Pregabalin: Difference between revisions
No edit summary |
No edit summary |
||
| Line 333: | Line 333: | ||
: [[File:{{PAGENAME}}07.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | : [[File:{{PAGENAME}}07.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
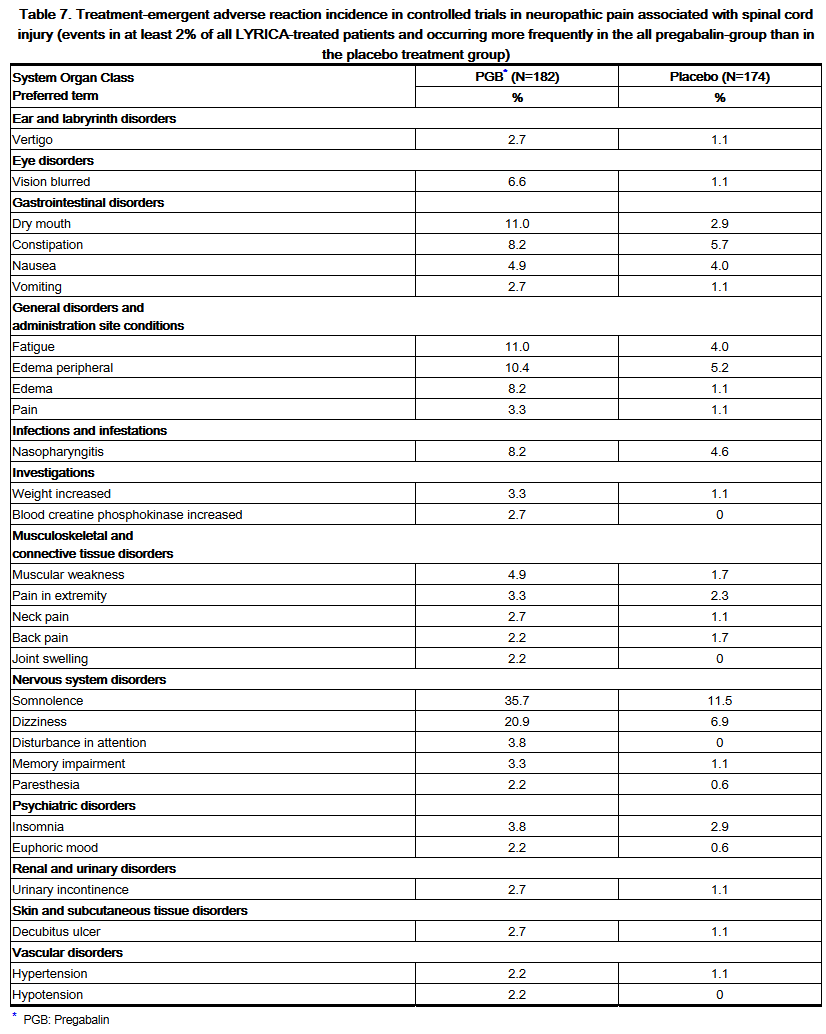
*Controlled Studies in Neuropathic Pain Associated with Spinal Cord Injury | |||
*Adverse Reactions Leading to Discontinuation | |||
:*In clinical trials of patients with neuropathic pain associated with spinal cord injury, 13% of patients treated with pregabalin and 10% of patients treated with placebo discontinued prematurely due to adverse reactions. In the pregabalin treatment group, the most common reasons for discontinuation due to adverse reactions were somnolence (3%) and edema (2%). In comparison, none of the placebo-treated patients withdrew due to somnolence and edema. Other reasons for discontinuation from the trials, occurring with greater frequency in the pregabalin treatment group than in the placebo treatment group, were fatigue and balance disorder. Each of these adverse reactions led to withdrawal in less than 2% of patients. | |||
*Most Common Adverse Reactions | |||
:*Table 7 lists all adverse reactions, regardless of causality, occurring in ≥2% of patients with neuropathic pain associated with spinal cord injury in the controlled trials. A majority of pregabalin-treated patients in clinical studies experienced adverse reactions with a maximum intensity of "mild" or "moderate". | |||
Revision as of 15:01, 1 August 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Vignesh Ponnusamy, M.B.B.S. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Pregabalin is a that is FDA approved for the {{{indicationType}}} of neuropathic pain associated with diabetic peripheral neuropathy (DPN), postherpetic neuralgia (PHN), adjunctive therapy for adult patients with partial onset seizures ,fibromyalgia, neuropathic pain associated with spinal cord injury.. Common adverse reactions include dizziness, somnolence, dry mouth, edema, blurred vision, weight gain and thinking abnormal (primarily difficulty with concentration/attention)..
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
- LYRICA is indicated for:
- Management of neuropathic pain associated with diabetic peripheral neuropathy
- Management of postherpetic neuralgia
- Adjunctive therapy for adult patients with partial onset seizures
- Management of fibromyalgia
- Management of neuropathic pain associated with spinal cord injury
Dosage And Administration
- LYRICA is given orally with or without food.
- When discontinuing LYRICA, taper gradually over a minimum of 1 week.
Neuropathic Pain Associated with Diabetic Peripheral Neuropathy
- The maximum recommended dose of LYRICA is 100 mg three times a day (300 mg/day) in patients with creatinine clearance of at least 60 mL/min. Begin dosing at 50 mg three times a day (150 mg/day). The dose may be increased to 300 mg/day within 1 week based on efficacy and tolerability. Because LYRICA is eliminated primarily by renal excretion, adjust the dose in patients with reduced renal function.
- Although LYRICA was also studied at 600 mg/day, there is no evidence that this dose confers additional significant benefit and this dose was less well tolerated. In view of the dose-dependent adverse reactions, treatment with doses above 300 mg/day is not recommended [see Adverse Reactions (6.1)].
Postherpetic Neuralgia
- The recommended dose of LYRICA is 75 to 150 mg two times a day, or 50 to 100 mg three times a day (150 to 300 mg/day) in patients with creatinine clearance of at least 60 mL/min. Begin dosing at 75 mg two times a day, or 50 mg three times a day (150 mg/day). The dose may be increased to 300 mg/day within 1 week based on efficacy and tolerability. Because LYRICA is eliminated primarily by renal excretion, adjust the dose in patients with reduced renal function.
- Patients who do not experience sufficient pain relief following 2 to 4 weeks of treatment with 300 mg/day, and who are able to tolerate LYRICA, may be treated with up to 300 mg two times a day, or 200 mg three times a day (600 mg/day). In view of the dose-dependent adverse reactions and the higher rate of treatment discontinuation due to adverse reactions, reserve dosing above 300 mg/day for those patients who have on-going pain and are tolerating 300 mg daily.
Adjunctive Therapy for Adult Patients with Partial Onset Seizures
- LYRICA at doses of 150 to 600 mg/day has been shown to be effective as adjunctive therapy in the treatment of partial onset seizures in adults. Both the efficacy and adverse event profiles of LYRICA have been shown to be dose-related. Administer the total daily dose in two or three divided doses. In general, it is recommended that patients be started on a total daily dose no greater than 150 mg/day (75 mg two times a day, or 50 mg three times a day). Based on individual patient response and tolerability, the dose may be increased to a maximum dose of 600 mg/day.
- Because LYRICA is eliminated primarily by renal excretion, adjust the dose in patients with reduced renal function.
- The effect of dose escalation rate on the tolerability of LYRICA has not been formally studied.
- The efficacy of add-on LYRICA in patients taking gabapentin has not been evaluated in controlled trials. Consequently, dosing recommendations for the use of LYRICA with gabapentin cannot be offered.
Management of Fibromyalgia
- The recommended dose of LYRICA for fibromyalgia is 300 to 450 mg/day. Begin dosing at 75 mg two times a day (150 mg/day). The dose may be increased to 150 mg two times a day (300 mg/day) within 1 week based on efficacy and tolerability. Patients who do not experience sufficient benefit with 300 mg/day may be further increased to 225 mg two times a day (450 mg/day). Although LYRICA was also studied at 600 mg/day, there is no evidence that this dose confers additional benefit and this dose was less well tolerated. In view of the dose-dependent adverse reactions, treatment with doses above 450 mg/day is not recommended. Because LYRICA is eliminated primarily by renal excretion, adjust the dose in patients with reduced renal function.
Neuropathic Pain Associated with Spinal Cord Injury
- The recommended dose range of LYRICA for the treatment of neuropathic pain associated with spinal cord injury is 150 to 600 mg/day. The recommended starting dose is 75 mg two times a day (150 mg/day). The dose may be increased to 150 mg two times a day (300 mg/day) within 1 week based on efficacy and tolerability. Patients who do not experience sufficient pain relief after 2 to 3 weeks of treatment with 150 mg two times a day and who tolerate LYRICA may be treated with up to 300 mg two times a day. Because LYRICA is eliminated primarily by renal excretion, adjust the dose in patients with reduced renal function.
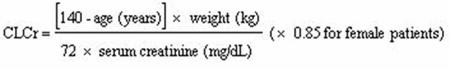
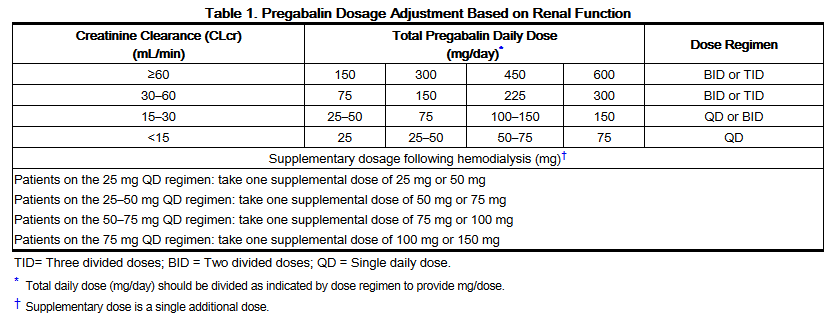
Patients with Renal Impairment
- In view of dose-dependent adverse reactions and since LYRICA is eliminated primarily by renal excretion, adjust the dose in patients with reduced renal function. Base the dose adjustment in patients with renal impairment on creatinine clearance (CLcr), as indicated in Table 1. To use this dosing table, an estimate of the patient's CLcr in mL/min is needed. CLcr in mL/min may be estimated from serum creatinine (mg/dL) determination using the Cockcroft and Gault equation:
- Next, refer to the Dosage and Administration section to determine the recommended total daily dose based on indication, for a patient with normal renal function (CLcr ≥60 mL/min). Then refer to Table 1 to determine the corresponding renal adjusted dose.
- (For example: A patient initiating LYRICA therapy for postherpetic neuralgia with normal renal function (CLcr ≥60 mL/min), receives a total daily dose of 150 mg/day pregabalin. Therefore, a renal impaired patient with a CLcr of 50 mL/min would receive a total daily dose of 75 mg/day pregabalin administered in two or three divided doses.)
- For patients undergoing hemodialysis, adjust the pregabalin daily dose based on renal function. In addition to the daily dose adjustment, administer a supplemental dose immediately following every 4-hour hemodialysis treatment (see Table 1).
Oral Solution Concentration and Dispensing
- The oral solution is 20 mg pregabalin per milliliter (mL) and prescriptions should be written in milligrams (mg). The pharmacist will calculate the applicable dose in mL for dispensing (e.g., 150 mg equals 7.5 mL oral solution).
Dosage Forms And Strengths
- Capsules: 25 mg, 50 mg, 75 mg, 100 mg, 150 mg, 200 mg, 225 mg, and 300 mg
- Oral Solution: 20 mg/mL
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Condition1
- Developed by:
- Class of Recommendation:
- Strength of Evidence:
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Guideline-Supported Use of Pregabalin in adult patients.
Non–Guideline-Supported Use
Condition1
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Non–Guideline-Supported Use of Pregabalin in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Condition1
- Dosing Information
- Dosage
Condition2
There is limited information regarding FDA-Labeled Use of Pregabalin in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
Condition1
- Developed by:
- Class of Recommendation:
- Strength of Evidence:
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Guideline-Supported Use of Pregabalin in pediatric patients.
Non–Guideline-Supported Use
Condition1
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Non–Guideline-Supported Use of Pregabalin in pediatric patients.
Contraindications
- LYRICA is contraindicated in patients with known hypersensitivity to pregabalin or any of its components. Angioedema and hypersensitivity reactions have occurred in patients receiving pregabalin therapy.
Warnings
Precautions
- Angioedema
- There have been postmarketing reports of angioedema in patients during initial and chronic treatment with LYRICA. Specific symptoms included swelling of the face, mouth (tongue, lips, and gums), and neck (throat and larynx). There were reports of life-threatening angioedema with respiratory compromise requiring emergency treatment. Discontinue LYRICA immediately in patients with these symptoms.
- Exercise caution when prescribing LYRICA to patients who have had a previous episode of angioedema. In addition, patients who are taking other drugs associated with angioedema (e.g., angiotensin converting enzyme inhibitors [ACE-inhibitors]) may be at increased risk of developing angioedema.
- Hypersensitivity
- There have been postmarketing reports of hypersensitivity in patients shortly after initiation of treatment with LYRICA. Adverse reactions included skin redness, blisters, hives, rash, dyspnea, and wheezing. Discontinue LYRICA immediately in patients with these symptoms.
- Withdrawal of Antiepileptic Drugs (AEDs)
- As with all AEDs, withdraw LYRICA gradually to minimize the potential of increased seizure frequency in patients with seizure disorders. If LYRICA is discontinued, taper the drug gradually over a minimum of 1 week.
- Suicidal Behavior and Ideation
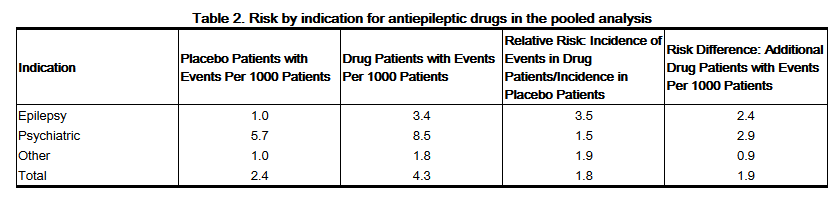
- Antiepileptic drugs (AEDs), including LYRICA, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Monitor patients treated with any AED for any indication for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
- Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43%, compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
- The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
- The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5–100 years) in the clinical trials analyzed.
- Table 2 shows absolute and relative risk by indication for all evaluated AEDs.
- The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
- Anyone considering prescribing LYRICA or any other AED must balance the risk of suicidal thoughts or behavior with the risk of untreated illness. Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
- Inform patients, their caregivers, and families that LYRICA and other AEDs increase the risk of suicidal thoughts and behavior and advise them of the need to be alert for the emergence or worsening of the signs and symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Report behaviors of concern immediately to healthcare providers.
- Peripheral Edema
- LYRICA treatment may cause peripheral edema. In short-term trials of patients without clinically significant heart or peripheral vascular disease, there was no apparent association between peripheral edema and cardiovascular complications such as hypertension or congestive heart failure. Peripheral edema was not associated with laboratory changes suggestive of deterioration in renal or hepatic function.
- In controlled clinical trials the incidence of peripheral edema was 6% in the LYRICA group compared with 2% in the placebo group. In controlled clinical trials, 0.5% of LYRICA patients and 0.2% placebo patients withdrew due to peripheral edema.
- Higher frequencies of weight gain and peripheral edema were observed in patients taking both LYRICA and a thiazolidinedione antidiabetic agent compared to patients taking either drug alone. The majority of patients using thiazolidinedione antidiabetic agents in the overall safety database were participants in studies of pain associated with diabetic peripheral neuropathy. In this population, peripheral edema was reported in 3% (2/60) of patients who were using thiazolidinedione antidiabetic agents only, 8% (69/859) of patients who were treated with LYRICA only, and 19% (23/120) of patients who were on both LYRICA and thiazolidinedione antidiabetic agents. Similarly, weight gain was reported in 0% (0/60) of patients on thiazolidinediones only; 4% (35/859) of patients on LYRICA only; and 7.5% (9/120) of patients on both drugs.
- As the thiazolidinedione class of antidiabetic drugs can cause weight gain and/or fluid retention, possibly exacerbating or leading to heart failure, exercise caution when co-administering LYRICA and these agents.
- Because there are limited data on congestive heart failure patients with New York Heart Association (NYHA) Class III or IV cardiac status, exercise caution when using LYRICA in these patients.
- Dizziness and Somnolence
- LYRICA may cause dizziness and somnolence. Inform patients that LYRICA-related dizziness and somnolence may impair their ability to perform tasks such as driving or operating machinery [see Patient Counseling Information (17.5)].
- In the LYRICA controlled trials, dizziness was experienced by 30% of LYRICA-treated patients compared to 8% of placebo-treated patients; somnolence was experienced by 23% of LYRICA-treated patients compared to 8% of placebo-treated patients. Dizziness and somnolence generally began shortly after the initiation of LYRICA therapy and occurred more frequently at higher doses. Dizziness and somnolence were the adverse reactions most frequently leading to withdrawal (4% each) from controlled studies. In LYRICA-treated patients reporting these adverse reactions in short-term, controlled studies, dizziness persisted until the last dose in 30% and somnolence persisted until the last dose in 42% of patients [see Drug Interactions (7)].
- Weight Gain
- LYRICA treatment may cause weight gain. In LYRICA controlled clinical trials of up to 14 weeks, a gain of 7% or more over baseline weight was observed in 9% of LYRICA-treated patients and 2% of placebo-treated patients. Few patients treated with LYRICA (0.3%) withdrew from controlled trials due to weight gain. LYRICA associated weight gain was related to dose and duration of exposure, but did not appear to be associated with baseline BMI, gender, or age. Weight gain was not limited to patients with edema [see Warnings and Precautions (5.5)].
- Although weight gain was not associated with clinically important changes in blood pressure in short-term controlled studies, the long-term cardiovascular effects of LYRICA-associated weight gain are unknown.
- Among diabetic patients, LYRICA-treated patients gained an average of 1.6 kg (range: -16 to 16 kg), compared to an average 0.3 kg (range: -10 to 9 kg) weight gain in placebo patients. In a cohort of 333 diabetic patients who received LYRICA for at least 2 years, the average weight gain was 5.2 kg.
- While the effects of LYRICA-associated weight gain on glycemic control have not been systematically assessed, in controlled and longer-term open label clinical trials with diabetic patients, LYRICA treatment did not appear to be associated with loss of glycemic control (as measured by HbA1C).
- Abrupt or Rapid Discontinuation
- Following abrupt or rapid discontinuation of LYRICA, some patients reported symptoms including insomnia, nausea, headache, anxiety, hyperhidrosis, and diarrhea. Taper LYRICA gradually over a minimum of 1 week rather than discontinuing the drug abruptly.
- Tumorigenic Potential
- In standard preclinical in vivo lifetime carcinogenicity studies of LYRICA, an unexpectedly high incidence of hemangiosarcoma was identified in two different strains of mice [see Nonclinical Toxicology (13.1)]. The clinical significance of this finding is unknown. Clinical experience during LYRICA's premarketing development provides no direct means to assess its potential for inducing tumors in humans.
- In clinical studies across various patient populations, comprising 6396 patient-years of exposure in patients >12 years of age, new or worsening-preexisting tumors were reported in 57 patients. Without knowledge of the background incidence and recurrence in similar populations not treated with LYRICA, it is impossible to know whether the incidence seen in these cohorts is or is not affected by treatment.
- Ophthalmological Effects
- In controlled studies, a higher proportion of patients treated with LYRICA reported blurred vision (7%) than did patients treated with placebo (2%), which resolved in a majority of cases with continued dosing. Less than 1% of patients discontinued LYRICA treatment due to vision-related events (primarily blurred vision).
- Prospectively planned ophthalmologic testing, including visual acuity testing, formal visual field testing and dilated funduscopic examination, was performed in over 3600 patients. In these patients, visual acuity was reduced in 7% of patients treated with LYRICA, and 5% of placebo-treated patients. Visual field changes were detected in 13% of LYRICA-treated, and 12% of placebo-treated patients. Funduscopic changes were observed in 2% of LYRICA-treated and 2% of placebo-treated patients.
- Although the clinical significance of the ophthalmologic findings is unknown, inform patients to notify their physician if changes in vision occur. If visual disturbance persists, consider further assessment. Consider more frequent assessment for patients who are already routinely monitored for ocular conditions [see Patient Counseling Information (17.8)].
- Creatine Kinase Elevations
- LYRICA treatment was associated with creatine kinase elevations. Mean changes in creatine kinase from baseline to the maximum value were 60 U/L for LYRICA-treated patients and 28 U/L for the placebo patients. In all controlled trials across multiple patient populations, 1.5% of patients on LYRICA and 0.7% of placebo patients had a value of creatine kinase at least three times the upper limit of normal. Three LYRICA treated subjects had events reported as rhabdomyolysis in premarketing clinical trials. The relationship between these myopathy events and LYRICA is not completely understood because the cases had documented factors that may have caused or contributed to these events. Instruct patients to promptly report unexplained muscle pain, tenderness, or weakness, particularly if these muscle symptoms are accompanied by malaise or fever. Discontinue treatment with LYRICA if myopathy is diagnosed or suspected or if markedly elevated creatine kinase levels occur.
- Decreased Platelet Count
- LYRICA treatment was associated with a decrease in platelet count. LYRICA-treated subjects experienced a mean maximal decrease in platelet count of 20 × 103/µL, compared to 11 × 103/µL in placebo patients. In the overall database of controlled trials, 2% of placebo patients and 3% of LYRICA patients experienced a potentially clinically significant decrease in platelets, defined as 20% below baseline value and <<<150 × 103/µL. A single LYRICA treated subject developed severe thrombocytopenia with a platelet count less than 20 × 103/ µL. In randomized controlled trials, LYRICA was not associated with an increase in bleeding-related adverse reactions.
- PR Interval Prolongation
- LYRICA treatment was associated with PR interval prolongation. In analyses of clinical trial ECG data, the mean PR interval increase was 3–6 msec at LYRICA doses ≥300 mg/day. This mean change difference was not associated with an increased risk of PR increase ≥25% from baseline, an increased percentage of subjects with on-treatment PR >200 msec, or an increased risk of adverse reactions of second or third degree AV block.
- Subgroup analyses did not identify an increased risk of PR prolongation in patients with baseline PR prolongation or in patients taking other PR prolonging medications. However, these analyses cannot be considered definitive because of the limited number of patients in these categories.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- In all controlled and uncontrolled trials across various patient populations during the premarketing development of LYRICA, more than 10,000 patients have received LYRICA. Approximately 5000 patients were treated for 6 months or more, over 3100 patients were treated for 1 year or longer, and over 1400 patients were treated for at least 2 years.
- Adverse Reactions Most Commonly Leading to Discontinuation in All Premarketing Controlled Clinical Studies
- In premarketing controlled trials of all populations combined, 14% of patients treated with LYRICA and 7% of patients treated with placebo discontinued prematurely due to adverse reactions. In the LYRICA treatment group, the adverse reactions most frequently leading to discontinuation were dizziness (4%) and somnolence (4%). In the placebo group, 1% of patients withdrew due to dizziness and <1% withdrew due to somnolence. Other adverse reactions that led to discontinuation from controlled trials more frequently in the LYRICA group compared to the placebo group were ataxia, confusion, asthenia, thinking abnormal, blurred vision, incoordination, and peripheral edema (1% each).
- Most Common Adverse Reactions in All Premarketing Controlled Clinical Studies
- In premarketing controlled trials of all patient populations combined, dizziness, somnolence, dry mouth, edema, blurred vision, weight gain, and "thinking abnormal" (primarily difficulty with concentration/attention) were more commonly reported by subjects treated with LYRICA than by subjects treated with placebo (≥5% and twice the rate of that seen in placebo).
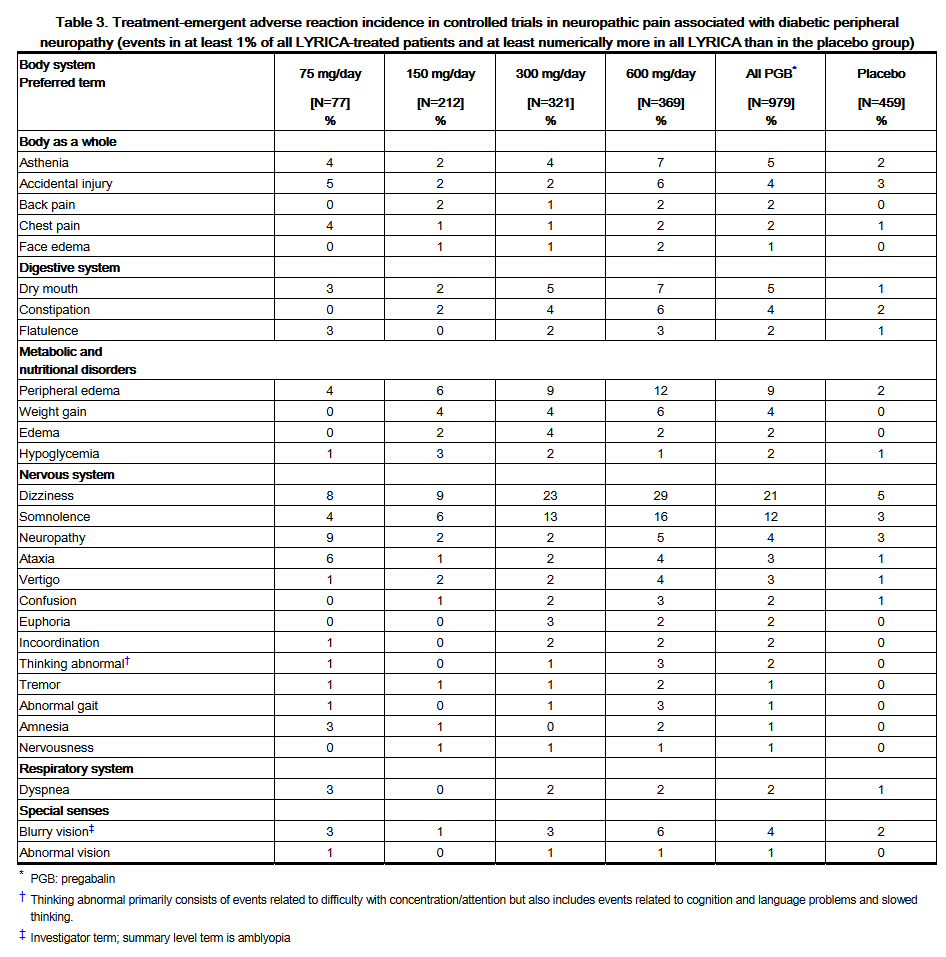
- Controlled Studies with Neuropathic Pain Associated with Diabetic Peripheral Neuropathy
- Adverse Reactions Leading to Discontinuation
- In clinical trials in patients with neuropathic pain associated with diabetic peripheral neuropathy, 9% of patients treated with LYRICA and 4% of patients treated with placebo discontinued prematurely due to adverse reactions. In the LYRICA treatment group, the most common reasons for discontinuation due to adverse reactions were dizziness (3%) and somnolence (2%). In comparison, <1% of placebo patients withdrew due to dizziness and somnolence. Other reasons for discontinuation from the trials, occurring with greater frequency in the LYRICA group than in the placebo group, were asthenia, confusion, and peripheral edema. Each of these events led to withdrawal in approximately 1% of patients.
- Most Common Adverse Reactions
- Table 3 lists all adverse reactions, regardless of causality, occurring in ≥1% of patients with neuropathic pain associated with diabetic neuropathy in the combined LYRICA group for which the incidence was greater in this combined LYRICA group than in the placebo group. A majority of pregabalin-treated patients in clinical studies had adverse reactions with a maximum intensity of "mild" or "moderate".
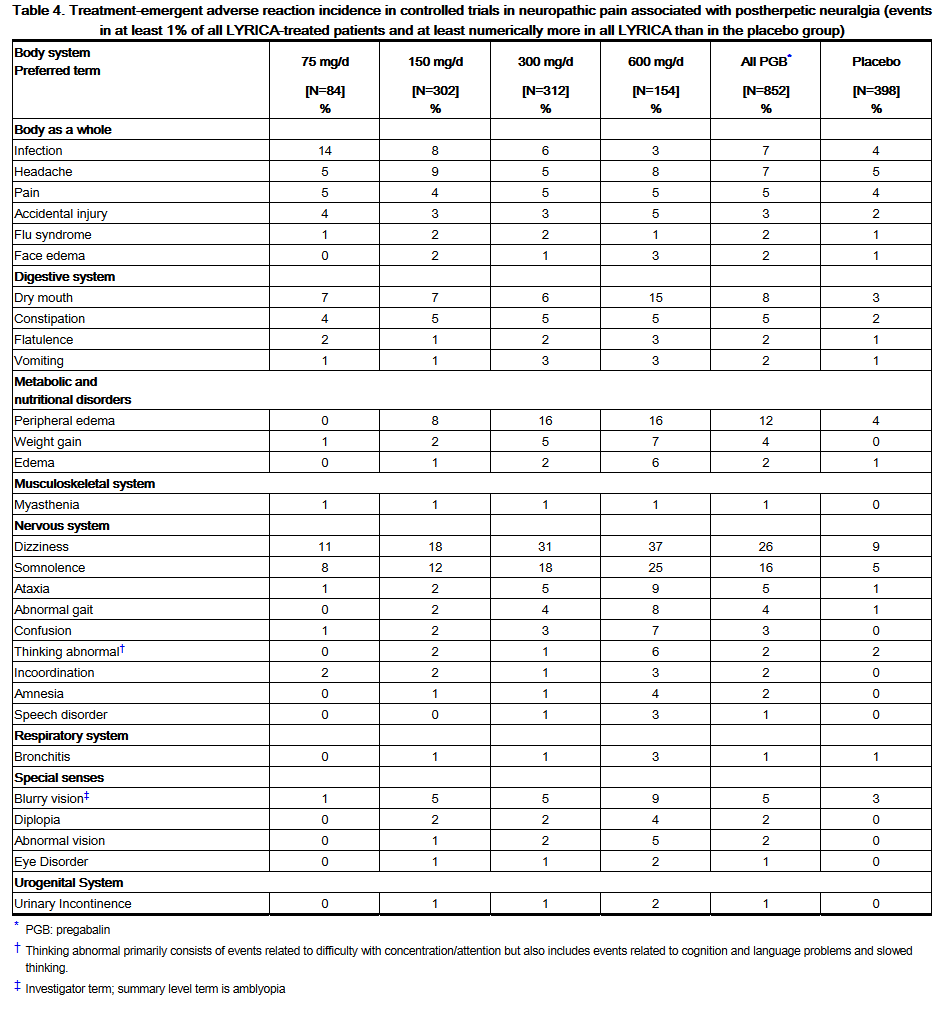
- Controlled Studies in Postherpetic Neuralgia
- Adverse Reactions Leading to Discontinuation
- In clinical trials in patients with postherpetic neuralgia, 14% of patients treated with LYRICA and 7% of patients treated with placebo discontinued prematurely due to adverse reactions. In the LYRICA treatment group, the most common reasons for discontinuation due to adverse reactions were dizziness (4%) and somnolence (3%). In comparison, less than 1% of placebo patients withdrew due to dizziness and somnolence. Other reasons for discontinuation from the trials, occurring in greater frequency in the LYRICA group than in the placebo group, were confusion (2%), as well as peripheral edema, asthenia, ataxia, and abnormal gait (1% each).
- Most Common Adverse Reactions
- Table 4 lists all adverse reactions, regardless of causality, occurring in ≥ 1% of patients with neuropathic pain associated with postherpetic neuralgia in the combined LYRICA group for which the incidence was greater in this combined LYRICA group than in the placebo group. In addition, an event is included, even if the incidence in the all LYRICA group is not greater than in the placebo group, if the incidence of the event in the 600 mg/day group is more than twice that in the placebo group. A majority of pregabalin-treated patients in clinical studies had adverse reactions with a maximum intensity of "mild" or "moderate". Overall, 12.4% of all pregabalin-treated patients and 9.0% of all placebo-treated patients had at least one severe event while 8% of pregabalin-treated patients and 4.3% of placebo-treated patients had at least one severe treatment-related adverse event.
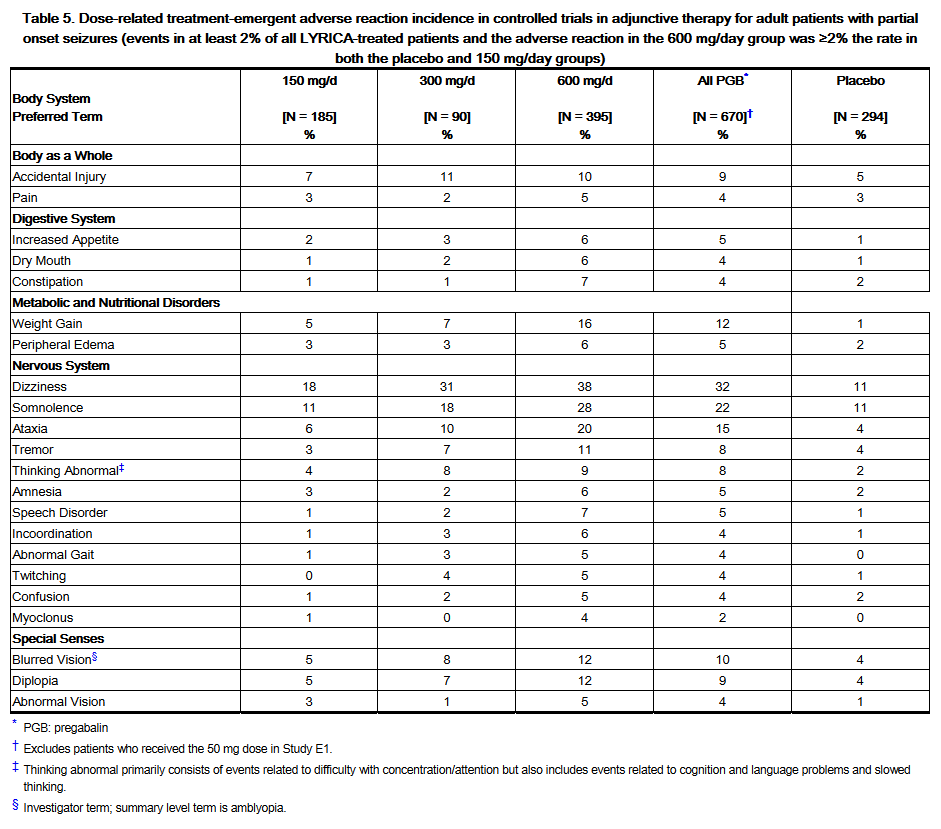
- Controlled Add-On Studies in Adjunctive Therapy for Adult Patients with Partial Onset Seizures
- Adverse Reactions Leading to Discontinuation
- Approximately 15% of patients receiving LYRICA and 6% of patients receiving placebo in add-on epilepsy trials discontinued prematurely due to adverse reactions. In the LYRICA treatment group, the adverse reactions most frequently leading to discontinuation were dizziness (6%), ataxia (4%), and somnolence (3%). In comparison, <1% of patients in the placebo group withdrew due to each of these events. Other adverse reactions that led to discontinuation of at least 1% of patients in the LYRICA group and at least twice as frequently compared to the placebo group were asthenia, diplopia, blurred vision, thinking abnormal, nausea, tremor, vertigo, headache, and confusion (which each led to withdrawal in 2% or less of patients).
- Most Common Adverse Reactions
- Table 5 lists all dose-related adverse reactions occurring in at least 2% of all LYRICA-treated patients. Dose-relatedness was defined as the incidence of the adverse event in the 600 mg/day group was at least 2% greater than the rate in both the placebo and 150 mg/day groups. In these studies, 758 patients received LYRICA and 294 patients received placebo for up to 12 weeks. Because patients were also treated with 1 to 3 other AEDs, it is not possible to determine whether the following adverse reactions can be ascribed to LYRICA alone, or the combination of LYRICA and other AEDs. A majority of pregabalin-treated patients in clinical studies had adverse reactions with a maximum intensity of "mild" or "moderate".
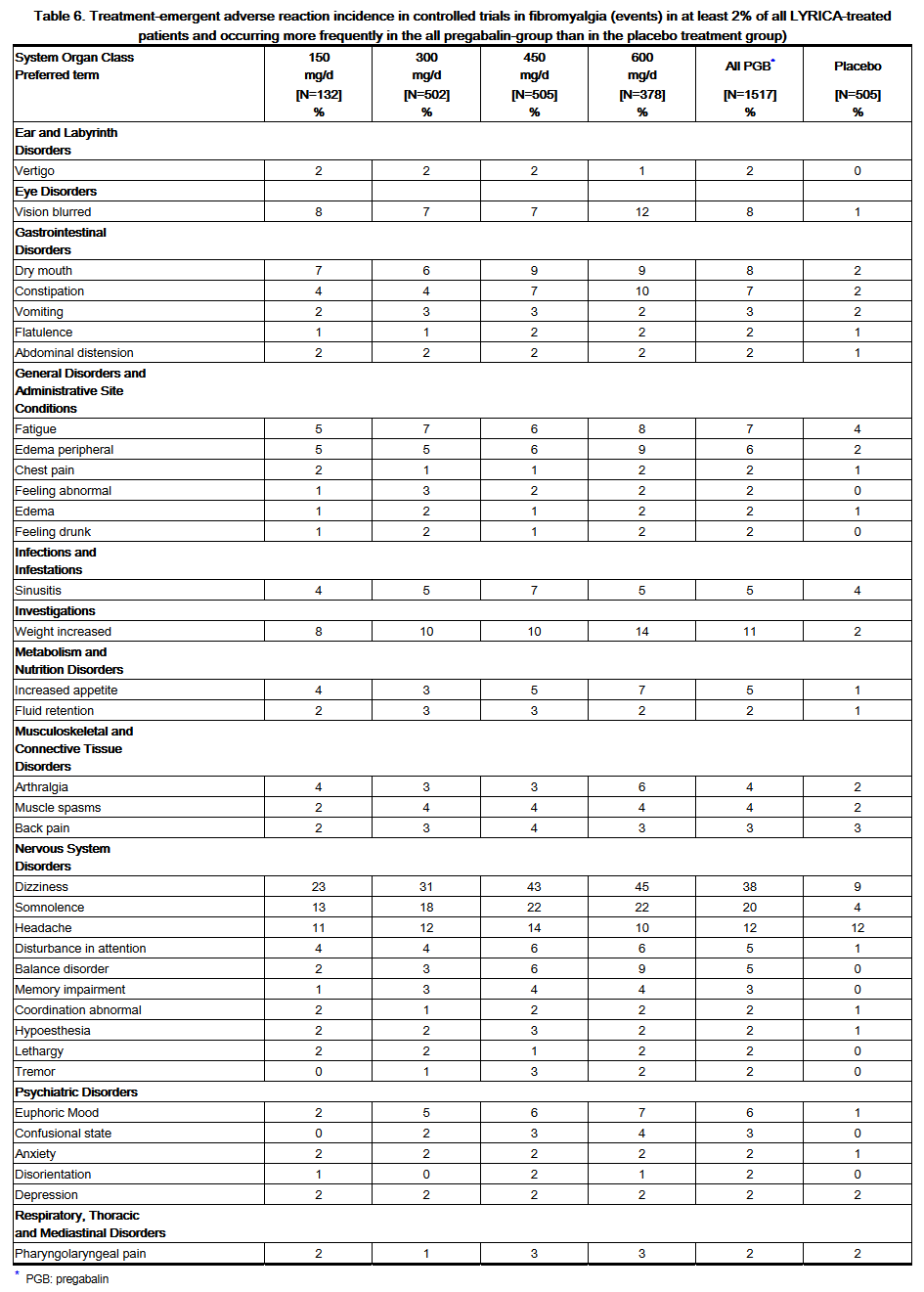
- Controlled Studies with Fibromyalgia
- Adverse Reactions Leading to Discontinuation
- In clinical trials of patients with fibromyalgia, 19% of patients treated with pregabalin (150–600 mg/day) and 10% of patients treated with placebo discontinued prematurely due to adverse reactions. In the pregabalin treatment group, the most common reasons for discontinuation due to adverse reactions were dizziness (6%) and somnolence (3%). In comparison, <1% of placebo-treated patients withdrew due to dizziness and somnolence. Other reasons for discontinuation from the trials, occurring with greater frequency in the pregabalin treatment group than in the placebo treatment group, were fatigue, headache, balance disorder, and weight increased. Each of these adverse reactions led to withdrawal in approximately 1% of patients.
- Most Common Adverse Reactions
- Table 6 lists all adverse reactions, regardless of causality, occurring in ≥2% of patients with fibromyalgia in the 'all pregabalin' treatment group for which the incidence was greater than in the placebo treatment group. A majority of pregabalin-treated patients in clinical studies experienced adverse reactions with a maximum intensity of "mild" or "moderate".
- Controlled Studies in Neuropathic Pain Associated with Spinal Cord Injury
- Adverse Reactions Leading to Discontinuation
- In clinical trials of patients with neuropathic pain associated with spinal cord injury, 13% of patients treated with pregabalin and 10% of patients treated with placebo discontinued prematurely due to adverse reactions. In the pregabalin treatment group, the most common reasons for discontinuation due to adverse reactions were somnolence (3%) and edema (2%). In comparison, none of the placebo-treated patients withdrew due to somnolence and edema. Other reasons for discontinuation from the trials, occurring with greater frequency in the pregabalin treatment group than in the placebo treatment group, were fatigue and balance disorder. Each of these adverse reactions led to withdrawal in less than 2% of patients.
- Most Common Adverse Reactions
- Table 7 lists all adverse reactions, regardless of causality, occurring in ≥2% of patients with neuropathic pain associated with spinal cord injury in the controlled trials. A majority of pregabalin-treated patients in clinical studies experienced adverse reactions with a maximum intensity of "mild" or "moderate".
Body as a Whole
Cardiovascular
Digestive
Endocrine
Hematologic and Lymphatic
Metabolic and Nutritional
Musculoskeletal
Neurologic
Respiratory
Skin and Hypersensitivy Reactions
Special Senses
Urogenital
Miscellaneous
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Pregabalin in the drug label.
Body as a Whole
Cardiovascular
Digestive
Endocrine
Hematologic and Lymphatic
Metabolic and Nutritional
Musculoskeletal
Neurologic
Respiratory
Skin and Hypersensitivy Reactions
Special Senses
Urogenital
Miscellaneous
Drug Interactions
- Drug
- Description
Use in Specific Populations
Pregnancy
- Pregnancy Category
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Pregabalin in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Pregabalin during labor and delivery.
Nursing Mothers
There is no FDA guidance on the use of Pregabalin with respect to nursing mothers.
Pediatric Use
There is no FDA guidance on the use of Pregabalin with respect to pediatric patients.
Geriatic Use
There is no FDA guidance on the use of Pregabalin with respect to geriatric patients.
Gender
There is no FDA guidance on the use of Pregabalin with respect to specific gender populations.
Race
There is no FDA guidance on the use of Pregabalin with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Pregabalin in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Pregabalin in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Pregabalin in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Pregabalin in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
- Intravenous
Monitoring
There is limited information regarding Monitoring of Pregabalin in the drug label.
- Description
IV Compatibility
There is limited information regarding IV Compatibility of Pregabalin in the drug label.
Overdosage
Acute Overdose
Signs and Symptoms
- Description
Management
- Description
Chronic Overdose
There is limited information regarding Chronic Overdose of Pregabalin in the drug label.
Pharmacology
There is limited information regarding Pregabalin Pharmacology in the drug label.
Mechanism of Action
Structure
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Pregabalin in the drug label.
Pharmacokinetics
There is limited information regarding Pharmacokinetics of Pregabalin in the drug label.
Nonclinical Toxicology
There is limited information regarding Nonclinical Toxicology of Pregabalin in the drug label.
Clinical Studies
There is limited information regarding Clinical Studies of Pregabalin in the drug label.
How Supplied
Storage
There is limited information regarding Pregabalin Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Pregabalin |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Pregabalin |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Patient Counseling Information of Pregabalin in the drug label.
Precautions with Alcohol
- Alcohol-Pregabalin interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- ®[1]
Look-Alike Drug Names
- A® — B®[2]
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Empty citation (help)
- ↑ "http://www.ismp.org". External link in
|title=(help)
{{#subobject:
|Page Name=Pregabalin |Pill Name=No image.jpg |Drug Name= |Pill Ingred=|+sep=; |Pill Imprint= |Pill Dosage= |Pill Color=|+sep=; |Pill Shape= |Pill Size (mm)= |Pill Scoring= |Pill Image= |Drug Author= |NDC=
}}
{{#subobject:
|Label Page=Pregabalin |Label Name=Pregabalin11.png
}}
{{#subobject:
|Label Page=Pregabalin |Label Name=Pregabalin11.png
}}
This image is provided by the National Library of Medicine. 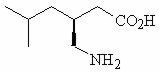
This image is provided by the National Library of Medicine. 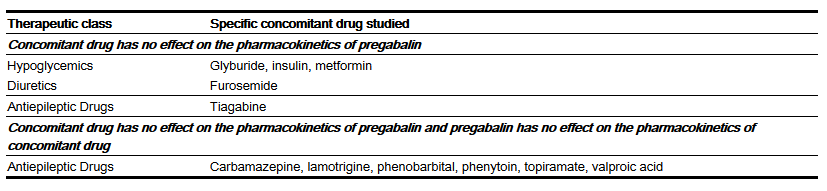
This image is provided by the National Library of Medicine. 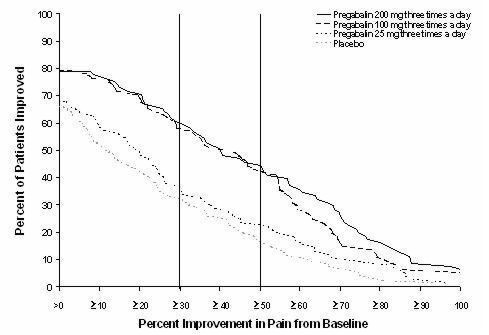
This image is provided by the National Library of Medicine. 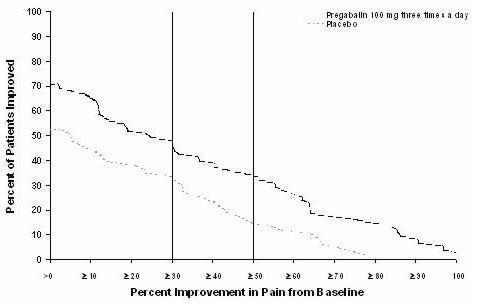
This image is provided by the National Library of Medicine. 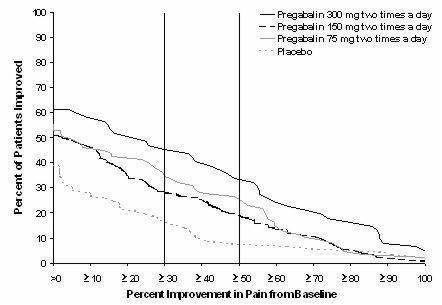
This image is provided by the National Library of Medicine. 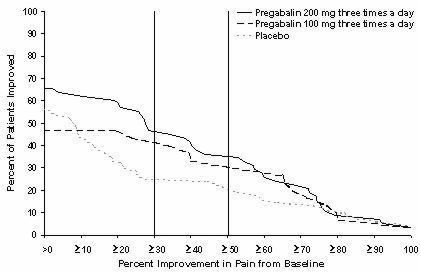
This image is provided by the National Library of Medicine. 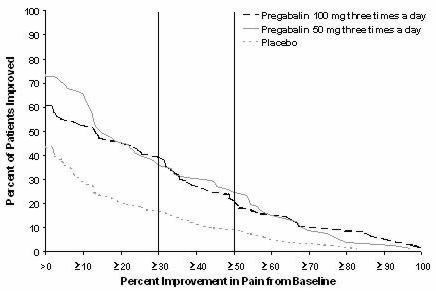
This image is provided by the National Library of Medicine. 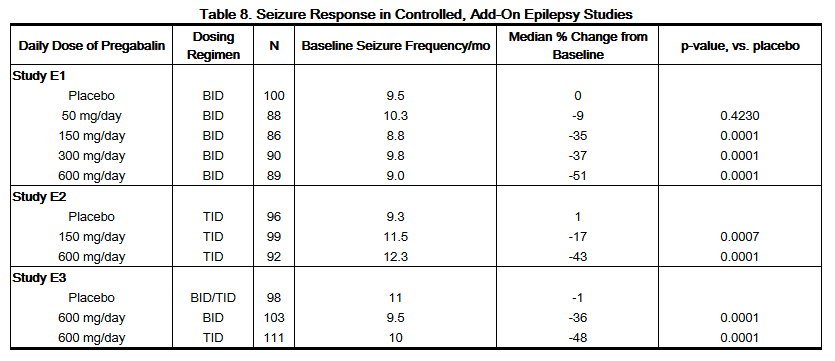
This image is provided by the National Library of Medicine. 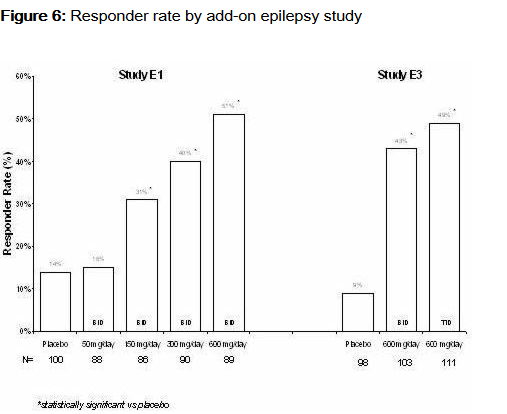
This image is provided by the National Library of Medicine. 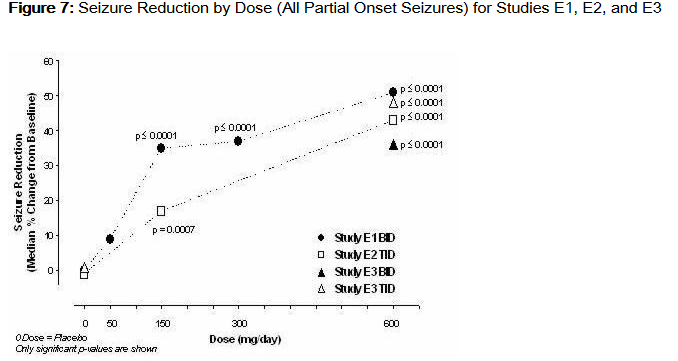
This image is provided by the National Library of Medicine. 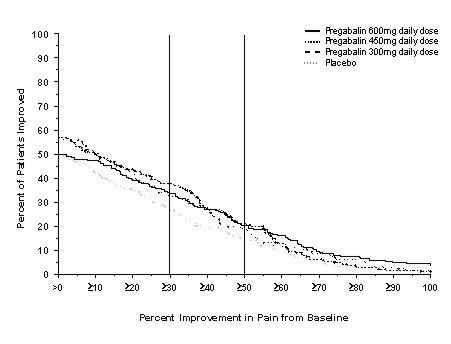
This image is provided by the National Library of Medicine. 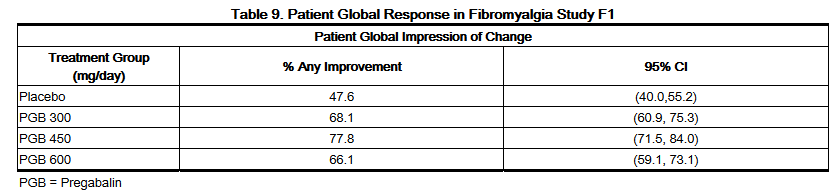
This image is provided by the National Library of Medicine. 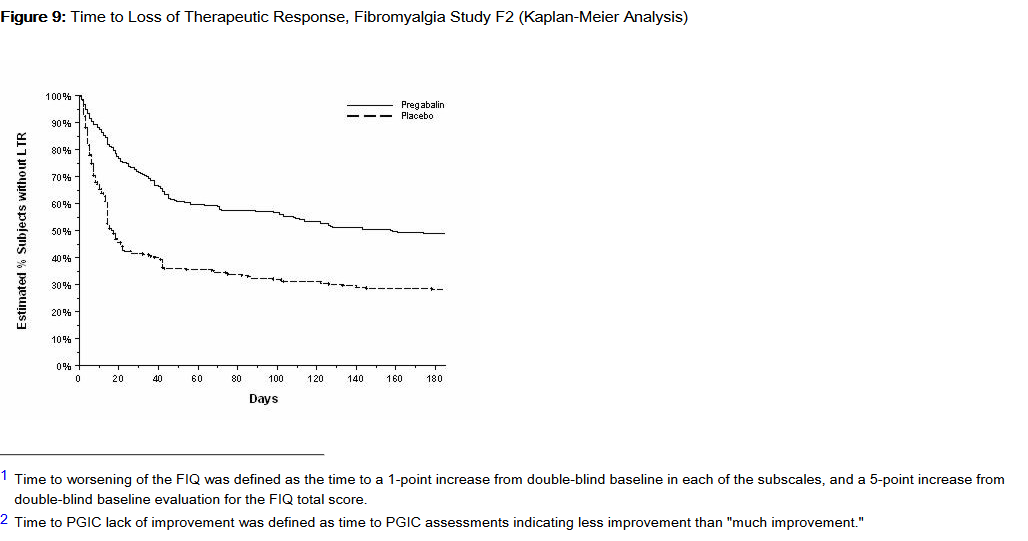
This image is provided by the National Library of Medicine. 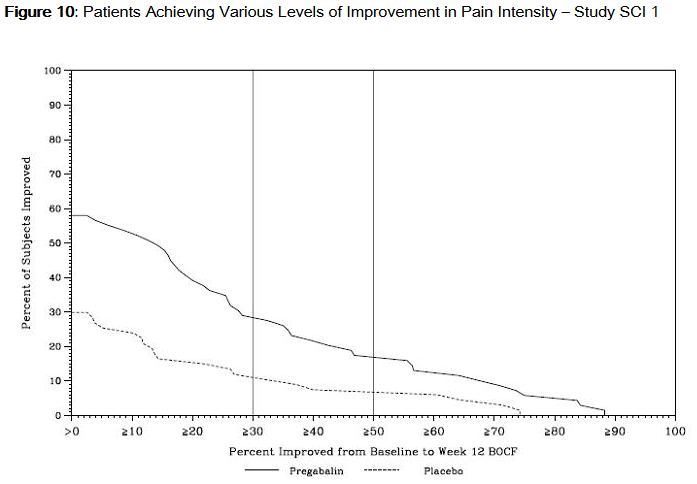
This image is provided by the National Library of Medicine. 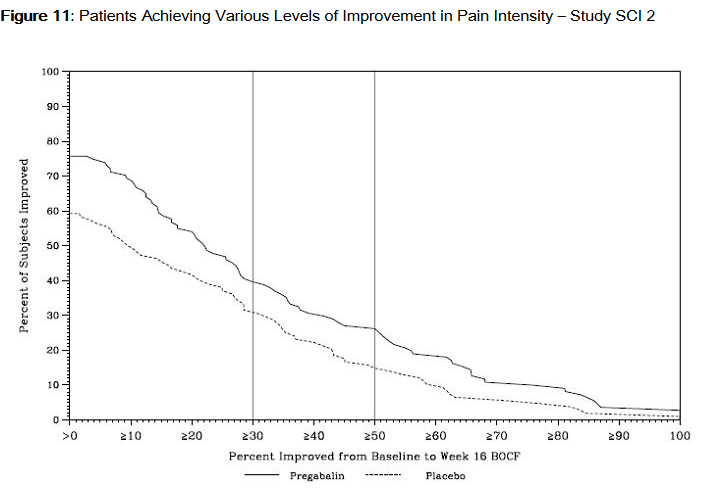
This image is provided by the National Library of Medicine. 
This image is provided by the National Library of Medicine. 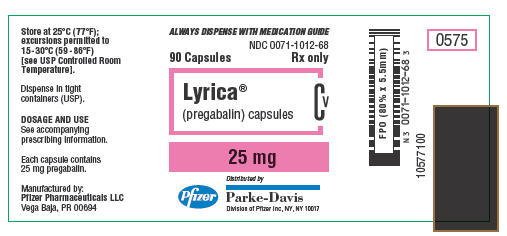
This image is provided by the National Library of Medicine. 
This image is provided by the National Library of Medicine. 
This image is provided by the National Library of Medicine. 
This image is provided by the National Library of Medicine. 
This image is provided by the National Library of Medicine.

This image is provided by the National Library of Medicine. 
This image is provided by the National Library of Medicine. 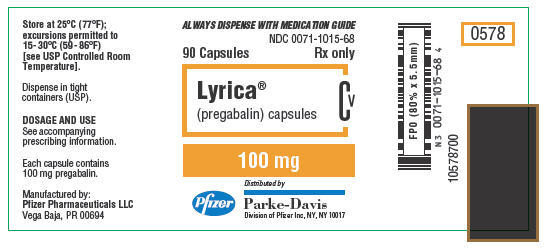
This image is provided by the National Library of Medicine. 
This image is provided by the National Library of Medicine. 
This image is provided by the National Library of Medicine. 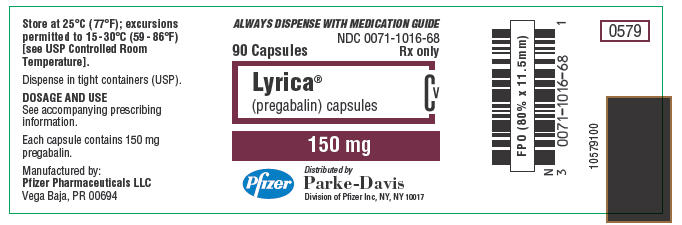
This image is provided by the National Library of Medicine. 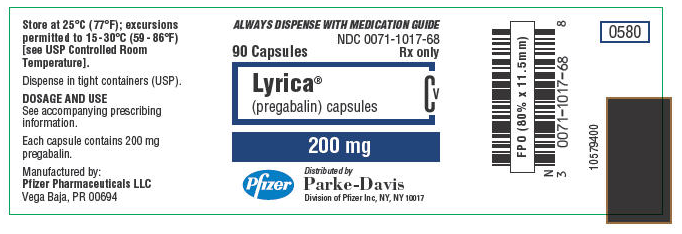
This image is provided by the National Library of Medicine. 
This image is provided by the National Library of Medicine. 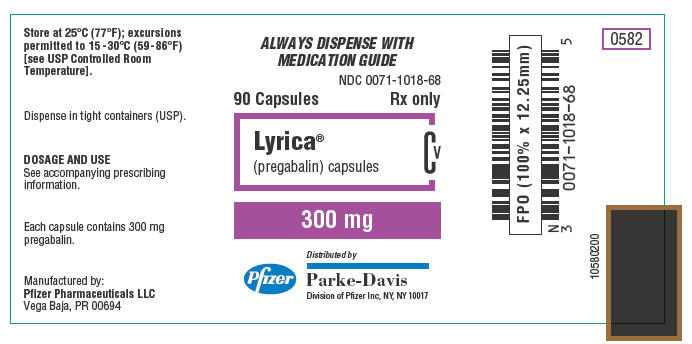
This image is provided by the National Library of Medicine. 
This image is provided by the National Library of Medicine. 
This image is provided by the National Library of Medicine. 
This image is provided by the National Library of Medicine.