulus is usually smaller in systole. The increased rigidity due to annular calcification impairs contraction. In 2D- echocardiography, there is increased echogenicity on the LV side immediately adjacent to the attachment of the posterior mitral valve leaflet. Region of anterior mitral leaflet is only rarely involved. This is common in elderly subjects and younger ones with chronic renal failure and hypertension.
Ischaemic Mitral Regurgitation
Mitral regurgitation can occur in ischemia as a result of regional left ventricular dysfunction with abnormal contraction of papillary muscle or underlying ventricular wall. Myocardial infarction can result in MR at rest while if the underlying cause is ischemia the MR may be intermittent. The echocardiogram is characterized by restricted valve leaflet motion and tenting of mitral valve in systole.
Papillary Muscle Rupture
This is usually a complication of myocardial infarction. If entire papillary muscle is disconnected from the left ventricle severe MR results and few survive. Partial rupture is more common.
Functional Mitral Regurgitation
Functional MR results due to LV dilatation and systolic dysfunction in those with a structurally normal mitral valve apparatus.
 |
- Mitral Ring Dehiscence Post Repair With Severe Mitral Regurgitation
<googlevideo>7246533519972889950&hl=en</googlevideo>
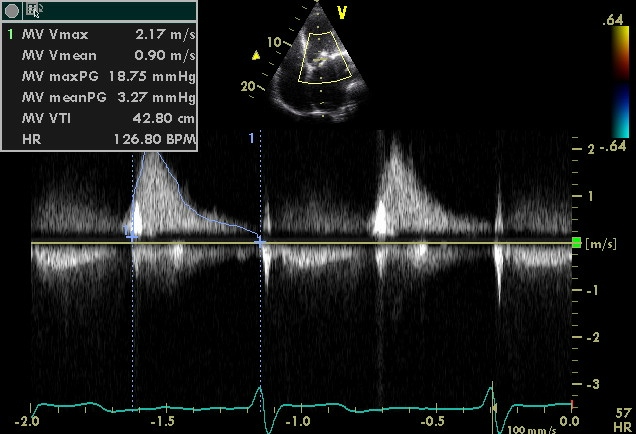
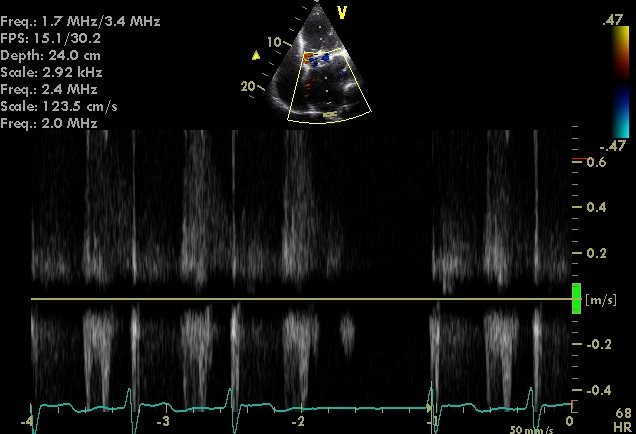
- Severe Mitral Regurgitation From Ring Dehiscence Pulmonary Vein Pulsed Wave Doppler
- Severe Mitral Regurgitation Pulmonary Vein Pulsed Wave Doppler
References
- ↑ Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Faxon DP, Freed MD; et al. (2008). "2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". J Am Coll Cardiol. 52 (13): e1–142. doi:10.1016/j.jacc.2008.05.007. PMID 18848134.