Sandbox:Cherry: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{Irritable bowel syndrome}} | |||
{{CMG}}; {{AE}} | |||
==Overview== | |||
The exact pathogenesis of [disease name] is not fully understood. | |||
OR | |||
It is thought that [disease name] is the result of / is mediated by / is produced by / is caused by either [hypothesis 1], [hypothesis 2], or [hypothesis 3]. | |||
OR | |||
[Pathogen name] is usually transmitted via the [transmission route] route to the human host. | |||
OR | |||
Following transmission/ingestion, the [pathogen] uses the [entry site] to invade the [cell name] cell. | |||
OR | |||
[Disease or malignancy name] arises from [cell name]s, which are [cell type] cells that are normally involved in [function of cells]. | |||
OR | |||
The progression to [disease name] usually involves the [molecular pathway]. | |||
OR | |||
The pathophysiology of [disease/malignancy] depends on the histological subtype. | |||
==Pathophysiology== | |||
===Pathogenesis=== | |||
The exact pathogenesis of Irritable Bowel Syndrome (IBS) is uncertain. It is understood that IBS is caused by the interaction of various factors: | |||
*'''Gastrointestinal motor abnormalities''' | |||
**IBS is referred to as ‘spastic colon’ due to changes in colonic motor function. | |||
**Manometry recordings from the transverse, descending and sigmoid colon have shown that spastic colon leads to changed patterns of colonic and small intestinal motor function such as increased frequency and irregularity of luminal contractions.<ref name="pmid8789897">{{cite journal |vauthors=Schmidt T, Hackelsberger N, Widmer R, Meisel C, Pfeiffer A, Kaess H |title=Ambulatory 24-hour jejunal motility in diarrhea-predominant irritable bowel syndrome |journal=Scand. J. Gastroenterol. |volume=31 |issue=6 |pages=581–9 |year=1996 |pmid=8789897 |doi= |url=}}</ref><ref name="pmid2865504">{{cite journal |vauthors=Kumar D, Wingate DL |title=The irritable bowel syndrome: a paroxysmal motor disorder |journal=Lancet |volume=2 |issue=8462 |pages=973–7 |year=1985 |pmid=2865504 |doi= |url=}}</ref><ref name="pmid11215731">{{cite journal |vauthors=Simrén M, Castedal M, Svedlund J, Abrahamsson H, Björnsson E |title=Abnormal propagation pattern of duodenal pressure waves in the irritable bowel syndrome (IBS) [correction of (IBD)] |journal=Dig. Dis. Sci. |volume=45 |issue=11 |pages=2151–61 |year=2000 |pmid=11215731 |doi= |url=}}</ref> | |||
**Peak amplitude of high-amplitude propagating contractions (HAPCs) in diarrhea-prone IBS patients is higher, compared to healthy subjects.<ref name="pmid18456567">{{cite journal |vauthors=Camilleri M, McKinzie S, Busciglio I, Low PA, Sweetser S, Burton D, Baxter K, Ryks M, Zinsmeister AR |title=Prospective study of motor, sensory, psychologic, and autonomic functions in patients with irritable bowel syndrome |journal=Clin. Gastroenterol. Hepatol. |volume=6 |issue=7 |pages=772–81 |year=2008 |pmid=18456567 |pmc=2495078 |doi=10.1016/j.cgh.2008.02.060 |url=}}</ref><ref name="pmid3569764">{{cite journal |vauthors=Kellow JE, Phillips SF |title=Altered small bowel motility in irritable bowel syndrome is correlated with symptoms |journal=Gastroenterology |volume=92 |issue=6 |pages=1885–93 |year=1987 |pmid=3569764 |doi= |url=}}</ref> | |||
**Diarrhea prone IBS patients have increased responses to ingestion, CRH(Corticotropin releasing hormone)<ref name="pmid7379673">{{cite journal |vauthors=Whitehead WE, Engel BT, Schuster MM |title=Irritable bowel syndrome: physiological and psychological differences between diarrhea-predominant and constipation-predominant patients |journal=Dig. Dis. Sci. |volume=25 |issue=6 |pages=404–13 |year=1980 |pmid=7379673 |doi= |url=}}</ref><ref name="pmid9691924">{{cite journal |vauthors=Fukudo S, Nomura T, Hongo M |title=Impact of corticotropin-releasing hormone on gastrointestinal motility and adrenocorticotropic hormone in normal controls and patients with irritable bowel syndrome |journal=Gut |volume=42 |issue=6 |pages=845–9 |year=1998 |pmid=9691924 |pmc=1727153 |doi= |url=}}</ref>, CCK(cholecystokinin)<ref name="pmid11374689">{{cite journal |vauthors=Chey WY, Jin HO, Lee MH, Sun SW, Lee KY |title=Colonic motility abnormality in patients with irritable bowel syndrome exhibiting abdominal pain and diarrhea |journal=Am. J. Gastroenterol. |volume=96 |issue=5 |pages=1499–506 |year=2001 |pmid=11374689 |doi=10.1111/j.1572-0241.2001.03804.x |url=}}</ref> and present with abdominal discomfort and accelerated transit through the colon. | |||
**On the other hand, constipation prone IBS patients show fewer HAPCs, delayed transit through the colon and decreased motility.<ref name="pmid18456567">{{cite journal |vauthors=Camilleri M, McKinzie S, Busciglio I, Low PA, Sweetser S, Burton D, Baxter K, Ryks M, Zinsmeister AR |title=Prospective study of motor, sensory, psychologic, and autonomic functions in patients with irritable bowel syndrome |journal=Clin. Gastroenterol. Hepatol. |volume=6 |issue=7 |pages=772–81 |year=2008 |pmid=18456567 |pmc=2495078 |doi=10.1016/j.cgh.2008.02.060 |url=}}</ref> | |||
**It has been demonstrated that more than 90% of HAPCs are associated with abdominal pain.<ref name="pmid11374689">{{cite journal |vauthors=Chey WY, Jin HO, Lee MH, Sun SW, Lee KY |title=Colonic motility abnormality in patients with irritable bowel syndrome exhibiting abdominal pain and diarrhea |journal=Am. J. Gastroenterol. |volume=96 |issue=5 |pages=1499–506 |year=2001 |pmid=11374689 |doi=10.1111/j.1572-0241.2001.03804.x |url=}}</ref> | |||
*'''CNS dysregulation''' | |||
** The conceptualization of IBS being a brain gut disorder is reinforced by the following: | |||
*** Epidemiological studies suggest that IBS occurs in individuals who have experienced childhood trauma, with symptom exacerbation occurring in patients with emotional disturbances or stress.<ref name="pmid27061107">{{cite journal |vauthors=Park SH, Videlock EJ, Shih W, Presson AP, Mayer EA, Chang L |title=Adverse childhood experiences are associated with irritable bowel syndrome and gastrointestinal symptom severity |journal=Neurogastroenterol. Motil. |volume=28 |issue=8 |pages=1252–60 |year=2016 |pmid=27061107 |pmc=4956522 |doi=10.1111/nmo.12826 |url=}}</ref> | |||
*** Traumatic experiences before the age of 18 can directly shape adult connectivity in the executive control network. The effects on structures such as the insula, anterior cingulate cortex and the thalamus have been implicated in the pathophysiology of central pain amplification.<ref name="pmid25003944">{{cite journal |vauthors=Gupta A, Kilpatrick L, Labus J, Tillisch K, Braun A, Hong JY, Ashe-McNalley C, Naliboff B, Mayer EA |title=Early adverse life events and resting state neural networks in patients with chronic abdominal pain: evidence for sex differences |journal=Psychosom Med |volume=76 |issue=6 |pages=404–12 |year=2014 |pmid=25003944 |pmc=4113723 |doi=10.1097/PSY.0000000000000089 |url=}}</ref> | |||
*** IBS has been found to have a high association with pre-existing psychiatric and psychological conditions like anxiety and depression.<ref name="pmid27144627">{{cite journal |vauthors=Mearin F, Lacy BE, Chang L, Chey WD, Lembo AJ, Simren M, Spiller R |title=Bowel Disorders |journal=Gastroenterology |volume= |issue= |pages= |year=2016 |pmid=27144627 |doi=10.1053/j.gastro.2016.02.031 |url=}}</ref> However, studies have shown that even when patients are not anxious or depressed, the dorsolateral prefrontal cortex activity is reduced, pointing directly towards CNS dysfunction and increased susceptibility to stressors.<ref name="pmid22108191">{{cite journal |vauthors=Larsson MB, Tillisch K, Craig AD, Engström M, Labus J, Naliboff B, Lundberg P, Ström M, Mayer EA, Walter SA |title=Brain responses to visceral stimuli reflect visceral sensitivity thresholds in patients with irritable bowel syndrome |journal=Gastroenterology |volume=142 |issue=3 |pages=463–472.e3 |year=2012 |pmid=22108191 |pmc=3288538 |doi=10.1053/j.gastro.2011.11.022 |url=}}</ref> | |||
*** Psychological therapies that act on cerebral cortical sites and antidepressants have proven to be one of the mainstays of therapy for patients. The role of probiotics in modifying signal processing in the brain also proves that IBS is a brain gut disorder. <ref name="pmid23474283">{{cite journal |vauthors=Tillisch K, Labus J, Kilpatrick L, Jiang Z, Stains J, Ebrat B, Guyonnet D, Legrain-Raspaud S, Trotin B, Naliboff B, Mayer EA |title=Consumption of fermented milk product with probiotic modulates brain activity |journal=Gastroenterology |volume=144 |issue=7 |pages=1394–401, 1401.e1–4 |year=2013 |pmid=23474283 |pmc=3839572 |doi=10.1053/j.gastro.2013.02.043 |url=}}</ref> | |||
*** Studies using advanced brain imaging techniques have analyzed differences in brain activity and have helped us appreciate that the mid-cingulate cortex (responsible for attention processes and responses) and the prefrontal cortex(responsible for vigilance and alertness of the human brain) are involved in IBS. <ref name="pmid25003944" /> | |||
*** Modulation of the mid-cingulate cortex is associated with alterations in the subjective sensations of pain whereas prefrontal cortex modulation may lead to increased perception of visceral pain.<ref name="pmid25003944">{{cite journal |vauthors=Gupta A, Kilpatrick L, Labus J, Tillisch K, Braun A, Hong JY, Ashe-McNalley C, Naliboff B, Mayer EA |title=Early adverse life events and resting state neural networks in patients with chronic abdominal pain: evidence for sex differences |journal=Psychosom Med |volume=76 |issue=6 |pages=404–12 |year=2014 |pmid=25003944 |pmc=4113723 |doi=10.1097/PSY.0000000000000089 |url=}}</ref> | |||
*** Patients with IBS have aberrant processing of central information,<ref name="pmid23864686">{{cite journal |vauthors=Hong JY, Kilpatrick LA, Labus J, Gupta A, Jiang Z, Ashe-McNalley C, Stains J, Heendeniya N, Ebrat B, Smith S, Tillisch K, Naliboff B, Mayer EA |title=Patients with chronic visceral pain show sex-related alterations in intrinsic oscillations of the resting brain |journal=J. Neurosci. |volume=33 |issue=29 |pages=11994–2002 |year=2013 |pmid=23864686 |pmc=3713732 |doi=10.1523/JNEUROSCI.5733-12.2013 |url=}}</ref> with decreased feedback on the emotional arousal network that controls the autonomic modulation of gastrointestinal function.<ref name="pmid20003075">{{cite journal |vauthors=Hall GB, Kamath MV, Collins S, Ganguli S, Spaziani R, Miranda KL, Bayati A, Bienenstock J |title=Heightened central affective response to visceral sensations of pain and discomfort in IBS |journal=Neurogastroenterol. Motil. |volume=22 |issue=3 |pages=276–e80 |year=2010 |pmid=20003075 |doi=10.1111/j.1365-2982.2009.01436.x |url=}}</ref>These have been seen as irregularities on diffusion tensor imaging<ref name="pmid23721972">{{cite journal |vauthors=Ellingson BM, Mayer E, Harris RJ, Ashe-McNally C, Naliboff BD, Labus JS, Tillisch K |title=Diffusion tensor imaging detects microstructural reorganization in the brain associated with chronic irritable bowel syndrome |journal=Pain |volume=154 |issue=9 |pages=1528–41 |year=2013 |pmid=23721972 |pmc=3758125 |doi=10.1016/j.pain.2013.04.010 |url=}}</ref> in the white matter of the brain. | |||
*** Rectal balloon distension in patients has shown the increased involvement of regions of the brain associated with attentional and behavioral responses to the arrival of such stimuli.<ref name="pmid20600024">{{cite journal |vauthors=Elsenbruch S, Rosenberger C, Bingel U, Forsting M, Schedlowski M, Gizewski ER |title=Patients with irritable bowel syndrome have altered emotional modulation of neural responses to visceral stimuli |journal=Gastroenterology |volume=139 |issue=4 |pages=1310–9 |year=2010 |pmid=20600024 |doi=10.1053/j.gastro.2010.06.054 |url=}}</ref><ref name="pmid19651629">{{cite journal |vauthors=Elsenbruch S, Rosenberger C, Enck P, Forsting M, Schedlowski M, Gizewski ER |title=Affective disturbances modulate the neural processing of visceral pain stimuli in irritable bowel syndrome: an fMRI study |journal=Gut |volume=59 |issue=4 |pages=489–95 |year=2010 |pmid=19651629 |doi=10.1136/gut.2008.175000 |url=}}</ref><ref name="pmid22108191">{{cite journal |vauthors=Larsson MB, Tillisch K, Craig AD, Engström M, Labus J, Naliboff B, Lundberg P, Ström M, Mayer EA, Walter SA |title=Brain responses to visceral stimuli reflect visceral sensitivity thresholds in patients with irritable bowel syndrome |journal=Gastroenterology |volume=142 |issue=3 |pages=463–472.e3 |year=2012 |pmid=22108191 |pmc=3288538 |doi=10.1053/j.gastro.2011.11.022 |url=}}</ref> | |||
* '''Visceral hypersensitivity''' | |||
** Visceral hypersensitivity is an important factor in the pathogenesis of pain perception in IBS patients<ref name="pmid2323511">{{cite journal |vauthors=Whitehead WE, Holtkotter B, Enck P, Hoelzl R, Holmes KD, Anthony J, Shabsin HS, Schuster MM |title=Tolerance for rectosigmoid distention in irritable bowel syndrome |journal=Gastroenterology |volume=98 |issue=5 Pt 1 |pages=1187–92 |year=1990 |pmid=2323511 |doi= |url=}}</ref>. IBS is associated with a decreased threshold for perception of visceral stimuli<ref name="pmid18456567">{{cite journal |vauthors=Camilleri M, McKinzie S, Busciglio I, Low PA, Sweetser S, Burton D, Baxter K, Ryks M, Zinsmeister AR |title=Prospective study of motor, sensory, psychologic, and autonomic functions in patients with irritable bowel syndrome |journal=Clin. Gastroenterol. Hepatol. |volume=6 |issue=7 |pages=772–81 |year=2008 |pmid=18456567 |pmc=2495078 |doi=10.1016/j.cgh.2008.02.060 |url=}}</ref><ref name="pmid21537962">{{cite journal |vauthors=Barbara G, Cremon C, De Giorgio R, Dothel G, Zecchi L, Bellacosa L, Carini G, Stanghellini V, Corinaldesi R |title=Mechanisms underlying visceral hypersensitivity in irritable bowel syndrome |journal=Curr Gastroenterol Rep |volume=13 |issue=4 |pages=308–15 |year=2011 |pmid=21537962 |doi=10.1007/s11894-011-0195-7 |url=}}</ref> (i.e. visceral hypersensitivity). | |||
** Studies in IBS patients have shown that rectal balloon inflation produces painful and non-painful sensations at lower volumes as compared to healthy controls, suggesting the presence of afferent pathway disturbances in visceral innervation<ref name="pmid7797041">{{cite journal |vauthors=Mertz H, Naliboff B, Munakata J, Niazi N, Mayer EA |title=Altered rectal perception is a biological marker of patients with irritable bowel syndrome |journal=Gastroenterology |volume=109 |issue=1 |pages=40–52 |year=1995 |pmid=7797041 |doi= |url=}}</ref><ref name="pmid2338274">{{cite journal |vauthors=Prior A, Maxton DG, Whorwell PJ |title=Anorectal manometry in irritable bowel syndrome: differences between diarrhoea and constipation predominant subjects |journal=Gut |volume=31 |issue=4 |pages=458–62 |year=1990 |pmid=2338274 |pmc=1378424 |doi= |url=}}</ref><ref name="pmid17919487">{{cite journal |vauthors=Posserud I, Syrous A, Lindström L, Tack J, Abrahamsson H, Simrén M |title=Altered rectal perception in irritable bowel syndrome is associated with symptom severity |journal=Gastroenterology |volume=133 |issue=4 |pages=1113–23 |year=2007 |pmid=17919487 |doi=10.1053/j.gastro.2007.07.024 |url=}}</ref><ref name="pmid12055583">{{cite journal |vauthors=Bouin M, Plourde V, Boivin M, Riberdy M, Lupien F, Laganière M, Verrier P, Poitras P |title=Rectal distention testing in patients with irritable bowel syndrome: sensitivity, specificity, and predictive values of pain sensory thresholds |journal=Gastroenterology |volume=122 |issue=7 |pages=1771–7 |year=2002 |pmid=12055583 |doi= |url=}}</ref>. Many factors contribute to visceral hyperalgesia(i.e increased sensitivity of the intestines to normal sensations): | |||
*** Spinal hyperexcitability due to activation of an N-methyl D aspartate(NMDA) receptor, Nitric oxide and possibly other neurotransmitters. | |||
*** Activation of specific gastrointestinal mediators like kinins and serotonin that lead to afferent nerve fiber sensitization. | |||
*** Central (brainstem and cortical) modulation with increased activation of anterior circulate cortex, thalamus and insula, involved in processing of pain, translating into long term hypersensitivity due to neuroplasticity, causing semipermanent changes in the neural response to all kinds of visceral stimulation. These findings have been proven by brain imaging studies. (e.g. functional magnetic resonance imaging, positron emission tomography'')<ref name="pmid21537962">{{cite journal |vauthors=Barbara G, Cremon C, De Giorgio R, Dothel G, Zecchi L, Bellacosa L, Carini G, Stanghellini V, Corinaldesi R |title=Mechanisms underlying visceral hypersensitivity in irritable bowel syndrome |journal=Curr Gastroenterol Rep |volume=13 |issue=4 |pages=308–15 |year=2011 |pmid=21537962 |doi=10.1007/s11894-011-0195-7 |url=}}</ref><ref name="pmid10784583">{{cite journal |vauthors=Mertz H, Morgan V, Tanner G, Pickens D, Price R, Shyr Y, Kessler R |title=Regional cerebral activation in irritable bowel syndrome and control subjects with painful and nonpainful rectal distention |journal=Gastroenterology |volume=118 |issue=5 |pages=842–8 |year=2000 |pmid=10784583 |doi= |url=}}</ref> '' | |||
*** Recruitment of peripheral silent nociceptors causing increased end organ sensitivity due to hormonal or immune activation<ref name="pmid21537962">{{cite journal |vauthors=Barbara G, Cremon C, De Giorgio R, Dothel G, Zecchi L, Bellacosa L, Carini G, Stanghellini V, Corinaldesi R |title=Mechanisms underlying visceral hypersensitivity in irritable bowel syndrome |journal=Curr Gastroenterol Rep |volume=13 |issue=4 |pages=308–15 |year=2011 |pmid=21537962 |doi=10.1007/s11894-011-0195-7 |url=}}</ref>. | |||
* '''Immune activation and mucosal inflammation''' | |||
** The high prevalence of IBS in patients with history of inflammatory bowel disease, celiac disease or microscopic colitis points towards the fact that immune activation and mucosal inflammation play an important role in the pathogenesis of IBS.<ref name="pmid19997094">{{cite journal |vauthors=Coëffier M, Gloro R, Boukhettala N, Aziz M, Lecleire S, Vandaele N, Antonietti M, Savoye G, Bôle-Feysot C, Déchelotte P, Reimund JM, Ducrotté P |title=Increased proteasome-mediated degradation of occludin in irritable bowel syndrome |journal=Am. J. Gastroenterol. |volume=105 |issue=5 |pages=1181–8 |year=2010 |pmid=19997094 |doi=10.1038/ajg.2009.700 |url=}}</ref><ref name="pmid12055584">{{cite journal |vauthors=Chadwick VS, Chen W, Shu D, Paulus B, Bethwaite P, Tie A, Wilson I |title=Activation of the mucosal immune system in irritable bowel syndrome |journal=Gastroenterology |volume=122 |issue=7 |pages=1778–83 |year=2002 |pmid=12055584 |doi= |url=}}</ref><ref name="pmid17383420">{{cite journal |vauthors=Liebregts T, Adam B, Bredack C, Röth A, Heinzel S, Lester S, Downie-Doyle S, Smith E, Drew P, Talley NJ, Holtmann G |title=Immune activation in patients with irritable bowel syndrome |journal=Gastroenterology |volume=132 |issue=3 |pages=913–20 |year=2007 |pmid=17383420 |doi=10.1053/j.gastro.2007.01.046 |url=}}</ref><ref name="pmid12454854">{{cite journal |vauthors=Törnblom H, Lindberg G, Nyberg B, Veress B |title=Full-thickness biopsy of the jejunum reveals inflammation and enteric neuropathy in irritable bowel syndrome |journal=Gastroenterology |volume=123 |issue=6 |pages=1972–9 |year=2002 |pmid=12454854 |doi=10.1053/gast.2002.37059 |url=}}</ref><ref name="pmid17005763">{{cite journal |vauthors=Guilarte M, Santos J, de Torres I, Alonso C, Vicario M, Ramos L, Martínez C, Casellas F, Saperas E, Malagelada JR |title=Diarrhoea-predominant IBS patients show mast cell activation and hyperplasia in the jejunum |journal=Gut |volume=56 |issue=2 |pages=203–9 |year=2007 |pmid=17005763 |pmc=1856785 |doi=10.1136/gut.2006.100594 |url=}}</ref><ref name="pmid14988823">{{cite journal |vauthors=Barbara G, Stanghellini V, De Giorgio R, Cremon C, Cottrell GS, Santini D, Pasquinelli G, Morselli-Labate AM, Grady EF, Bunnett NW, Collins SM, Corinaldesi R |title=Activated mast cells in proximity to colonic nerves correlate with abdominal pain in irritable bowel syndrome |journal=Gastroenterology |volume=126 |issue=3 |pages=693–702 |year=2004 |pmid=14988823 |doi= |url=}}</ref><ref name="pmid17383420">{{cite journal |vauthors=Liebregts T, Adam B, Bredack C, Röth A, Heinzel S, Lester S, Downie-Doyle S, Smith E, Drew P, Talley NJ, Holtmann G |title=Immune activation in patients with irritable bowel syndrome |journal=Gastroenterology |volume=132 |issue=3 |pages=913–20 |year=2007 |pmid=17383420 |doi=10.1053/j.gastro.2007.01.046 |url=}}</ref> | |||
** Moreover, psychological stress can significantly impact the release of proinflammatory cytokines, thereby affecting intestinal permeability and reinforcing a functional link existing between immune activation, psychological symptoms and symptoms in patients with IBS.<ref name="pmid19997094">{{cite journal |vauthors=Coëffier M, Gloro R, Boukhettala N, Aziz M, Lecleire S, Vandaele N, Antonietti M, Savoye G, Bôle-Feysot C, Déchelotte P, Reimund JM, Ducrotté P |title=Increased proteasome-mediated degradation of occludin in irritable bowel syndrome |journal=Am. J. Gastroenterol. |volume=105 |issue=5 |pages=1181–8 |year=2010 |pmid=19997094 |doi=10.1038/ajg.2009.700 |url=}}</ref> | |||
** Patients are found to have higher mucosal counts of lymphocytes (T cells, B cells), mast cells and immune mediators such as prostanoids, proteases, cytokines and histamines. <ref name="pmid17383420">{{cite journal |vauthors=Liebregts T, Adam B, Bredack C, Röth A, Heinzel S, Lester S, Downie-Doyle S, Smith E, Drew P, Talley NJ, Holtmann G |title=Immune activation in patients with irritable bowel syndrome |journal=Gastroenterology |volume=132 |issue=3 |pages=913–20 |year=2007 |pmid=17383420 |doi=10.1053/j.gastro.2007.01.046 |url=}}</ref><ref name="pmid20427395">{{cite journal |vauthors=Marshall JK, Thabane M, Garg AX, Clark WF, Moayyedi P, Collins SM |title=Eight year prognosis of postinfectious irritable bowel syndrome following waterborne bacterial dysentery |journal=Gut |volume=59 |issue=5 |pages=605–11 |year=2010 |pmid=20427395 |doi=10.1136/gut.2009.202234 |url=}}</ref><ref name="pmid21911849">{{cite journal |vauthors=Wensaas KA, Langeland N, Hanevik K, Mørch K, Eide GE, Rortveit G |title=Irritable bowel syndrome and chronic fatigue 3 years after acute giardiasis: historic cohort study |journal=Gut |volume=61 |issue=2 |pages=214–9 |year=2012 |pmid=21911849 |doi=10.1136/gutjnl-2011-300220 |url=}}</ref><ref name="pmid19711225">{{cite journal |vauthors=Mearin F, Perelló A, Balboa A, Perona M, Sans M, Salas A, Angulo S, Lloreta J, Benasayag R, García-Gonzalez MA, Pérez-Oliveras M, Coderch J |title=Pathogenic mechanisms of postinfectious functional gastrointestinal disorders: results 3 years after gastroenteritis |journal=Scand. J. Gastroenterol. |volume=44 |issue=10 |pages=1173–85 |year=2009 |pmid=19711225 |doi=10.1080/00365520903171276 |url=}}</ref><ref name="pmid12631663">{{cite journal |vauthors=Gwee KA, Collins SM, Read NW, Rajnakova A, Deng Y, Graham JC, McKendrick MW, Moochhala SM |title=Increased rectal mucosal expression of interleukin 1beta in recently acquired post-infectious irritable bowel syndrome |journal=Gut |volume=52 |issue=4 |pages=523–6 |year=2003 |pmid=12631663 |pmc=1773606 |doi= |url=}}</ref> | |||
** '''Lymphocytes:''' | |||
*** Patients with IBS have increased B lymphocyte activation in the blood.<ref name="pmid19222763">{{cite journal |vauthors=Ohman L, Lindmark AC, Isaksson S, Posserud I, Strid H, Sjövall H, Simrén M |title=B-cell activation in patients with irritable bowel syndrome (IBS) |journal=Neurogastroenterol. Motil. |volume=21 |issue=6 |pages=644–50, e27 |year=2009 |pmid=19222763 |doi=10.1111/j.1365-2982.2009.01272.x |url=}}</ref> However, activation of humoral immunity in IBS is specific for the gastrointestinal tract<ref name="pmid25209656">{{cite journal |vauthors=Vicario M, González-Castro AM, Martínez C, Lobo B, Pigrau M, Guilarte M, de Torres I, Mosquera JL, Fortea M, Sevillano-Aguilera C, Salvo-Romero E, Alonso C, Rodiño-Janeiro BK, Söderholm JD, Azpiroz F, Santos J |title=Increased humoral immunity in the jejunum of diarrhoea-predominant irritable bowel syndrome associated with clinical manifestations |journal=Gut |volume=64 |issue=9 |pages=1379–88 |year=2015 |pmid=25209656 |doi=10.1136/gutjnl-2013-306236 |url=}}</ref> as increased numbers of lymphocytes have been found in the small intestine and colon of patients.<ref name="pmid12055584">{{cite journal |vauthors=Chadwick VS, Chen W, Shu D, Paulus B, Bethwaite P, Tie A, Wilson I |title=Activation of the mucosal immune system in irritable bowel syndrome |journal=Gastroenterology |volume=122 |issue=7 |pages=1778–83 |year=2002 |pmid=12055584 |doi= |url=}}</ref><ref name="pmid12454854">{{cite journal |vauthors=Törnblom H, Lindberg G, Nyberg B, Veress B |title=Full-thickness biopsy of the jejunum reveals inflammation and enteric neuropathy in irritable bowel syndrome |journal=Gastroenterology |volume=123 |issue=6 |pages=1972–9 |year=2002 |pmid=12454854 |doi=10.1053/gast.2002.37059 |url=}}</ref> | |||
*** In addition to this, IBS patients with diarrhea<ref name="pmid25209656">{{cite journal |vauthors=Vicario M, González-Castro AM, Martínez C, Lobo B, Pigrau M, Guilarte M, de Torres I, Mosquera JL, Fortea M, Sevillano-Aguilera C, Salvo-Romero E, Alonso C, Rodiño-Janeiro BK, Söderholm JD, Azpiroz F, Santos J |title=Increased humoral immunity in the jejunum of diarrhoea-predominant irritable bowel syndrome associated with clinical manifestations |journal=Gut |volume=64 |issue=9 |pages=1379–88 |year=2015 |pmid=25209656 |doi=10.1136/gutjnl-2013-306236 |url=}}</ref> have enhanced mucosal humoral activity, associated with activation and proliferation of B cells and immunoglobulin production, identified by microarray profiling. | |||
*** IBS patients with severe disease have an increase in lymphocyte infiltration in the myentric plexus,<ref name="pmid12454854">{{cite journal |vauthors=Törnblom H, Lindberg G, Nyberg B, Veress B |title=Full-thickness biopsy of the jejunum reveals inflammation and enteric neuropathy in irritable bowel syndrome |journal=Gastroenterology |volume=123 |issue=6 |pages=1972–9 |year=2002 |pmid=12454854 |doi=10.1053/gast.2002.37059 |url=}}</ref> in studies where full-thickness jejunal biopsies were obtained. | |||
*** Mediators released by lymphocytes include histamine, proteases and nitric oxide. The stimulation of the enteric nervous system by these mediators leads to abnormal visceral and motor responses within the gastrointestinal tract.<ref name="pmid12055584" /> | |||
*** Examination of stool in patients with diarrhea prominent IBS have high levels of serine protease activity.<ref name="pmid18924448">{{cite journal |vauthors=Bueno L |title=Protease activated receptor 2: a new target for IBS treatment |journal=Eur Rev Med Pharmacol Sci |volume=12 Suppl 1 |issue= |pages=95–102 |year=2008 |pmid=18924448 |doi= |url=}}</ref><ref name="pmid18194983">{{cite journal |vauthors=Gecse K, Róka R, Ferrier L, Leveque M, Eutamene H, Cartier C, Ait-Belgnaoui A, Rosztóczy A, Izbéki F, Fioramonti J, Wittmann T, Bueno L |title=Increased faecal serine protease activity in diarrhoeic IBS patients: a colonic lumenal factor impairing colonic permeability and sensitivity |journal=Gut |volume=57 |issue=5 |pages=591–9 |year=2008 |pmid=18194983 |doi=10.1136/gut.2007.140210 |url=}}</ref>When fecal extracts are intra colonically infused into mice, there is increased visceral pain and colonic cellular permeability. <ref name="pmid18924448" /> | |||
*** Serine protease inhibitors prevent effects mediated by high levels of serine protease. Studies have shown that mononuclear cell supernatants in the peripheral blood from healthy controls have greater inhibitory effects on colorectal sensory afferent nerve endings than in IBS patients.<ref name="pmid18194983" /><ref name="pmid18924448" /> | |||
** '''Mast cells:''' | |||
*** Studies have shown an increased number of mast cells in IBS patients in the jejunum, terminal ileum and colon.<ref name="pmid14988823">{{cite journal |vauthors=Barbara G, Stanghellini V, De Giorgio R, Cremon C, Cottrell GS, Santini D, Pasquinelli G, Morselli-Labate AM, Grady EF, Bunnett NW, Collins SM, Corinaldesi R |title=Activated mast cells in proximity to colonic nerves correlate with abdominal pain in irritable bowel syndrome |journal=Gastroenterology |volume=126 |issue=3 |pages=693–702 |year=2004 |pmid=14988823 |doi= |url=}}</ref> | |||
*** Higher numbers of activated mast cells are found in proximity to colonic nerve fibres in the mucosa of the gastrointestinal tract of IBS patients. <ref name="pmid14988823">{{cite journal |vauthors=Barbara G, Stanghellini V, De Giorgio R, Cremon C, Cottrell GS, Santini D, Pasquinelli G, Morselli-Labate AM, Grady EF, Bunnett NW, Collins SM, Corinaldesi R |title=Activated mast cells in proximity to colonic nerves correlate with abdominal pain in irritable bowel syndrome |journal=Gastroenterology |volume=126 |issue=3 |pages=693–702 |year=2004 |pmid=14988823 |doi= |url=}}</ref><ref name="pmid17005763">{{cite journal |vauthors=Guilarte M, Santos J, de Torres I, Alonso C, Vicario M, Ramos L, Martínez C, Casellas F, Saperas E, Malagelada JR |title=Diarrhoea-predominant IBS patients show mast cell activation and hyperplasia in the jejunum |journal=Gut |volume=56 |issue=2 |pages=203–9 |year=2007 |pmid=17005763 |pmc=1856785 |doi=10.1136/gut.2006.100594 |url=}}</ref> | |||
** '''Proinflammatory cytokines:''' | |||
*** Cytokines are proteinaceous mediators of the immune response. Increased levels of cytokines have been found in IBS patients.<ref name="pmid12631663">{{cite journal |vauthors=Gwee KA, Collins SM, Read NW, Rajnakova A, Deng Y, Graham JC, McKendrick MW, Moochhala SM |title=Increased rectal mucosal expression of interleukin 1beta in recently acquired post-infectious irritable bowel syndrome |journal=Gut |volume=52 |issue=4 |pages=523–6 |year=2003 |pmid=12631663 |pmc=1773606 |doi= |url=}}</ref><ref name="pmid19711225">{{cite journal |vauthors=Mearin F, Perelló A, Balboa A, Perona M, Sans M, Salas A, Angulo S, Lloreta J, Benasayag R, García-Gonzalez MA, Pérez-Oliveras M, Coderch J |title=Pathogenic mechanisms of postinfectious functional gastrointestinal disorders: results 3 years after gastroenteritis |journal=Scand. J. Gastroenterol. |volume=44 |issue=10 |pages=1173–85 |year=2009 |pmid=19711225 |doi=10.1080/00365520903171276 |url=}}</ref> | |||
*** Higher amounts of of tumor necrosis factor are produced by the peripheral blood mononuclear cells of IBS patients.<ref name="pmid16472586">{{cite journal |vauthors=Dinan TG, Quigley EM, Ahmed SM, Scully P, O'Brien S, O'Mahony L, O'Mahony S, Shanahan F, Keeling PW |title=Hypothalamic-pituitary-gut axis dysregulation in irritable bowel syndrome: plasma cytokines as a potential biomarker? |journal=Gastroenterology |volume=130 |issue=2 |pages=304–11 |year=2006 |pmid=16472586 |doi=10.1053/j.gastro.2005.11.033 |url=}}</ref><ref name="pmid17383420">{{cite journal |vauthors=Liebregts T, Adam B, Bredack C, Röth A, Heinzel S, Lester S, Downie-Doyle S, Smith E, Drew P, Talley NJ, Holtmann G |title=Immune activation in patients with irritable bowel syndrome |journal=Gastroenterology |volume=132 |issue=3 |pages=913–20 |year=2007 |pmid=17383420 |doi=10.1053/j.gastro.2007.01.046 |url=}}</ref> | |||
*** In studies conducted using supernatants from cultured peripheral blood mononuclear cells in IBS patients,the TNF antagonist infliximab has been found to block the mechanical hypersensitivity of the mouse colonic afferent nerve endings. <ref name="pmid25063707">{{cite journal |vauthors=Hughes PA, Moretta M, Lim A, Grasby DJ, Bird D, Brierley SM, Liebregts T, Adam B, Blackshaw LA, Holtmann G, Bampton P, Hoffmann P, Andrews JM, Zola H, Krumbiegel D |title=Immune derived opioidergic inhibition of viscerosensory afferents is decreased in Irritable Bowel Syndrome patients |journal=Brain Behav. Immun. |volume=42 |issue= |pages=191–203 |year=2014 |pmid=25063707 |doi=10.1016/j.bbi.2014.07.001 |url=}}</ref> | |||
*** Other cytokines such as interleukin 1β, interleukin 6, interleukin 10 and TNFα have been found in increased amounts on analysis of the supernatants from IBS patients with diarrhea, as compared to healthy controls.Increased concentration of these cytokines is directly proportional to the severity and frequency of pain.<ref name="pmid17383420">{{cite journal |vauthors=Liebregts T, Adam B, Bredack C, Röth A, Heinzel S, Lester S, Downie-Doyle S, Smith E, Drew P, Talley NJ, Holtmann G |title=Immune activation in patients with irritable bowel syndrome |journal=Gastroenterology |volume=132 |issue=3 |pages=913–20 |year=2007 |pmid=17383420 |doi=10.1053/j.gastro.2007.01.046 |url=}}</ref><ref name="pmid25063707">{{cite journal |vauthors=Hughes PA, Moretta M, Lim A, Grasby DJ, Bird D, Brierley SM, Liebregts T, Adam B, Blackshaw LA, Holtmann G, Bampton P, Hoffmann P, Andrews JM, Zola H, Krumbiegel D |title=Immune derived opioidergic inhibition of viscerosensory afferents is decreased in Irritable Bowel Syndrome patients |journal=Brain Behav. Immun. |volume=42 |issue= |pages=191–203 |year=2014 |pmid=25063707 |doi=10.1016/j.bbi.2014.07.001 |url=}}</ref><ref name="pmid16472586">{{cite journal |vauthors=Dinan TG, Quigley EM, Ahmed SM, Scully P, O'Brien S, O'Mahony L, O'Mahony S, Shanahan F, Keeling PW |title=Hypothalamic-pituitary-gut axis dysregulation in irritable bowel syndrome: plasma cytokines as a potential biomarker? |journal=Gastroenterology |volume=130 |issue=2 |pages=304–11 |year=2006 |pmid=16472586 |doi=10.1053/j.gastro.2005.11.033 |url=}}</ref> | |||
** '''Altered gut microbiota''' | |||
*** It is postulated that altered fecal microflora may be associated with IBS.<ref name="pmid20117111">{{cite journal |vauthors=Ford AC, Thabane M, Collins SM, Moayyedi P, Garg AX, Clark WF, Marshall JK |title=Prevalence of uninvestigated dyspepsia 8 years after a large waterborne outbreak of bacterial dysentery: a cohort study |journal=Gastroenterology |volume=138 |issue=5 |pages=1727–36; quiz e12 |year=2010 |pmid=20117111 |doi=10.1053/j.gastro.2010.01.043 |url=}}</ref><ref name="pmid20427395">{{cite journal |vauthors=Marshall JK, Thabane M, Garg AX, Clark WF, Moayyedi P, Collins SM |title=Eight year prognosis of postinfectious irritable bowel syndrome following waterborne bacterial dysentery |journal=Gut |volume=59 |issue=5 |pages=605–11 |year=2010 |pmid=20427395 |doi=10.1136/gut.2009.202234 |url=}}</ref> There are numerous studies that suggest that altered fecal microflora in IBS patients differ from healthy controls. <ref name="pmid17631127">{{cite journal |vauthors=Kassinen A, Krogius-Kurikka L, Mäkivuokko H, Rinttilä T, Paulin L, Corander J, Malinen E, Apajalahti J, Palva A |title=The fecal microbiota of irritable bowel syndrome patients differs significantly from that of healthy subjects |journal=Gastroenterology |volume=133 |issue=1 |pages=24–33 |year=2007 |pmid=17631127 |doi=10.1053/j.gastro.2007.04.005 |url=}}</ref><ref name="pmid15667495">{{cite journal |vauthors=Malinen E, Rinttilä T, Kajander K, Mättö J, Kassinen A, Krogius L, Saarela M, Korpela R, Palva A |title=Analysis of the fecal microbiota of irritable bowel syndrome patients and healthy controls with real-time PCR |journal=Am. J. Gastroenterol. |volume=100 |issue=2 |pages=373–82 |year=2005 |pmid=15667495 |doi=10.1111/j.1572-0241.2005.40312.x |url=}}</ref><ref name="pmid21820992">{{cite journal |vauthors=Rajilić-Stojanović M, Biagi E, Heilig HG, Kajander K, Kekkonen RA, Tims S, de Vos WM |title=Global and deep molecular analysis of microbiota signatures in fecal samples from patients with irritable bowel syndrome |journal=Gastroenterology |volume=141 |issue=5 |pages=1792–801 |year=2011 |pmid=21820992 |doi=10.1053/j.gastro.2011.07.043 |url=}}</ref><ref name="pmid21741921">{{cite journal |vauthors=Saulnier DM, Riehle K, Mistretta TA, Diaz MA, Mandal D, Raza S, Weidler EM, Qin X, Coarfa C, Milosavljevic A, Petrosino JF, Highlander S, Gibbs R, Lynch SV, Shulman RJ, Versalovic J |title=Gastrointestinal microbiome signatures of pediatric patients with irritable bowel syndrome |journal=Gastroenterology |volume=141 |issue=5 |pages=1782–91 |year=2011 |pmid=21741921 |pmc=3417828 |doi=10.1053/j.gastro.2011.06.072 |url=}}</ref><ref name="pmid22180058">{{cite journal |vauthors=Jeffery IB, O'Toole PW, Öhman L, Claesson MJ, Deane J, Quigley EM, Simrén M |title=An irritable bowel syndrome subtype defined by species-specific alterations in faecal microbiota |journal=Gut |volume=61 |issue=7 |pages=997–1006 |year=2012 |pmid=22180058 |doi=10.1136/gutjnl-2011-301501 |url=}}</ref> | |||
*** Inoculation of germ free animals with fecal microbiota from IBS patients has demonstrated increased colonic hypersensitivity, as compared to samples inoculated from healthy controls. <ref name="pmid23433203">{{cite journal |vauthors=Crouzet L, Gaultier E, Del'Homme C, Cartier C, Delmas E, Dapoigny M, Fioramonti J, Bernalier-Donadille A |title=The hypersensitivity to colonic distension of IBS patients can be transferred to rats through their fecal microbiota |journal=Neurogastroenterol. Motil. |volume=25 |issue=4 |pages=e272–82 |year=2013 |pmid=23433203 |doi=10.1111/nmo.12103 |url=}}</ref> | |||
*** Studies have also shown that the fecal microbiota in patients with post infectious IBS differs markedly from healthy controls, with decrease in the diversity of the fecal microbiome, correlated with increased numbers of CD8 and CD4RA-positive intraepithelial lymphocytes. <ref name="pmid25521822">{{cite journal |vauthors=Sundin J, Rangel I, Fuentes S, Heikamp-de Jong I, Hultgren-Hörnquist E, de Vos WM, Brummer RJ |title=Altered faecal and mucosal microbial composition in post-infectious irritable bowel syndrome patients correlates with mucosal lymphocyte phenotypes and psychological distress |journal=Aliment. Pharmacol. Ther. |volume=41 |issue=4 |pages=342–51 |year=2015 |pmid=25521822 |doi=10.1111/apt.13055 |url=}}</ref> | |||
*** IBS patients who have undergone colonoscopy, with sampling from the colon and terminal ileum have been found to have colonic spirochaetosis with a unique pathology of increased lymphoid follicles and eosinophils as compared to healthy controls.<ref name="pmid25540866">{{cite journal |vauthors=Walker MM, Talley NJ, Inganäs L, Engstrand L, Jones MP, Nyhlin H, Agréus L, Kjellstrom L, Öst Å, Andreasson A |title=Colonic spirochetosis is associated with colonic eosinophilia and irritable bowel syndrome in a general population in Sweden |journal=Hum. Pathol. |volume=46 |issue=2 |pages=277–83 |year=2015 |pmid=25540866 |doi=10.1016/j.humpath.2014.10.026 |url=}}</ref> | |||
*** IBS with diarrhea is sometimes preceded by acute enteric infections and therefore, benefit from probiotics that serve to alter metabolism and composition of the microflora.<ref name="pmid22315951">{{cite journal |vauthors=Chassard C, Dapoigny M, Scott KP, Crouzet L, Del'homme C, Marquet P, Martin JC, Pickering G, Ardid D, Eschalier A, Dubray C, Flint HJ, Bernalier-Donadille A |title=Functional dysbiosis within the gut microbiota of patients with constipated-irritable bowel syndrome |journal=Aliment. Pharmacol. Ther. |volume=35 |issue=7 |pages=828–38 |year=2012 |pmid=22315951 |doi=10.1111/j.1365-2036.2012.05007.x |url=}}</ref><ref name="pmid18806702">{{cite journal |vauthors=Camilleri M |title=Probiotics and irritable bowel syndrome: rationale, mechanisms, and efficacy |journal=J. Clin. Gastroenterol. |volume=42 Suppl 3 Pt 1 |issue= |pages=S123–5 |year=2008 |pmid=18806702 |doi=10.1097/MCG.0b013e3181574393 |url=}}</ref> Administration of probiotics in patients decreases flatulence relative to Lactobacillus.<ref name="pmid10811333">{{cite journal |vauthors=Nobaek S, Johansson ML, Molin G, Ahrné S, Jeppsson B |title=Alteration of intestinal microflora is associated with reduction in abdominal bloating and pain in patients with irritable bowel syndrome |journal=Am. J. Gastroenterol. |volume=95 |issue=5 |pages=1231–8 |year=2000 |pmid=10811333 |doi=10.1111/j.1572-0241.2000.02015.x |url=}}</ref> A probiotic yogurt containing a mixture of Bacteroides species has been shown to improve symptoms in IBS patients.<ref name="pmid22713265">{{cite journal |vauthors=Maccaferri S, Candela M, Turroni S, Centanni M, Severgnini M, Consolandi C, Cavina P, Brigidi P |title=IBS-associated phylogenetic unbalances of the intestinal microbiota are not reverted by probiotic supplementation |journal=Gut Microbes |volume=3 |issue=5 |pages=406–13 |year=2012 |pmid=22713265 |doi=10.4161/gmic.21009 |url=}}</ref> | |||
*** Studies have been conducted suggesting that the switching on of a T-helper-2 immune-cell response may cause increased susceptibility to IBS after acute GI infection.<ref name="pmid26071133">{{cite journal |vauthors=Wouters MM, Van Wanrooy S, Nguyen A, Dooley J, Aguilera-Lizarraga J, Van Brabant W, Garcia-Perez JE, Van Oudenhove L, Van Ranst M, Verhaegen J, Liston A, Boeckxstaens G |title=Psychological comorbidity increases the risk for postinfectious IBS partly by enhanced susceptibility to develop infectious gastroenteritis |journal=Gut |volume=65 |issue=8 |pages=1279–88 |year=2016 |pmid=26071133 |doi=10.1136/gutjnl-2015-309460 |url=}}</ref><ref name="pmid26729548">{{cite journal |vauthors=Riddle MS, Welsh M, Porter CK, Nieh C, Boyko EJ, Gackstetter G, Hooper TI |title=The Epidemiology of Irritable Bowel Syndrome in the US Military: Findings from the Millennium Cohort Study |journal=Am. J. Gastroenterol. |volume=111 |issue=1 |pages=93–104 |year=2016 |pmid=26729548 |pmc=4759150 |doi=10.1038/ajg.2015.386 |url=}}</ref> | |||
*** Abnormal serotonin pathways | |||
*** Neuroimmune factors | |||
*** Genetic factors- Mutations in SCN5A encode alpha subunit of voltage gated sodium channel NaV1.5 | |||
*** Bile acid malabsorption- causes alteration of the function of an apical ileal bile acid transporter | |||
==Genetics== | |||
** | |||
==Genetics== | |||
*[Disease name] is transmitted in [mode of genetic transmission] pattern. | |||
*Genes involved in the pathogenesis of [disease name] include [gene1], [gene2], and [gene3]. | |||
*The development of [disease name] is the result of multiple genetic mutations. | |||
==Associated Conditions== | |||
==Gross Pathology== | |||
*On gross pathology, [feature1], [feature2], and [feature3] are characteristic findings of [disease name]. | |||
==Microscopic Pathology== | |||
*On microscopic histopathological analysis, [feature1], [feature2], and [feature3] are characteristic findings of [disease name]. | |||
==References== | |||
{{Reflist|2}} | |||
{{WH}} | |||
{{WS}} | |||
[[Category: (name of the system)]] | |||
<div style="-webkit-user-select: none;"> | <div style="-webkit-user-select: none;"> | ||
{| class="infobox" style="position: fixed; top: 65%; right: 10px; margin: 0 0 0 0; border: 0; float: right;" | {| class="infobox" style="position: fixed; top: 65%; right: 10px; margin: 0 0 0 0; border: 0; float: right;" | ||
Revision as of 14:25, 24 October 2017
|
Irritable bowel syndrome Microchapters |
|
Differentiating Irritable bowel syndrome from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Sandbox:Cherry On the Web |
|
American Roentgen Ray Society Images of Sandbox:Cherry |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]; Associate Editor(s)-in-Chief:
Overview
The exact pathogenesis of [disease name] is not fully understood.
OR
It is thought that [disease name] is the result of / is mediated by / is produced by / is caused by either [hypothesis 1], [hypothesis 2], or [hypothesis 3].
OR
[Pathogen name] is usually transmitted via the [transmission route] route to the human host.
OR
Following transmission/ingestion, the [pathogen] uses the [entry site] to invade the [cell name] cell.
OR
[Disease or malignancy name] arises from [cell name]s, which are [cell type] cells that are normally involved in [function of cells].
OR
The progression to [disease name] usually involves the [molecular pathway].
OR
The pathophysiology of [disease/malignancy] depends on the histological subtype.
Pathophysiology
Pathogenesis
The exact pathogenesis of Irritable Bowel Syndrome (IBS) is uncertain. It is understood that IBS is caused by the interaction of various factors:
- Gastrointestinal motor abnormalities
- IBS is referred to as ‘spastic colon’ due to changes in colonic motor function.
- Manometry recordings from the transverse, descending and sigmoid colon have shown that spastic colon leads to changed patterns of colonic and small intestinal motor function such as increased frequency and irregularity of luminal contractions.[1][2][3]
- Peak amplitude of high-amplitude propagating contractions (HAPCs) in diarrhea-prone IBS patients is higher, compared to healthy subjects.[4][5]
- Diarrhea prone IBS patients have increased responses to ingestion, CRH(Corticotropin releasing hormone)[6][7], CCK(cholecystokinin)[8] and present with abdominal discomfort and accelerated transit through the colon.
- On the other hand, constipation prone IBS patients show fewer HAPCs, delayed transit through the colon and decreased motility.[4]
- It has been demonstrated that more than 90% of HAPCs are associated with abdominal pain.[8]
- CNS dysregulation
- The conceptualization of IBS being a brain gut disorder is reinforced by the following:
- Epidemiological studies suggest that IBS occurs in individuals who have experienced childhood trauma, with symptom exacerbation occurring in patients with emotional disturbances or stress.[9]
- Traumatic experiences before the age of 18 can directly shape adult connectivity in the executive control network. The effects on structures such as the insula, anterior cingulate cortex and the thalamus have been implicated in the pathophysiology of central pain amplification.[10]
- IBS has been found to have a high association with pre-existing psychiatric and psychological conditions like anxiety and depression.[11] However, studies have shown that even when patients are not anxious or depressed, the dorsolateral prefrontal cortex activity is reduced, pointing directly towards CNS dysfunction and increased susceptibility to stressors.[12]
- Psychological therapies that act on cerebral cortical sites and antidepressants have proven to be one of the mainstays of therapy for patients. The role of probiotics in modifying signal processing in the brain also proves that IBS is a brain gut disorder. [13]
- Studies using advanced brain imaging techniques have analyzed differences in brain activity and have helped us appreciate that the mid-cingulate cortex (responsible for attention processes and responses) and the prefrontal cortex(responsible for vigilance and alertness of the human brain) are involved in IBS. [10]
- Modulation of the mid-cingulate cortex is associated with alterations in the subjective sensations of pain whereas prefrontal cortex modulation may lead to increased perception of visceral pain.[10]
- Patients with IBS have aberrant processing of central information,[14] with decreased feedback on the emotional arousal network that controls the autonomic modulation of gastrointestinal function.[15]These have been seen as irregularities on diffusion tensor imaging[16] in the white matter of the brain.
- Rectal balloon distension in patients has shown the increased involvement of regions of the brain associated with attentional and behavioral responses to the arrival of such stimuli.[17][18][12]
- The conceptualization of IBS being a brain gut disorder is reinforced by the following:
- Visceral hypersensitivity
- Visceral hypersensitivity is an important factor in the pathogenesis of pain perception in IBS patients[19]. IBS is associated with a decreased threshold for perception of visceral stimuli[4][20] (i.e. visceral hypersensitivity).
- Studies in IBS patients have shown that rectal balloon inflation produces painful and non-painful sensations at lower volumes as compared to healthy controls, suggesting the presence of afferent pathway disturbances in visceral innervation[21][22][23][24]. Many factors contribute to visceral hyperalgesia(i.e increased sensitivity of the intestines to normal sensations):
- Spinal hyperexcitability due to activation of an N-methyl D aspartate(NMDA) receptor, Nitric oxide and possibly other neurotransmitters.
- Activation of specific gastrointestinal mediators like kinins and serotonin that lead to afferent nerve fiber sensitization.
- Central (brainstem and cortical) modulation with increased activation of anterior circulate cortex, thalamus and insula, involved in processing of pain, translating into long term hypersensitivity due to neuroplasticity, causing semipermanent changes in the neural response to all kinds of visceral stimulation. These findings have been proven by brain imaging studies. (e.g. functional magnetic resonance imaging, positron emission tomography)[20][25]
- Recruitment of peripheral silent nociceptors causing increased end organ sensitivity due to hormonal or immune activation[20].
- Immune activation and mucosal inflammation
- The high prevalence of IBS in patients with history of inflammatory bowel disease, celiac disease or microscopic colitis points towards the fact that immune activation and mucosal inflammation play an important role in the pathogenesis of IBS.[26][27][28][29][30][31][28]
- Moreover, psychological stress can significantly impact the release of proinflammatory cytokines, thereby affecting intestinal permeability and reinforcing a functional link existing between immune activation, psychological symptoms and symptoms in patients with IBS.[26]
- Patients are found to have higher mucosal counts of lymphocytes (T cells, B cells), mast cells and immune mediators such as prostanoids, proteases, cytokines and histamines. [28][32][33][34][35]
- Lymphocytes:
- Patients with IBS have increased B lymphocyte activation in the blood.[36] However, activation of humoral immunity in IBS is specific for the gastrointestinal tract[37] as increased numbers of lymphocytes have been found in the small intestine and colon of patients.[27][29]
- In addition to this, IBS patients with diarrhea[37] have enhanced mucosal humoral activity, associated with activation and proliferation of B cells and immunoglobulin production, identified by microarray profiling.
- IBS patients with severe disease have an increase in lymphocyte infiltration in the myentric plexus,[29] in studies where full-thickness jejunal biopsies were obtained.
- Mediators released by lymphocytes include histamine, proteases and nitric oxide. The stimulation of the enteric nervous system by these mediators leads to abnormal visceral and motor responses within the gastrointestinal tract.[27]
- Examination of stool in patients with diarrhea prominent IBS have high levels of serine protease activity.[38][39]When fecal extracts are intra colonically infused into mice, there is increased visceral pain and colonic cellular permeability. [38]
- Serine protease inhibitors prevent effects mediated by high levels of serine protease. Studies have shown that mononuclear cell supernatants in the peripheral blood from healthy controls have greater inhibitory effects on colorectal sensory afferent nerve endings than in IBS patients.[39][38]
- Mast cells:
- Proinflammatory cytokines:
- Cytokines are proteinaceous mediators of the immune response. Increased levels of cytokines have been found in IBS patients.[35][34]
- Higher amounts of of tumor necrosis factor are produced by the peripheral blood mononuclear cells of IBS patients.[40][28]
- In studies conducted using supernatants from cultured peripheral blood mononuclear cells in IBS patients,the TNF antagonist infliximab has been found to block the mechanical hypersensitivity of the mouse colonic afferent nerve endings. [41]
- Other cytokines such as interleukin 1β, interleukin 6, interleukin 10 and TNFα have been found in increased amounts on analysis of the supernatants from IBS patients with diarrhea, as compared to healthy controls.Increased concentration of these cytokines is directly proportional to the severity and frequency of pain.[28][41][40]
- Altered gut microbiota
- It is postulated that altered fecal microflora may be associated with IBS.[42][32] There are numerous studies that suggest that altered fecal microflora in IBS patients differ from healthy controls. [43][44][45][46][47]
- Inoculation of germ free animals with fecal microbiota from IBS patients has demonstrated increased colonic hypersensitivity, as compared to samples inoculated from healthy controls. [48]
- Studies have also shown that the fecal microbiota in patients with post infectious IBS differs markedly from healthy controls, with decrease in the diversity of the fecal microbiome, correlated with increased numbers of CD8 and CD4RA-positive intraepithelial lymphocytes. [49]
- IBS patients who have undergone colonoscopy, with sampling from the colon and terminal ileum have been found to have colonic spirochaetosis with a unique pathology of increased lymphoid follicles and eosinophils as compared to healthy controls.[50]
- IBS with diarrhea is sometimes preceded by acute enteric infections and therefore, benefit from probiotics that serve to alter metabolism and composition of the microflora.[51][52] Administration of probiotics in patients decreases flatulence relative to Lactobacillus.[53] A probiotic yogurt containing a mixture of Bacteroides species has been shown to improve symptoms in IBS patients.[54]
- Studies have been conducted suggesting that the switching on of a T-helper-2 immune-cell response may cause increased susceptibility to IBS after acute GI infection.[55][56]
- Abnormal serotonin pathways
- Neuroimmune factors
- Genetic factors- Mutations in SCN5A encode alpha subunit of voltage gated sodium channel NaV1.5
- Bile acid malabsorption- causes alteration of the function of an apical ileal bile acid transporter
Genetics
Genetics
- [Disease name] is transmitted in [mode of genetic transmission] pattern.
- Genes involved in the pathogenesis of [disease name] include [gene1], [gene2], and [gene3].
- The development of [disease name] is the result of multiple genetic mutations.
Associated Conditions
Gross Pathology
- On gross pathology, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
Microscopic Pathology
- On microscopic histopathological analysis, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
References
- ↑ Schmidt T, Hackelsberger N, Widmer R, Meisel C, Pfeiffer A, Kaess H (1996). "Ambulatory 24-hour jejunal motility in diarrhea-predominant irritable bowel syndrome". Scand. J. Gastroenterol. 31 (6): 581–9. PMID 8789897.
- ↑ Kumar D, Wingate DL (1985). "The irritable bowel syndrome: a paroxysmal motor disorder". Lancet. 2 (8462): 973–7. PMID 2865504.
- ↑ Simrén M, Castedal M, Svedlund J, Abrahamsson H, Björnsson E (2000). "Abnormal propagation pattern of duodenal pressure waves in the irritable bowel syndrome (IBS) [correction of (IBD)]". Dig. Dis. Sci. 45 (11): 2151–61. PMID 11215731.
- ↑ 4.0 4.1 4.2 Camilleri M, McKinzie S, Busciglio I, Low PA, Sweetser S, Burton D, Baxter K, Ryks M, Zinsmeister AR (2008). "Prospective study of motor, sensory, psychologic, and autonomic functions in patients with irritable bowel syndrome". Clin. Gastroenterol. Hepatol. 6 (7): 772–81. doi:10.1016/j.cgh.2008.02.060. PMC 2495078. PMID 18456567.
- ↑ Kellow JE, Phillips SF (1987). "Altered small bowel motility in irritable bowel syndrome is correlated with symptoms". Gastroenterology. 92 (6): 1885–93. PMID 3569764.
- ↑ Whitehead WE, Engel BT, Schuster MM (1980). "Irritable bowel syndrome: physiological and psychological differences between diarrhea-predominant and constipation-predominant patients". Dig. Dis. Sci. 25 (6): 404–13. PMID 7379673.
- ↑ Fukudo S, Nomura T, Hongo M (1998). "Impact of corticotropin-releasing hormone on gastrointestinal motility and adrenocorticotropic hormone in normal controls and patients with irritable bowel syndrome". Gut. 42 (6): 845–9. PMC 1727153. PMID 9691924.
- ↑ 8.0 8.1 Chey WY, Jin HO, Lee MH, Sun SW, Lee KY (2001). "Colonic motility abnormality in patients with irritable bowel syndrome exhibiting abdominal pain and diarrhea". Am. J. Gastroenterol. 96 (5): 1499–506. doi:10.1111/j.1572-0241.2001.03804.x. PMID 11374689.
- ↑ Park SH, Videlock EJ, Shih W, Presson AP, Mayer EA, Chang L (2016). "Adverse childhood experiences are associated with irritable bowel syndrome and gastrointestinal symptom severity". Neurogastroenterol. Motil. 28 (8): 1252–60. doi:10.1111/nmo.12826. PMC 4956522. PMID 27061107.
- ↑ 10.0 10.1 10.2 Gupta A, Kilpatrick L, Labus J, Tillisch K, Braun A, Hong JY, Ashe-McNalley C, Naliboff B, Mayer EA (2014). "Early adverse life events and resting state neural networks in patients with chronic abdominal pain: evidence for sex differences". Psychosom Med. 76 (6): 404–12. doi:10.1097/PSY.0000000000000089. PMC 4113723. PMID 25003944.
- ↑ Mearin F, Lacy BE, Chang L, Chey WD, Lembo AJ, Simren M, Spiller R (2016). "Bowel Disorders". Gastroenterology. doi:10.1053/j.gastro.2016.02.031. PMID 27144627.
- ↑ 12.0 12.1 Larsson MB, Tillisch K, Craig AD, Engström M, Labus J, Naliboff B, Lundberg P, Ström M, Mayer EA, Walter SA (2012). "Brain responses to visceral stimuli reflect visceral sensitivity thresholds in patients with irritable bowel syndrome". Gastroenterology. 142 (3): 463–472.e3. doi:10.1053/j.gastro.2011.11.022. PMC 3288538. PMID 22108191.
- ↑ Tillisch K, Labus J, Kilpatrick L, Jiang Z, Stains J, Ebrat B, Guyonnet D, Legrain-Raspaud S, Trotin B, Naliboff B, Mayer EA (2013). "Consumption of fermented milk product with probiotic modulates brain activity". Gastroenterology. 144 (7): 1394–401, 1401.e1–4. doi:10.1053/j.gastro.2013.02.043. PMC 3839572. PMID 23474283.
- ↑ Hong JY, Kilpatrick LA, Labus J, Gupta A, Jiang Z, Ashe-McNalley C, Stains J, Heendeniya N, Ebrat B, Smith S, Tillisch K, Naliboff B, Mayer EA (2013). "Patients with chronic visceral pain show sex-related alterations in intrinsic oscillations of the resting brain". J. Neurosci. 33 (29): 11994–2002. doi:10.1523/JNEUROSCI.5733-12.2013. PMC 3713732. PMID 23864686.
- ↑ Hall GB, Kamath MV, Collins S, Ganguli S, Spaziani R, Miranda KL, Bayati A, Bienenstock J (2010). "Heightened central affective response to visceral sensations of pain and discomfort in IBS". Neurogastroenterol. Motil. 22 (3): 276–e80. doi:10.1111/j.1365-2982.2009.01436.x. PMID 20003075.
- ↑ Ellingson BM, Mayer E, Harris RJ, Ashe-McNally C, Naliboff BD, Labus JS, Tillisch K (2013). "Diffusion tensor imaging detects microstructural reorganization in the brain associated with chronic irritable bowel syndrome". Pain. 154 (9): 1528–41. doi:10.1016/j.pain.2013.04.010. PMC 3758125. PMID 23721972.
- ↑ Elsenbruch S, Rosenberger C, Bingel U, Forsting M, Schedlowski M, Gizewski ER (2010). "Patients with irritable bowel syndrome have altered emotional modulation of neural responses to visceral stimuli". Gastroenterology. 139 (4): 1310–9. doi:10.1053/j.gastro.2010.06.054. PMID 20600024.
- ↑ Elsenbruch S, Rosenberger C, Enck P, Forsting M, Schedlowski M, Gizewski ER (2010). "Affective disturbances modulate the neural processing of visceral pain stimuli in irritable bowel syndrome: an fMRI study". Gut. 59 (4): 489–95. doi:10.1136/gut.2008.175000. PMID 19651629.
- ↑ Whitehead WE, Holtkotter B, Enck P, Hoelzl R, Holmes KD, Anthony J, Shabsin HS, Schuster MM (1990). "Tolerance for rectosigmoid distention in irritable bowel syndrome". Gastroenterology. 98 (5 Pt 1): 1187–92. PMID 2323511.
- ↑ 20.0 20.1 20.2 Barbara G, Cremon C, De Giorgio R, Dothel G, Zecchi L, Bellacosa L, Carini G, Stanghellini V, Corinaldesi R (2011). "Mechanisms underlying visceral hypersensitivity in irritable bowel syndrome". Curr Gastroenterol Rep. 13 (4): 308–15. doi:10.1007/s11894-011-0195-7. PMID 21537962.
- ↑ Mertz H, Naliboff B, Munakata J, Niazi N, Mayer EA (1995). "Altered rectal perception is a biological marker of patients with irritable bowel syndrome". Gastroenterology. 109 (1): 40–52. PMID 7797041.
- ↑ Prior A, Maxton DG, Whorwell PJ (1990). "Anorectal manometry in irritable bowel syndrome: differences between diarrhoea and constipation predominant subjects". Gut. 31 (4): 458–62. PMC 1378424. PMID 2338274.
- ↑ Posserud I, Syrous A, Lindström L, Tack J, Abrahamsson H, Simrén M (2007). "Altered rectal perception in irritable bowel syndrome is associated with symptom severity". Gastroenterology. 133 (4): 1113–23. doi:10.1053/j.gastro.2007.07.024. PMID 17919487.
- ↑ Bouin M, Plourde V, Boivin M, Riberdy M, Lupien F, Laganière M, Verrier P, Poitras P (2002). "Rectal distention testing in patients with irritable bowel syndrome: sensitivity, specificity, and predictive values of pain sensory thresholds". Gastroenterology. 122 (7): 1771–7. PMID 12055583.
- ↑ Mertz H, Morgan V, Tanner G, Pickens D, Price R, Shyr Y, Kessler R (2000). "Regional cerebral activation in irritable bowel syndrome and control subjects with painful and nonpainful rectal distention". Gastroenterology. 118 (5): 842–8. PMID 10784583.
- ↑ 26.0 26.1 Coëffier M, Gloro R, Boukhettala N, Aziz M, Lecleire S, Vandaele N, Antonietti M, Savoye G, Bôle-Feysot C, Déchelotte P, Reimund JM, Ducrotté P (2010). "Increased proteasome-mediated degradation of occludin in irritable bowel syndrome". Am. J. Gastroenterol. 105 (5): 1181–8. doi:10.1038/ajg.2009.700. PMID 19997094.
- ↑ 27.0 27.1 27.2 Chadwick VS, Chen W, Shu D, Paulus B, Bethwaite P, Tie A, Wilson I (2002). "Activation of the mucosal immune system in irritable bowel syndrome". Gastroenterology. 122 (7): 1778–83. PMID 12055584.
- ↑ 28.0 28.1 28.2 28.3 28.4 Liebregts T, Adam B, Bredack C, Röth A, Heinzel S, Lester S, Downie-Doyle S, Smith E, Drew P, Talley NJ, Holtmann G (2007). "Immune activation in patients with irritable bowel syndrome". Gastroenterology. 132 (3): 913–20. doi:10.1053/j.gastro.2007.01.046. PMID 17383420.
- ↑ 29.0 29.1 29.2 Törnblom H, Lindberg G, Nyberg B, Veress B (2002). "Full-thickness biopsy of the jejunum reveals inflammation and enteric neuropathy in irritable bowel syndrome". Gastroenterology. 123 (6): 1972–9. doi:10.1053/gast.2002.37059. PMID 12454854.
- ↑ 30.0 30.1 Guilarte M, Santos J, de Torres I, Alonso C, Vicario M, Ramos L, Martínez C, Casellas F, Saperas E, Malagelada JR (2007). "Diarrhoea-predominant IBS patients show mast cell activation and hyperplasia in the jejunum". Gut. 56 (2): 203–9. doi:10.1136/gut.2006.100594. PMC 1856785. PMID 17005763.
- ↑ 31.0 31.1 31.2 Barbara G, Stanghellini V, De Giorgio R, Cremon C, Cottrell GS, Santini D, Pasquinelli G, Morselli-Labate AM, Grady EF, Bunnett NW, Collins SM, Corinaldesi R (2004). "Activated mast cells in proximity to colonic nerves correlate with abdominal pain in irritable bowel syndrome". Gastroenterology. 126 (3): 693–702. PMID 14988823.
- ↑ 32.0 32.1 Marshall JK, Thabane M, Garg AX, Clark WF, Moayyedi P, Collins SM (2010). "Eight year prognosis of postinfectious irritable bowel syndrome following waterborne bacterial dysentery". Gut. 59 (5): 605–11. doi:10.1136/gut.2009.202234. PMID 20427395.
- ↑ Wensaas KA, Langeland N, Hanevik K, Mørch K, Eide GE, Rortveit G (2012). "Irritable bowel syndrome and chronic fatigue 3 years after acute giardiasis: historic cohort study". Gut. 61 (2): 214–9. doi:10.1136/gutjnl-2011-300220. PMID 21911849.
- ↑ 34.0 34.1 Mearin F, Perelló A, Balboa A, Perona M, Sans M, Salas A, Angulo S, Lloreta J, Benasayag R, García-Gonzalez MA, Pérez-Oliveras M, Coderch J (2009). "Pathogenic mechanisms of postinfectious functional gastrointestinal disorders: results 3 years after gastroenteritis". Scand. J. Gastroenterol. 44 (10): 1173–85. doi:10.1080/00365520903171276. PMID 19711225.
- ↑ 35.0 35.1 Gwee KA, Collins SM, Read NW, Rajnakova A, Deng Y, Graham JC, McKendrick MW, Moochhala SM (2003). "Increased rectal mucosal expression of interleukin 1beta in recently acquired post-infectious irritable bowel syndrome". Gut. 52 (4): 523–6. PMC 1773606. PMID 12631663.
- ↑ Ohman L, Lindmark AC, Isaksson S, Posserud I, Strid H, Sjövall H, Simrén M (2009). "B-cell activation in patients with irritable bowel syndrome (IBS)". Neurogastroenterol. Motil. 21 (6): 644–50, e27. doi:10.1111/j.1365-2982.2009.01272.x. PMID 19222763.
- ↑ 37.0 37.1 Vicario M, González-Castro AM, Martínez C, Lobo B, Pigrau M, Guilarte M, de Torres I, Mosquera JL, Fortea M, Sevillano-Aguilera C, Salvo-Romero E, Alonso C, Rodiño-Janeiro BK, Söderholm JD, Azpiroz F, Santos J (2015). "Increased humoral immunity in the jejunum of diarrhoea-predominant irritable bowel syndrome associated with clinical manifestations". Gut. 64 (9): 1379–88. doi:10.1136/gutjnl-2013-306236. PMID 25209656.
- ↑ 38.0 38.1 38.2 Bueno L (2008). "Protease activated receptor 2: a new target for IBS treatment". Eur Rev Med Pharmacol Sci. 12 Suppl 1: 95–102. PMID 18924448.
- ↑ 39.0 39.1 Gecse K, Róka R, Ferrier L, Leveque M, Eutamene H, Cartier C, Ait-Belgnaoui A, Rosztóczy A, Izbéki F, Fioramonti J, Wittmann T, Bueno L (2008). "Increased faecal serine protease activity in diarrhoeic IBS patients: a colonic lumenal factor impairing colonic permeability and sensitivity". Gut. 57 (5): 591–9. doi:10.1136/gut.2007.140210. PMID 18194983.
- ↑ 40.0 40.1 Dinan TG, Quigley EM, Ahmed SM, Scully P, O'Brien S, O'Mahony L, O'Mahony S, Shanahan F, Keeling PW (2006). "Hypothalamic-pituitary-gut axis dysregulation in irritable bowel syndrome: plasma cytokines as a potential biomarker?". Gastroenterology. 130 (2): 304–11. doi:10.1053/j.gastro.2005.11.033. PMID 16472586.
- ↑ 41.0 41.1 Hughes PA, Moretta M, Lim A, Grasby DJ, Bird D, Brierley SM, Liebregts T, Adam B, Blackshaw LA, Holtmann G, Bampton P, Hoffmann P, Andrews JM, Zola H, Krumbiegel D (2014). "Immune derived opioidergic inhibition of viscerosensory afferents is decreased in Irritable Bowel Syndrome patients". Brain Behav. Immun. 42: 191–203. doi:10.1016/j.bbi.2014.07.001. PMID 25063707.
- ↑ Ford AC, Thabane M, Collins SM, Moayyedi P, Garg AX, Clark WF, Marshall JK (2010). "Prevalence of uninvestigated dyspepsia 8 years after a large waterborne outbreak of bacterial dysentery: a cohort study". Gastroenterology. 138 (5): 1727–36, quiz e12. doi:10.1053/j.gastro.2010.01.043. PMID 20117111.
- ↑ Kassinen A, Krogius-Kurikka L, Mäkivuokko H, Rinttilä T, Paulin L, Corander J, Malinen E, Apajalahti J, Palva A (2007). "The fecal microbiota of irritable bowel syndrome patients differs significantly from that of healthy subjects". Gastroenterology. 133 (1): 24–33. doi:10.1053/j.gastro.2007.04.005. PMID 17631127.
- ↑ Malinen E, Rinttilä T, Kajander K, Mättö J, Kassinen A, Krogius L, Saarela M, Korpela R, Palva A (2005). "Analysis of the fecal microbiota of irritable bowel syndrome patients and healthy controls with real-time PCR". Am. J. Gastroenterol. 100 (2): 373–82. doi:10.1111/j.1572-0241.2005.40312.x. PMID 15667495.
- ↑ Rajilić-Stojanović M, Biagi E, Heilig HG, Kajander K, Kekkonen RA, Tims S, de Vos WM (2011). "Global and deep molecular analysis of microbiota signatures in fecal samples from patients with irritable bowel syndrome". Gastroenterology. 141 (5): 1792–801. doi:10.1053/j.gastro.2011.07.043. PMID 21820992.
- ↑ Saulnier DM, Riehle K, Mistretta TA, Diaz MA, Mandal D, Raza S, Weidler EM, Qin X, Coarfa C, Milosavljevic A, Petrosino JF, Highlander S, Gibbs R, Lynch SV, Shulman RJ, Versalovic J (2011). "Gastrointestinal microbiome signatures of pediatric patients with irritable bowel syndrome". Gastroenterology. 141 (5): 1782–91. doi:10.1053/j.gastro.2011.06.072. PMC 3417828. PMID 21741921.
- ↑ Jeffery IB, O'Toole PW, Öhman L, Claesson MJ, Deane J, Quigley EM, Simrén M (2012). "An irritable bowel syndrome subtype defined by species-specific alterations in faecal microbiota". Gut. 61 (7): 997–1006. doi:10.1136/gutjnl-2011-301501. PMID 22180058.
- ↑ Crouzet L, Gaultier E, Del'Homme C, Cartier C, Delmas E, Dapoigny M, Fioramonti J, Bernalier-Donadille A (2013). "The hypersensitivity to colonic distension of IBS patients can be transferred to rats through their fecal microbiota". Neurogastroenterol. Motil. 25 (4): e272–82. doi:10.1111/nmo.12103. PMID 23433203.
- ↑ Sundin J, Rangel I, Fuentes S, Heikamp-de Jong I, Hultgren-Hörnquist E, de Vos WM, Brummer RJ (2015). "Altered faecal and mucosal microbial composition in post-infectious irritable bowel syndrome patients correlates with mucosal lymphocyte phenotypes and psychological distress". Aliment. Pharmacol. Ther. 41 (4): 342–51. doi:10.1111/apt.13055. PMID 25521822.
- ↑ Walker MM, Talley NJ, Inganäs L, Engstrand L, Jones MP, Nyhlin H, Agréus L, Kjellstrom L, Öst Å, Andreasson A (2015). "Colonic spirochetosis is associated with colonic eosinophilia and irritable bowel syndrome in a general population in Sweden". Hum. Pathol. 46 (2): 277–83. doi:10.1016/j.humpath.2014.10.026. PMID 25540866.
- ↑ Chassard C, Dapoigny M, Scott KP, Crouzet L, Del'homme C, Marquet P, Martin JC, Pickering G, Ardid D, Eschalier A, Dubray C, Flint HJ, Bernalier-Donadille A (2012). "Functional dysbiosis within the gut microbiota of patients with constipated-irritable bowel syndrome". Aliment. Pharmacol. Ther. 35 (7): 828–38. doi:10.1111/j.1365-2036.2012.05007.x. PMID 22315951.
- ↑ Camilleri M (2008). "Probiotics and irritable bowel syndrome: rationale, mechanisms, and efficacy". J. Clin. Gastroenterol. 42 Suppl 3 Pt 1: S123–5. doi:10.1097/MCG.0b013e3181574393. PMID 18806702.
- ↑ Nobaek S, Johansson ML, Molin G, Ahrné S, Jeppsson B (2000). "Alteration of intestinal microflora is associated with reduction in abdominal bloating and pain in patients with irritable bowel syndrome". Am. J. Gastroenterol. 95 (5): 1231–8. doi:10.1111/j.1572-0241.2000.02015.x. PMID 10811333.
- ↑ Maccaferri S, Candela M, Turroni S, Centanni M, Severgnini M, Consolandi C, Cavina P, Brigidi P (2012). "IBS-associated phylogenetic unbalances of the intestinal microbiota are not reverted by probiotic supplementation". Gut Microbes. 3 (5): 406–13. doi:10.4161/gmic.21009. PMID 22713265.
- ↑ Wouters MM, Van Wanrooy S, Nguyen A, Dooley J, Aguilera-Lizarraga J, Van Brabant W, Garcia-Perez JE, Van Oudenhove L, Van Ranst M, Verhaegen J, Liston A, Boeckxstaens G (2016). "Psychological comorbidity increases the risk for postinfectious IBS partly by enhanced susceptibility to develop infectious gastroenteritis". Gut. 65 (8): 1279–88. doi:10.1136/gutjnl-2015-309460. PMID 26071133.
- ↑ Riddle MS, Welsh M, Porter CK, Nieh C, Boyko EJ, Gackstetter G, Hooper TI (2016). "The Epidemiology of Irritable Bowel Syndrome in the US Military: Findings from the Millennium Cohort Study". Am. J. Gastroenterol. 111 (1): 93–104. doi:10.1038/ajg.2015.386. PMC 4759150. PMID 26729548.
| https://https://www.youtube.com/watch?v=9f5wxYW0Z3k%7C350}} |
Initially, IBS was considered a psychosomatic illness, and the involvement of biological and pathogenic factors was not verified until the 1990s, a process common in the history of emerging infectious diseases. The risk of developing IBS increases six-fold after acute gastrointestinal infection. Post-infection, further risk factors are young age, prolonged fever, anxiety and depression.[1]
Psychosomatic illness
One of the first references to the concept of an "Irritable Bowel" appeared in the Rocky Mountain Medical Journal in 1950.[2] The term was used to categorize patients who developed symptoms of diarrhea, abdominal pain, constipation, but where no well-recognized infective cause could be found. Early theories suggested that the Irritable Bowel was caused by a somatic, or mental disorder. One paper from the 1980s investigated "learned illness behavior" in patients with IBS and peptic ulcers.[3] Another study suggested that both IBS and stomach ulcer patients would benefit from 15 months of psychotherapy.[4] Later, it was found that most stomach ulcers were caused by a bacterial infection with Helicobacter pylori.[5]
Additional publications suggesting the role of brain-gut "axis" appeared in the 1990s, such as a study entitled Brain-gut response to stress and cholinergic stimulation in IBS published in the Journal of Clinical Gastrotnerology in 1993.[6] A 1997 study published in Gut magazine suggested that IBS was associated with a "derailing of the brain-gut axis."[7]
Immune reaction
From the late 1990s, research publications began identifying specific biochemical changes present in tissue biopsies and serum samples from IBS patients that suggested symptoms had an organic rather than psychosomatic cause. These studies identified cytokines and secretory products in tissues taken from IBS patients. The cytokines identified in IBS patients produce inflammation and are associated with the body's immune response.
- A study showed that intestinal biopsies from patients with constipation predominant IBS secreted higher levels of serotonin in-vitro.[9] Serotonin plays a role in regulating gastrointestinal motility and water content and can be altered by some diseases and infections.[10][11][12]
- A study of rectal biopsy tissue from IBS patients showed increased levels of cellular structures involved in the production of the cytokine Interleukin 1 Beta.[13]
- A study of blood samples from IBS patients identified elevated levels of cytokines Tumor necrosis factor-alpha, Interleukin 1, and Interleukin 6 in patients with IBS.[14]
- A study of intestinal biopsies from IBS patients showed increased levels of protease enzymes used by the body to digest proteins, and by infectious agents to combat the host's immune system.[15]
- A study of blood samples from IBS patients found elevated levels of antibodies to the protozoan Blastocystis.[16]
Specific forms of immune response that have been implicated in IBS symptoms include coeliac disease and other food allergy conditions.[17] Coeliac disease (also spelled "celiac") is an immunoglobulin type A-(IgA) mediated allergic response to the gliadin protein in gluten grains,which exhibits wide variety of symptoms and can present as IBS. "Some patients with diarrhea-predominant irritable bowel syndrome (IBS-D) may have undiagnosed celiac sprue (CS). Because the symptoms of CS respond to a gluten-free diet, testing for CS in IBS may prevent years of morbidity and attendant expense."[18] "Coeliac disease is a common finding among patients labelled as having irritable bowel syndrome. In this sub-group, a gluten free diet may lead to a significant improvement in symptoms. Routine testing for coeliac disease may be indicated in all patients being evaluated for irritable bowel syndrome."[19] Food allergies, particularly those mediated by IgE and IgG-type antibodies have been implicated in IBS.[20][21][22]
Active infections
There is research to support IBS being caused by an as-yet undiscovered active infection. Most recently, a study has found that the antibiotic Rifaximin provides sustained relief for IBS patients.[23] While some researchers see this as evidence that IBS is related to an undiscovered agent, others believe IBS patients suffer from overgrowth of intestinal flora and the antibiotics are effective in reducing the overgrowth (known as small intestinal bacterial overgrowth).[24] Other researchers have focused on an unrecognized protozoal infection as a cause of IBS[25] as certain protozoal infections occur more frequently in IBS patients.[26][27] Two of the protozoa investigated have a high prevalence in industrialized countries and infect the bowel, but little is known about them as they are recently emerged pathogens.
Blastocystis is a single-celled organism which has been reported to produce symptoms of abdominal pain, constipation and diarrhea in patients, along with headaches and depression,[28] though these reports are contested by some physicians.[29] Studies from research hospitals in various countries have identified high Blastocystis infection rates in IBS patients, with 38% being reported from London School of Hygiene & Tropical Medicine,[30] 47% reported from the Department of Gastroenterology at Aga Khan University in Pakistan[26] and 18.1% reported from the Institute of Diseases and Public Health at University of Ancona in Italy.[27] Reports from all three groups indicate a Blastocystis prevalence of approximately 7% in non-IBS patients. Researchers have noted that clinical diagnostics fail to identify infection,[31] and Blastocystis may not respond to treatment with common antiprotozoals.[32][33][34][35]
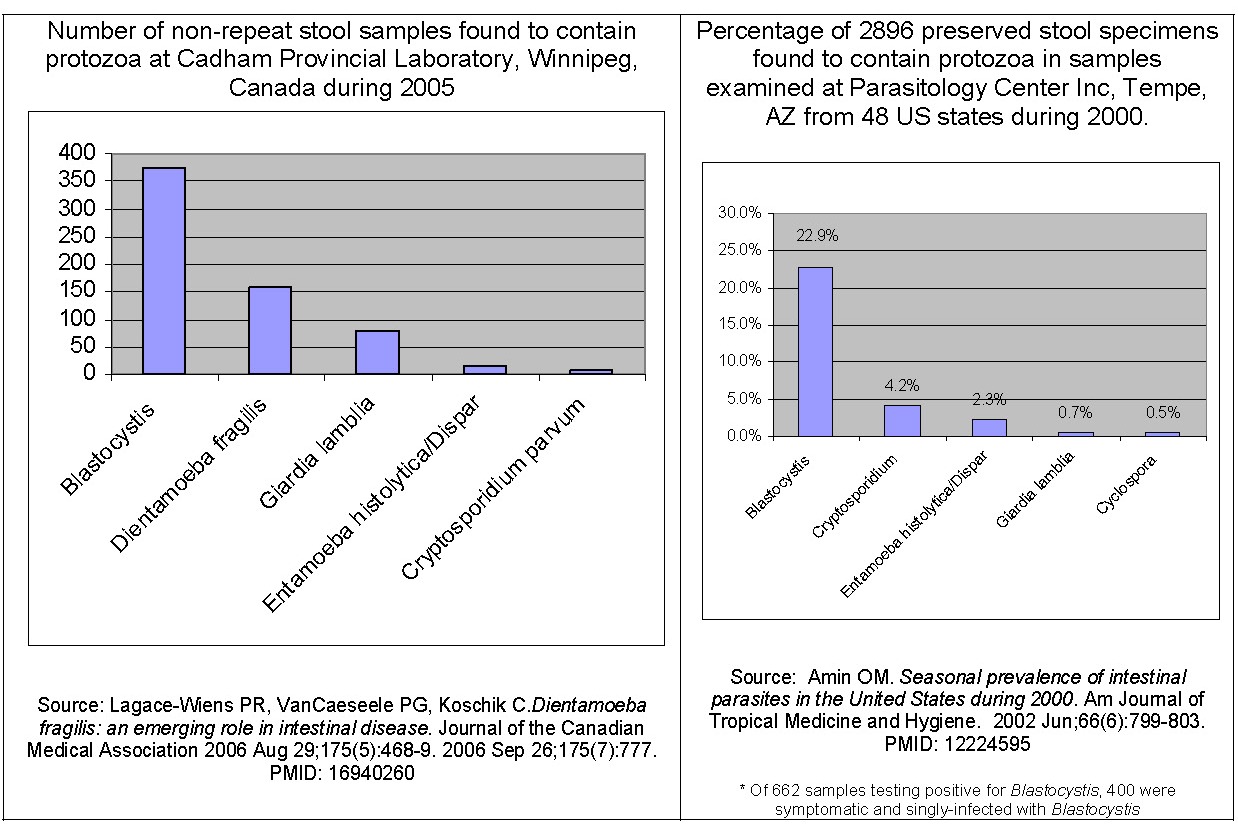
Dientamoeba fragilis is a single-celled organism which produces abdominal pain and diarrhea. Studies have reported a high incidence of infection in developed countries, and symptoms of patients resolve following antibiotic treatment.[36][38] One study reported on a large group of patients with IBS-like symptoms who were found to be infected with Dientamoeba fragilis and experienced resolution of symptoms following treatment.[39] Researchers have noted that methods used clinically may fail to detect some Dientamoeba fragilis infections.[38]
Pathophysiology
Pathogenesis
- The exact pathogenesis of [disease name] is not fully understood.
OR
- It is thought that [disease name] is the result of / is mediated by / is produced by / is caused by either [hypothesis 1], [hypothesis 2], or [hypothesis 3].
- [Pathogen name] is usually transmitted via the [transmission route] route to the human host.
- Following transmission/ingestion, the [pathogen] uses the [entry site] to invade the [cell name] cell.
- [Disease or malignancy name] arises from [cell name]s, which are [cell type] cells that are normally involved in [function of cells].
- The progression to [disease name] usually involves the [molecular pathway].
- The pathophysiology of [disease/malignancy] depends on the histological subtype.
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3]; Associate Editor(s)-in-Chief: Sudarshana Datta, MD [4]
Overview
| gkfff | |||
|---|---|---|---|
| blbkgg | df | ||
| bjkb |
Pathophysiology
Diagnosis
IBS is a diagnosis of [40] [41] Visceral hypersensitivity may have been utilized as a clinical marker of IBS and could be represented by signs and symptoms of urgency for bowel movements, bloating and abdominal pain. The mechanisms that result in persistent visceral hypersensitivity in patients who have IBS are unclear. nonetheless, various working models might be considered
|
Xyz Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Sandbox:Cherry On the Web |
|
American Roentgen Ray Society Images of Sandbox:Cherry |
For patient information, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [5]; Associate Editor(s)-in-Chief:
Synonyms and keywords:
Overview
Historical Perspective
Classification
Pathophysiology
Causes
Differentiating Xyz from other Diseases
Epidemiology and Demographics
Risk Factors
Screening
Natural History, Complications, and Prognosis
Diagnosis
History and Symptoms | Physical Examination | Electrocardiogram | Laboratory Findings | X-Ray Findings | Echocardiography and Ultrasound | CT-Scan Findings | MRI Findings | Other Diagnostic Studies | Other Imaging Findings
Treatment
Medical Therapy | Surgery | Primary Prevention | Secondary Prevention | Cost-Effectiveness of Therapy | Future or Investigational Therapies
Case Studies
- ↑ Thabane M, Kottachchi DT, Marshall JK (2007). "The incidence and prognosis of post-infectious irritable bowel syndrome". Aliment Pharmacol Ther. 26 (4): 535–44. PMID 17661757.
- ↑ BROWN PW (1950). "The irritable bowel syndrome". Rocky Mountain medical journal. 47 (5): 343–6. PMID 15418074.
- ↑ Whitehead WE, Winget C, Fedoravicius AS, Wooley S, Blackwell B (1982). "Learned illness behavior in patients with irritable bowel syndrome and peptic ulcer". Dig. Dis. Sci. 27 (3): 202–8. PMID 7075418.
- ↑ Svedlund J, Sjödin I (1985). "A psychosomatic approach to treatment in the irritable bowel syndrome and peptic ulcer disease with aspects of the design of clinical trials". Scand. J. Gastroenterol. Suppl. 109: 147–51. PMID 3895386.
- ↑ Damianos AJ, McGarrity TJ (1997). "Treatment strategies for Helicobacter pylori infection". American family physician. 55 (8): 2765–74, 2784–6. PMID 9191460.
- ↑ Fukudo S, Nomura T, Muranaka M, Taguchi F (1993). "Brain-gut response to stress and cholinergic stimulation in irritable bowel syndrome. A preliminary study". J. Clin. Gastroenterol. 17 (2): 133–41. PMID 8031340.
- ↑ Orr WC, Crowell MD, Lin B, Harnish MJ, Chen JD (1997). "Sleep and gastric function in irritable bowel syndrome: derailing the brain-gut axis". Gut. 41 (3): 390–3. PMID 9378397.
- ↑ El-Omar EM, Carrington M, Chow WH; et al. (2000). "Interleukin-1 polymorphisms associated with increased risk of gastric cancer". Nature. 404 (6776): 398–402. doi:10.1038/35006081. PMID 10746728.
- ↑ Miwa J, Echizen H, Matsueda K, Umeda N (2001). "Patients with constipation-predominant irritable bowel syndrome (IBS) may have elevated serotonin concentrations in colonic mucosa as compared with diarrhea-predominant patients and subjects with normal bowel habits". Digestion. 63 (3): 188–94. PMID 11351146.
- ↑ McGowan K, Kane A, Asarkof N; et al. (1983). "Entamoeba histolytica causes intestinal secretion: role of serotonin". Science. 221 (4612): 762–4. PMID 6308760.
- ↑ McGowan K, Guerina V, Wicks J, Donowitz M (1985). "Secretory hormones of Entamoeba histolytica". Ciba Found. Symp. 112: 139–54. PMID 2861068.
- ↑ Banu, Naheed; et al. (2005). "Neurohumoral alterations and their role in amoebiasis" (PDF). Indian J. Clin Biochem. 20 (2): 142–5.
- ↑ Gwee KA, Collins SM, Read NW; et al. (2003). "Increased rectal mucosal expression of interleukin 1beta in recently acquired post-infectious irritable bowel syndrome". Gut. 52 (4): 523–6. PMID 12631663.
- ↑ Liebregts T, Adam B, Bredack C; et al. (2007). "Immune activation in patients with irritable bowel syndrome". Gastroenterology. 132 (3): 913–20. doi:10.1053/j.gastro.2007.01.046. PMID 17383420.
- ↑ Cenac N, Andrews CN, Holzhausen M; et al. (2007). "Role for protease activity in visceral pain in irritable bowel syndrome". J. Clin. Invest. 117 (3): 636–47. doi:10.1172/JCI29255. PMID 17304351.
- ↑ Hussain R, Jaferi W, Zuberi S; et al. (1997). "Significantly increased IgG2 subclass antibody levels to Blastocystis hominis in patients with irritable bowel syndrome". Am. J. Trop. Med. Hyg. 56 (3): 301–6. PMID 9129532.
- ↑ Wangen, Dr. Stephen. The Irritable Bowel Syndrome Solution. 2006. ISBN 0976853787. Excerpted with author's permission at [1]
- ↑ Spiegel BM; et al. (2004). "Testing for celiac sprue in irritable bowel syndrome with predominant diarrhea: a cost-effectiveness analysis". Gastroenterology. 126 (7): 1721–32. PMID 15188167.
- ↑ Shahbazkhani B; et al. (2003). "Coeliac disease presenting with symptoms of irritable bowel syndrome". Aliment Pharmacol Therapy. 18 (2): 231–5. PMID 12869084.
- ↑ Li H; et al. (2007). "Allergen-IgE complexes trigger CD23-dependent CCL20 release from human intestinal epithelial cells". Gastroenterology. 133 (6): 1905–15. PMID 18054562.
- ↑ "The therapeutic effects of eliminating allergic foods according to food-specific IgG antibodies in irritable bowel syndrome - Article in Chinese". Zhonghua Nei Ke Za Zhi. 46 (8): 641–3. 2007. PMID 17967233. Text "Yang CM, Li YQ " ignored (help)
- ↑ Drisko; et al. (2006). "Treating Irritable Bowel Syndrome with a Food Elimination Diet Followed by Food Challenge and Probiotics". Journal of the American College of Nutrition. 25 (6): 514–22. PMID 17229899.
- ↑ Pimentel M, Park S, Mirocha J, Kane SV, Kong Y (2006). "The effect of a nonabsorbed oral antibiotic (rifaximin) on the symptoms of the irritable bowel syndrome: a randomized trial". Ann. Intern. Med. 145 (8): 557–63. PMID 17043337.
- ↑ Posserud I, Stotzer PO, Björnsson ES, Abrahamsson H, Simrén M (2007). "Small intestinal bacterial overgrowth in patients with irritable bowel syndrome". Gut. 56 (6): 802–8. doi:10.1136/gut.2006.108712. PMID 17148502.
- ↑ Stark D, van Hal S, Marriott D, Ellis J, Harkness J (2007). "Irritable bowel syndrome: a review on the role of intestinal protozoa and the importance of their detection and diagnosis". Int. J. Parasitol. 37 (1): 11–20. doi:10.1016/j.ijpara.2006.09.009. PMID 17070814.
- ↑ 26.0 26.1 Yakoob J, Jafri W, Jafri N; et al. (2004). "Irritable bowel syndrome: in search of an etiology: role of Blastocystis hominis". Am. J. Trop. Med. Hyg. 70 (4): 383–5. PMID 15100450.
- ↑ 27.0 27.1 Giacometti A, Cirioni O, Fiorentini A, Fortuna M, Scalise G (1999). "Irritable bowel syndrome in patients with Blastocystis hominis infection". Eur. J. Clin. Microbiol. Infect. Dis. 18 (6): 436–9. PMID 10442423.
- ↑ Qadri SM, al-Okaili GA, al-Dayel F (1989). "Clinical significance of Blastocystis hominis". J. Clin. Microbiol. 27 (11): 2407–9. PMID 2808664.
- ↑ Markell EK, Udkow MP (1986). "Blastocystis hominis: pathogen or fellow traveler?". Am. J. Trop. Med. Hyg. 35 (5): 1023–6. PMID 3766850.
- ↑ Windsor J (2007). "B. hominis and D. fragilis: Neglected human protozoa". British Biomedical Scientist: 524–7.
- ↑ Stensvold R, Brillowska-Dabrowska A, Nielsen HV, Arendrup MC (2006). "Detection of Blastocystis hominis in unpreserved stool specimens by using polymerase chain reaction". J. Parasitol. 92 (5): 1081–7. PMID 17152954.
- ↑ Yakoob J, Jafri W, Jafri N, Islam M, Asim Beg M (2004). "In vitro susceptibility of Blastocystis hominis isolated from patients with irritable bowel syndrome". Br. J. Biomed. Sci. 61 (2): 75–7. PMID 15250669.
- ↑ Haresh K, Suresh K, Khairul Anus A, Saminathan S (1999). "Isolate resistance of Blastocystis hominis to metronidazole". Trop. Med. Int. Health. 4 (4): 274–7. PMID 10357863.
- ↑ Markell EK, Udkow MP (1986). "Blastocystis hominis: pathogen or fellow traveler?". Am. J. Trop. Med. Hyg. 35 (5): 1023–6. PMID 3766850.
- ↑ Ok UZ, Girginkardeşler N, Balcioğlu C, Ertan P, Pirildar T, Kilimcioğlu AA (1999). "Effect of trimethoprim-sulfamethaxazole in Blastocystis hominis infection". Am. J. Gastroenterol. 94 (11): 3245–7. PMID 10566723.
- ↑ 36.0 36.1 Lagacé-Wiens PR, VanCaeseele PG, Koschik C (2006). "Dientamoeba fragilis: an emerging role in intestinal disease". CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne. 175 (5): 468–9. doi:10.1503/cmaj.060265. PMID 16940260.
- ↑ Amin OM (2002). "Seasonal prevalence of intestinal parasites in the United States during 2000". Am. J. Trop. Med. Hyg. 66 (6): 799–803. PMID 12224595.
- ↑ 38.0 38.1 Stensvold CR, Arendrup MC, Mølbak K, Nielsen HV (2007). "The prevalence of Dientamoeba fragilis in patients with suspected enteroparasitic disease in a metropolitan area in Denmark". Clin. Microbiol. Infect. 13 (8): 839–42. doi:10.1111/j.1469-0691.2007.01760.x. PMID 17610603.
- ↑ Borody T, Warren E, Wettstein A; et al. (2002). "Eradication of Dientamoeba fragilis can resolve IBS-like symptoms". J Gastroenterol Hepatol. 17 (Suppl, pages=A103).
- ↑ "api.isoa.org" (PDF).
- ↑ Dorn SD, Palsson OS, Thiwan SI, Kanazawa M, Clark WC, van Tilburg MA, Drossman DA, Scarlett Y, Levy RL, Ringel Y, Crowell MD, Olden KW, Whitehead WE (2007). "Increased colonic pain sensitivity in irritable bowel syndrome is the result of an increased tendency to report pain rather than increased neurosensory sensitivity". Gut. 56 (9): 1202–9. doi:10.1136/gut.2006.117390. PMC 1954968. PMID 17483191.