Multiple myeloma pathophysiology: Difference between revisions
| Line 9: | Line 9: | ||
*Multiple myeloma arises from post-germinal center [[B lymphocytes]], that are normally involved in production of human [[immunoglobulins]].<ref>Multiple myeloma. Wikipedia (2015)https://en.wikipedia.org/wiki/Multiple_myeloma#Pathophysiology</ref><ref>Multiple myeloma. Medlineplus (2015)https://www.nlm.nih.gov/medlineplus/multiplemyeloma.html</ref> | *Multiple myeloma arises from post-germinal center [[B lymphocytes]], that are normally involved in production of human [[immunoglobulins]].<ref>Multiple myeloma. Wikipedia (2015)https://en.wikipedia.org/wiki/Multiple_myeloma#Pathophysiology</ref><ref>Multiple myeloma. Medlineplus (2015)https://www.nlm.nih.gov/medlineplus/multiplemyeloma.html</ref> | ||
* Production of [[cytokine]]s (especially [[Interleukin 6|IL-6]]) by the plasma cells causes much of their localised damage, such as [[osteoporosis]], and creates a microenvironment in which the [[malignant]] cells thrive.<ref>Multiple myeloma. Wikipedia (2015) https://en.wikipedia.org/wiki/Multiple_myeloma#Pathophysiology</ref> | * Production of [[cytokine]]s (especially [[Interleukin 6|IL-6]]) by the plasma cells causes much of their localised damage, such as [[osteoporosis]], and creates a microenvironment in which the [[malignant]] cells thrive.<ref>Multiple myeloma. Wikipedia (2015) https://en.wikipedia.org/wiki/Multiple_myeloma#Pathophysiology</ref> | ||
*Immune | *Immune deficiencyas tne majority of the antibodies are ineffective monoclonal antibodies produced from the clonal plasma cell.<ref><ref>Multiple myeloma. Wikipedia (2015) https://en.wikipedia.org/wiki/Multiple_myeloma#Pathophysiology</ref> </ref> | ||
* The produced antibodies are deposited in various organs leading [[polyneuropathy]] and various other multiple myeloma associated symptoms. | * The produced antibodies are deposited in various organs leading [[polyneuropathy]] and various other multiple myeloma associated symptoms. | ||
*Renal failure due to glomerular deposition of [[amyloid]] or tubular damage from excretion of [[light chain]]s called [[Bence Jones protein]]s, which can manifest as the [[Fanconi syndrome]] (type II [[renal tubular acidosis]]).<ref>Multiple myeloma. Wikipedia (2015) https://en.wikipedia.org/wiki/Multiple_myeloma#Pathophysiology</ref> | *Renal failure due to glomerular deposition of [[amyloid]] or tubular damage from excretion of [[light chain]]s called [[Bence Jones protein]]s, which can manifest as the [[Fanconi syndrome]] (type II [[renal tubular acidosis]]).<ref>Multiple myeloma. Wikipedia (2015) https://en.wikipedia.org/wiki/Multiple_myeloma#Pathophysiology</ref> | ||
Revision as of 19:17, 18 September 2015
|
Multiple myeloma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Multiple myeloma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Multiple myeloma pathophysiology |
|
Risk calculators and risk factors for Multiple myeloma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Multiple myeloma arises from post-germinal center B lymphocytes, that are normally involved in production of human immunoglobulins. Development of multiple myeloma is the result of multiple genetic translocation between the immunoglobulin heavy chain gene and oncogenes which leads to dysregulated multiplication of plasma cells.[1][2] On microscopic histopathological analysis, abundant eosinophilic cytoplasm, eccentrically placed nucleus, russell bodies and dutcher bodies are characteristic findings of multiple myeloma.[3]
Pathogenesis
- Multiple myeloma arises from post-germinal center B lymphocytes, that are normally involved in production of human immunoglobulins.[4][5]
- Production of cytokines (especially IL-6) by the plasma cells causes much of their localised damage, such as osteoporosis, and creates a microenvironment in which the malignant cells thrive.[6]
- Immune deficiencyas tne majority of the antibodies are ineffective monoclonal antibodies produced from the clonal plasma cell. </ref>
- The produced antibodies are deposited in various organs leading polyneuropathy and various other multiple myeloma associated symptoms.
- Renal failure due to glomerular deposition of amyloid or tubular damage from excretion of light chains called Bence Jones proteins, which can manifest as the Fanconi syndrome (type II renal tubular acidosis).[7]
Genetics
- Genes involved in the pathogenesis of multiple myeloma include heavy chain gene (on the chromosome 14, locus 14q32), chromosome 13, and oncogenes (often 11q13, 4p16.3, 6p21, 16q23 and 20q11).[8]
- A genetic mutation results in dysregulation of the oncogene which is thought to be an important initiating event in the pathogenesis of multiple myeloma.
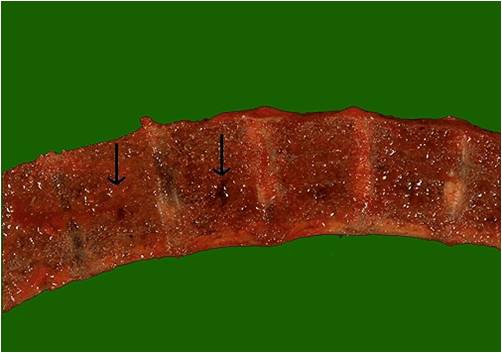
Gross Pathology
-
Vertebras in multiple myeloma
(Image courtesy of Melih Aktan M.D.) -
Calvarium in multiple myeloma.
(Image courtesy of Melih Aktan M.D.)
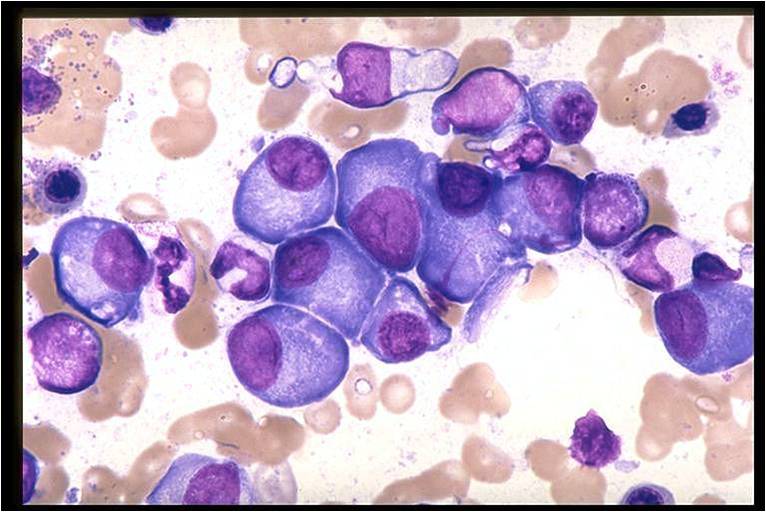
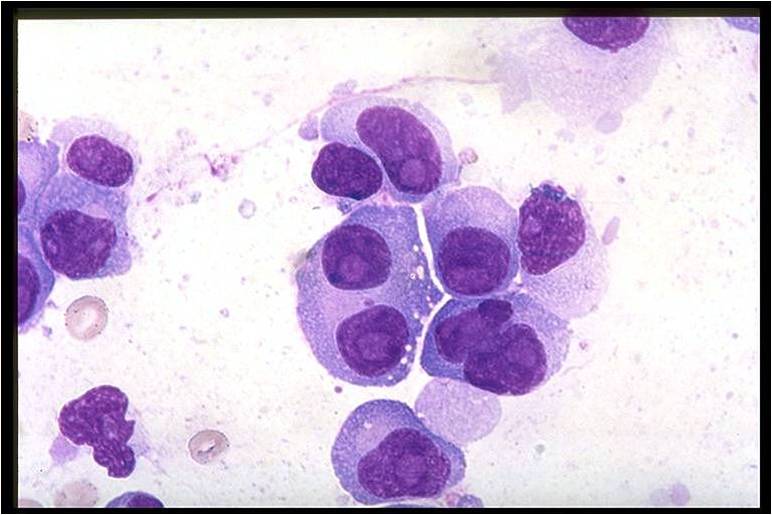
Microscopic Pathology
On microscopic histopathological analysis, multiple myeloma is characterized by the following:[9]
- Abundant eosinophilic cytoplasm.
- Eccentrically placed nucleus.
- Clock face morphology of the nucleus due to chromatin clumps around the edges.
- Russell bodies which are eosinophilic, large (10-15 micrometres), homogenous immunoglobulin-containing inclusions.
- Dutcher bodies which are PAS stain +ve intranuclear crystalline rods.
-
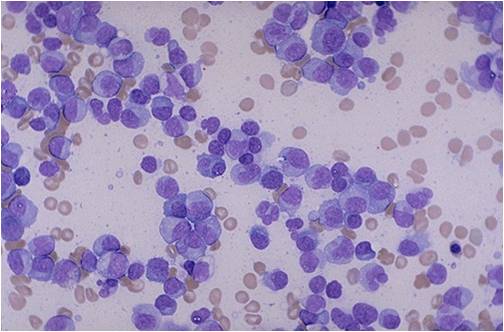
Multiple Myeloma slide showing plasma cells with large nucleus and scant cytoplasm [10]
-
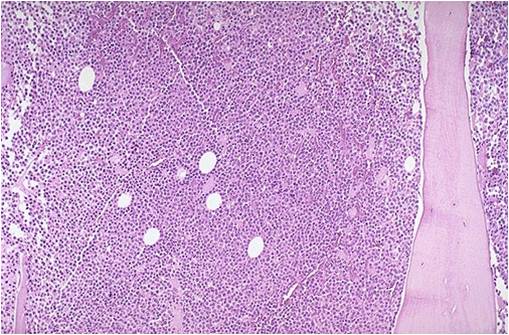
Bone marrow aspiration in multiple myeloma.
(Image courtesy of Melih Aktan M.D.) -
Bone marrow biopsy in multiple myeloma.
(Image courtesy of Melih Aktan M.D.) -
Bone marrow in multiple myeloma.
(Image courtesy of Melih Aktan M.D.) -
Bone marrow in multiple myeloma.
(Image courtesy of Melih Aktan M.D.)
References
- ↑ Multiple myeloma. Wikipedia (2015)https://en.wikipedia.org/wiki/Multiple_myeloma#Pathophysiology
- ↑ Multiple myeloma. Medlineplus (2015)https://www.nlm.nih.gov/medlineplus/multiplemyeloma.html
- ↑ Multiple myeloma. Librepathology (2015)http://www.wikidoc.org/index.php?title=Multiple_myeloma_pathophysiology&action=edit§ion=1
- ↑ Multiple myeloma. Wikipedia (2015)https://en.wikipedia.org/wiki/Multiple_myeloma#Pathophysiology
- ↑ Multiple myeloma. Medlineplus (2015)https://www.nlm.nih.gov/medlineplus/multiplemyeloma.html
- ↑ Multiple myeloma. Wikipedia (2015) https://en.wikipedia.org/wiki/Multiple_myeloma#Pathophysiology
- ↑ Multiple myeloma. Wikipedia (2015) https://en.wikipedia.org/wiki/Multiple_myeloma#Pathophysiology
- ↑ Kyle RA, Rajkumar SV. Multiple myeloma. N Engl J Med 2004;351:1860-73. PMID 15509819.
- ↑ Multiple myeloma. Librepathology(2015)http://librepathology.org/wiki/index.php/Plasma_cell_neoplasms
- ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages

![Multiple Myeloma slide showing plasma cells with large nucleus and scant cytoplasm [10]](/images/a/a5/Multiple_Myeloma.jpg)