Endometrial cancer classification: Difference between revisions
No edit summary |
|||
| Line 5: | Line 5: | ||
==Overview== | ==Overview== | ||
==Classification== | ==Classification== | ||
Cellular Classification of Endometrial Cancer | |||
Endometrial cancers are classified in one of the following two categories: | |||
Type 1 may arise from complex atypical hyperplasia and is pathogenetically linked to unopposed estrogenic stimulation. | |||
Type 2 develops from atrophic endometrium and is not linked to hormonally driven pathogenesis. | |||
Characteristic activating oncogenic mutations or amplification and inactivating mutations or deletion of tumor suppressors are seen more in association with one type of mutation versus the other type, but some overlap exists. With the Cancer Genome Atlas and a full genetic display of hundreds of endometrial cancers, four subtypes have been identified that will refine classification and provide prognostic and therapeutic implications.[1] | |||
<gallery> | The most common endometrial cancer cell type is endometrioid adenocarcinoma, which is composed of malignant glandular epithelial elements; an admixture of squamous metaplasia is not uncommon. Adenosquamous tumors contain malignant elements of both glandular and squamous epithelium;[2] clear cell and papillary serous carcinoma of the endometrium are tumors that are histologically similar to those noted in the ovary and the fallopian tube, and the prognosis is worse for these tumors.[3] Mucinous, squamous, and undifferentiated tumors are rarely encountered. Frequency of endometrial cancer cell types is as follows: | ||
Endometrioid (75%–80%). | |||
Ciliated adenocarcinoma. | |||
Secretory adenocarcinoma. | |||
Papillary or villoglandular. | |||
Adenocarcinoma with squamous differentiation. | |||
Adenoacanthoma. | |||
Adenosquamous. | |||
Uterine papillary serous (<10%). | |||
Mucinous (1%). | |||
Clear cell (4%). | |||
Squamous cell (<1%). | |||
Mixed (10%). | |||
Undifferentiated.Cellular Classification of Endometrial Cancer | |||
Endometrial cancers are classified in one of the following two categories: | |||
Type 1 may arise from complex atypical hyperplasia and is pathogenetically linked to unopposed estrogenic stimulation. | |||
Type 2 develops from atrophic endometrium and is not linked to hormonally driven pathogenesis. | |||
Characteristic activating oncogenic mutations or amplification and inactivating mutations or deletion of tumor suppressors are seen more in association with one type of mutation versus the other type, but some overlap exists. With the Cancer Genome Atlas and a full genetic display of hundreds of endometrial cancers, four subtypes have been identified that will refine classification and provide prognostic and therapeutic implications.[1] | |||
The most common endometrial cancer cell type is endometrioid adenocarcinoma, which is composed of malignant glandular epithelial elements; an admixture of squamous metaplasia is not uncommon. Adenosquamous tumors contain malignant elements of both glandular and squamous epithelium;[2] clear cell and papillary serous carcinoma of the endometrium are tumors that are histologically similar to those noted in the ovary and the fallopian tube, and the prognosis is worse for these tumors.[3] Mucinous, squamous, and undifferentiated tumors are rarely encountered. Frequency of endometrial cancer cell types is as follows: | |||
Endometrioid (75%–80%). | |||
Ciliated adenocarcinoma. | |||
Secretory adenocarcinoma. | |||
Papillary or villoglandular. | |||
Adenocarcinoma with squamous differentiation. | |||
Adenoacanthoma. | |||
Adenosquamous. | |||
Uterine papillary serous (<10%). | |||
Mucinous (1%). | |||
Clear cell (4%). | |||
Squamous cell (<1%). | |||
Mixed (10%). | |||
Undifferentiated.<gallery> | |||
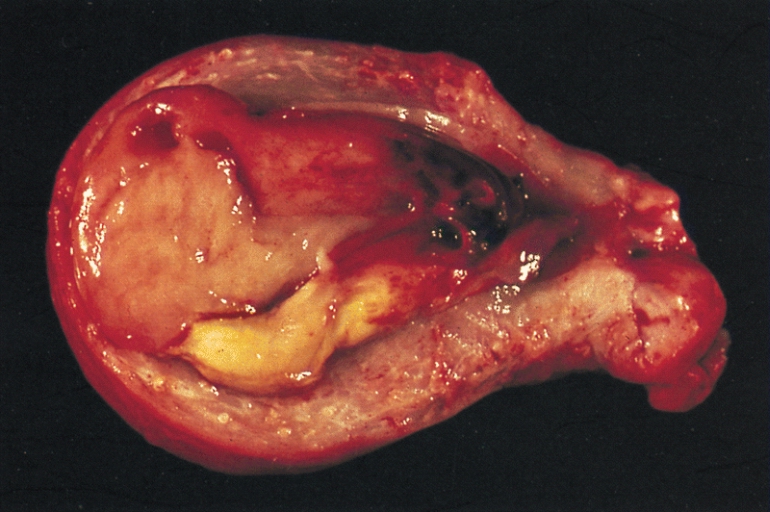
Image:Endometrial stromal sarcoma gross.jpg|Endometrial stromal sarcoma | Image:Endometrial stromal sarcoma gross.jpg|Endometrial stromal sarcoma | ||
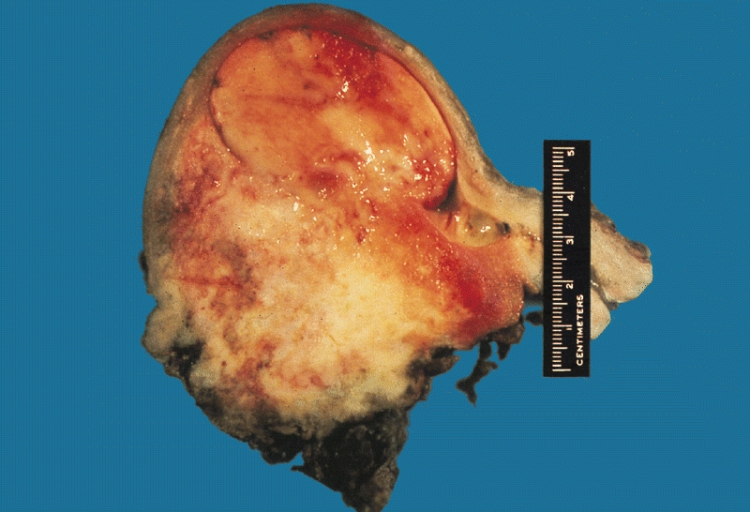
Image:Uterine carcinosarcoma.jpg|Malignant mixed müllerian tumor | Image:Uterine carcinosarcoma.jpg|Malignant mixed müllerian tumor | ||
Revision as of 15:03, 1 September 2015
|
Endometrial cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Endometrial cancer classification On the Web |
|
American Roentgen Ray Society Images of Endometrial cancer classification |
|
Risk calculators and risk factors for Endometrial cancer classification |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Classification
Cellular Classification of Endometrial Cancer
Endometrial cancers are classified in one of the following two categories:
Type 1 may arise from complex atypical hyperplasia and is pathogenetically linked to unopposed estrogenic stimulation. Type 2 develops from atrophic endometrium and is not linked to hormonally driven pathogenesis.
Characteristic activating oncogenic mutations or amplification and inactivating mutations or deletion of tumor suppressors are seen more in association with one type of mutation versus the other type, but some overlap exists. With the Cancer Genome Atlas and a full genetic display of hundreds of endometrial cancers, four subtypes have been identified that will refine classification and provide prognostic and therapeutic implications.[1]
The most common endometrial cancer cell type is endometrioid adenocarcinoma, which is composed of malignant glandular epithelial elements; an admixture of squamous metaplasia is not uncommon. Adenosquamous tumors contain malignant elements of both glandular and squamous epithelium;[2] clear cell and papillary serous carcinoma of the endometrium are tumors that are histologically similar to those noted in the ovary and the fallopian tube, and the prognosis is worse for these tumors.[3] Mucinous, squamous, and undifferentiated tumors are rarely encountered. Frequency of endometrial cancer cell types is as follows:
Endometrioid (75%–80%).
Ciliated adenocarcinoma. Secretory adenocarcinoma. Papillary or villoglandular. Adenocarcinoma with squamous differentiation.
Adenoacanthoma. Adenosquamous.
Uterine papillary serous (<10%). Mucinous (1%). Clear cell (4%). Squamous cell (<1%). Mixed (10%). Undifferentiated.Cellular Classification of Endometrial Cancer
Endometrial cancers are classified in one of the following two categories:
Type 1 may arise from complex atypical hyperplasia and is pathogenetically linked to unopposed estrogenic stimulation. Type 2 develops from atrophic endometrium and is not linked to hormonally driven pathogenesis.
Characteristic activating oncogenic mutations or amplification and inactivating mutations or deletion of tumor suppressors are seen more in association with one type of mutation versus the other type, but some overlap exists. With the Cancer Genome Atlas and a full genetic display of hundreds of endometrial cancers, four subtypes have been identified that will refine classification and provide prognostic and therapeutic implications.[1]
The most common endometrial cancer cell type is endometrioid adenocarcinoma, which is composed of malignant glandular epithelial elements; an admixture of squamous metaplasia is not uncommon. Adenosquamous tumors contain malignant elements of both glandular and squamous epithelium;[2] clear cell and papillary serous carcinoma of the endometrium are tumors that are histologically similar to those noted in the ovary and the fallopian tube, and the prognosis is worse for these tumors.[3] Mucinous, squamous, and undifferentiated tumors are rarely encountered. Frequency of endometrial cancer cell types is as follows:
Endometrioid (75%–80%).
Ciliated adenocarcinoma. Secretory adenocarcinoma. Papillary or villoglandular. Adenocarcinoma with squamous differentiation.
Adenoacanthoma. Adenosquamous.
Uterine papillary serous (<10%). Mucinous (1%). Clear cell (4%). Squamous cell (<1%). Mixed (10%).
Undifferentiated.
-
Endometrial stromal sarcoma
-
Malignant mixed müllerian tumor