Reticulocyte: Difference between revisions
No edit summary |
|||
| Line 19: | Line 19: | ||
== Overview == | == Overview == | ||
'''Reticulocytes''' are immature [[red blood cell]]s, typically composing about 1% of the red cells in the human body. | '''Reticulocytes''' are immature [[red blood cell]]s, typically composing about 1% of the red cells in the human body. | ||
Reticulocytes develop and mature in the red [[bone marrow]] and then circulate for about a day in the blood stream before developing into mature red blood cells. Like mature red blood cells, reticulocytes do not have a [[cell nucleus]]. | Reticulocytes develop and mature in the red [[bone marrow]] and then circulate for about a day in the blood stream before developing into mature red blood cells. Like mature red blood cells, reticulocytes do not have a [[cell nucleus]]. | ||
| Line 26: | Line 25: | ||
Reticulocytes appear slightly bluer than other red cells when looked at with the normal [[Romanowsky stain]]. Reticulocytes are also slightly larger, which can be picked up as a high MCV ([[mean corpuscular volume]]) with a [[full blood count]] done by a trained medical scientist, who has specialized in haematology, or a machine. <ref>[http://www.diseasesdatabase.com/index.asp The Disease Database]</ref> <ref>Sailer, Christian, Wasner, Susanne. Differential Diagnosis Pocket. Hermosa Beach, CA: Borm Bruckmeir Publishing LLC, 2002:77 ISBN 1591032016</ref> <ref>Kahan, Scott, Smith, Ellen G. In A Page: Signs and Symptoms. Malden, Massachusetts: Blackwell Publishing, 2004:68 ISBN 140510368X</ref> | Reticulocytes appear slightly bluer than other red cells when looked at with the normal [[Romanowsky stain]]. Reticulocytes are also slightly larger, which can be picked up as a high MCV ([[mean corpuscular volume]]) with a [[full blood count]] done by a trained medical scientist, who has specialized in haematology, or a machine. <ref>[http://www.diseasesdatabase.com/index.asp The Disease Database]</ref> <ref>Sailer, Christian, Wasner, Susanne. Differential Diagnosis Pocket. Hermosa Beach, CA: Borm Bruckmeir Publishing LLC, 2002:77 ISBN 1591032016</ref> <ref>Kahan, Scott, Smith, Ellen G. In A Page: Signs and Symptoms. Malden, Massachusetts: Blackwell Publishing, 2004:68 ISBN 140510368X</ref> | ||
==Differential Diagnosis of Reticulocytosis== | |||
Electromagnetic, Physics, trauma, Radiation Causes | |||
Radiation sickness/severe, acute | |||
Postirradiation effects | |||
Radiation exposure | |||
Infectious Disorders (Specific Agent) | |||
Posthepatitic aplastic anemia | |||
Parvovirus Infection/Parvovirus 19 | |||
Tuberculosis of bone marrow | |||
Infected organ, Abscesses | |||
Bacteremia/Septicemia | |||
Neoplastic Disorders | |||
Acute Myelogenous/Blastic Leukemia AML | |||
Leukemia | |||
Lymphoma/malignant, non-Hodgkins | |||
Myeloproliferative disease | |||
Primary Myelofibrosis/Myeloid metaplasia | |||
Metabolic, Storage Disorders | |||
Impaired folic acid metabolism | |||
Deficiency Disorders | |||
Anemia of malnutrition | |||
Folate depletion | |||
Folic acid deficiency anemia | |||
Inadequate Folic acid in diet | |||
Iron deficiency anemia | |||
Iron deficient diet | |||
Malnutrition/Starvation | |||
Folic acid dependency/metabolic defect | |||
Kwashiorkor (protein deficiency,severe) | |||
Malabsorption of folic acid | |||
Pellagra/niacin deficiency | |||
Vitamin B12 deficiency | |||
Congenital, Developmental Disorders | |||
Klinefelter's syndrome | |||
Anemia, congenital aplastic | |||
Folate malabsorption, congenital | |||
Hereditary, Familial, Genetic Disorders | |||
Thalassemia major | |||
Thalassemia minor | |||
Hereditary sideroblastic anemia | |||
Hemoglobin H disease | |||
Elliptocytosis, hereditary | |||
Fanconi's pancytopenia-dysmelia synd | |||
Thalassemia-hemoglobin C disease | |||
Vegetative, Autonomic, Endocrine Disorders | |||
Hypothyroidism (myxedema) | |||
Addison's disease (chronic adrenal ins) | |||
Hypogonadism, male/androgen deficiency | |||
Adrenocorticoid (Isolated) Deficiency | |||
Reference to Organ System | |||
Liver disease/Liver disorders | |||
Anemia of chronic disease | |||
Anemia of uremia | |||
Anemia, megaloblastic of pregnancy | |||
Chronic liver disease | |||
Megaloblastic anemia | |||
Anemia, aplastic | |||
Aplastic anemia crisis | |||
Myelophthisic anemia | |||
Renal Failure Chronic | |||
Acquired sideroblastic anemia | |||
Pernicious anemia | |||
Combined system disease/pernicious an. | |||
Myelofibrosis, secondary | |||
Refractory megaloblastic anemia | |||
Sideroblastic Anemia Siderochrestic | |||
Pathophysiologic | |||
Myeloid metaplasia pathophysiology | |||
Drugs | |||
Antimetabolite medication Administration/Toxicity | |||
Methotrexate (Rheumatrex) Administration/Toxicity | |||
Chemotherapy, cancer (anti-neoplastic) | |||
Drug induced Bone marrow suppression. | |||
Drug induced anemia | |||
Poisoning (Specific Agent) | |||
Lead poisoning in children | |||
Alcoholism, chronic | |||
Tetraethyl lead poisoning | |||
Lead poisoning | |||
==Reticulocyte count== | ==Reticulocyte count== | ||
The reticulocyte count is the percentage of circulating red blood cells that are in the reticulocyte stage. | The reticulocyte count is the percentage of circulating red blood cells that are in the reticulocyte stage. | ||
Revision as of 11:59, 15 April 2012
| Reticulocyte | |
 | |
|---|---|
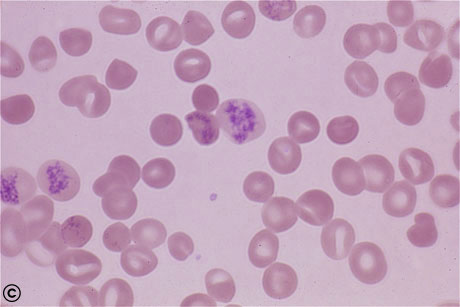
| Peripheral blood; Reticulocyte. © Image courtesy of Nivaldo Medeiros MD and published with permission |
|
WikiDoc Resources for Reticulocyte |
|
Articles |
|---|
|
Most recent articles on Reticulocyte Most cited articles on Reticulocyte |
|
Media |
|
Powerpoint slides on Reticulocyte |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Reticulocyte at Clinical Trials.gov Clinical Trials on Reticulocyte at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Reticulocyte
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Reticulocyte Discussion groups on Reticulocyte Patient Handouts on Reticulocyte Directions to Hospitals Treating Reticulocyte Risk calculators and risk factors for Reticulocyte
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Reticulocyte |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
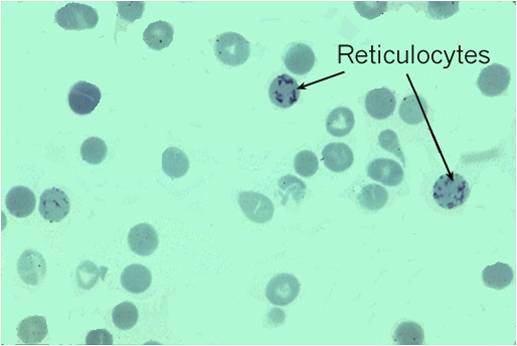
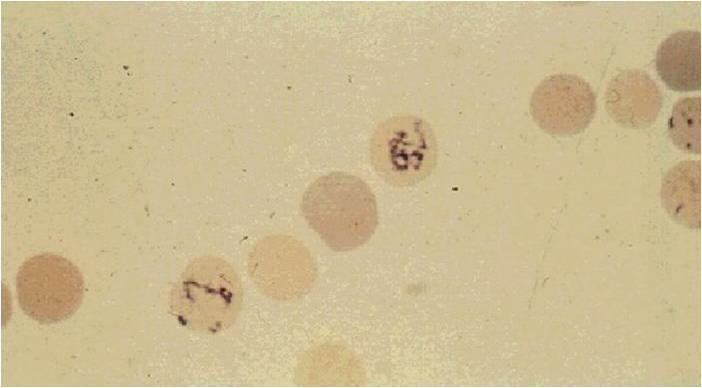
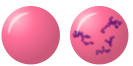
Reticulocytes are immature red blood cells, typically composing about 1% of the red cells in the human body. Reticulocytes develop and mature in the red bone marrow and then circulate for about a day in the blood stream before developing into mature red blood cells. Like mature red blood cells, reticulocytes do not have a cell nucleus. They are called reticulocytes because of a reticular (mesh-like) network of ribosomal RNA that becomes visible under a microscope with certain stains such as new methylene blue.
Reticulocytes appear slightly bluer than other red cells when looked at with the normal Romanowsky stain. Reticulocytes are also slightly larger, which can be picked up as a high MCV (mean corpuscular volume) with a full blood count done by a trained medical scientist, who has specialized in haematology, or a machine. [1] [2] [3]
Differential Diagnosis of Reticulocytosis
Electromagnetic, Physics, trauma, Radiation Causes Radiation sickness/severe, acute Postirradiation effects Radiation exposure Infectious Disorders (Specific Agent) Posthepatitic aplastic anemia Parvovirus Infection/Parvovirus 19 Tuberculosis of bone marrow Infected organ, Abscesses Bacteremia/Septicemia Neoplastic Disorders Acute Myelogenous/Blastic Leukemia AML Leukemia Lymphoma/malignant, non-Hodgkins Myeloproliferative disease Primary Myelofibrosis/Myeloid metaplasia Metabolic, Storage Disorders Impaired folic acid metabolism Deficiency Disorders Anemia of malnutrition Folate depletion Folic acid deficiency anemia Inadequate Folic acid in diet Iron deficiency anemia Iron deficient diet Malnutrition/Starvation Folic acid dependency/metabolic defect Kwashiorkor (protein deficiency,severe) Malabsorption of folic acid Pellagra/niacin deficiency Vitamin B12 deficiency Congenital, Developmental Disorders Klinefelter's syndrome Anemia, congenital aplastic Folate malabsorption, congenital Hereditary, Familial, Genetic Disorders Thalassemia major Thalassemia minor Hereditary sideroblastic anemia Hemoglobin H disease Elliptocytosis, hereditary Fanconi's pancytopenia-dysmelia synd Thalassemia-hemoglobin C disease Vegetative, Autonomic, Endocrine Disorders Hypothyroidism (myxedema) Addison's disease (chronic adrenal ins) Hypogonadism, male/androgen deficiency Adrenocorticoid (Isolated) Deficiency Reference to Organ System Liver disease/Liver disorders Anemia of chronic disease Anemia of uremia Anemia, megaloblastic of pregnancy Chronic liver disease Megaloblastic anemia Anemia, aplastic Aplastic anemia crisis Myelophthisic anemia Renal Failure Chronic Acquired sideroblastic anemia Pernicious anemia Combined system disease/pernicious an. Myelofibrosis, secondary Refractory megaloblastic anemia Sideroblastic Anemia Siderochrestic Pathophysiologic Myeloid metaplasia pathophysiology Drugs Antimetabolite medication Administration/Toxicity Methotrexate (Rheumatrex) Administration/Toxicity Chemotherapy, cancer (anti-neoplastic) Drug induced Bone marrow suppression. Drug induced anemia Poisoning (Specific Agent) Lead poisoning in children Alcoholism, chronic Tetraethyl lead poisoning Lead poisoning
Reticulocyte count
The reticulocyte count is the percentage of circulating red blood cells that are in the reticulocyte stage.
To accurately measure reticulocyte counts, automated counters that use lasers mark cell samples with fluorescent dye that marks RNA and DNA (such as thiazole orange).[4] This distinguishes reticulocytes as the middle ground of dye response to laser light, between red blood cells (which have neither RNA nor DNA) and lymphocytes (which have a large amount of DNA, unlike reticulocytes).[5]
The normal range of values for reticulocytes in the blood depends on the clinical situation and the lab, but broadly speaking is 0.5% to 1.5%. However, if a person has anaemia, their reticulocyte percentage should be higher than "normal" if the bone marrow's ability to produce new blood cells remains intact. Thus, calculating the reticulocyte production index is an important step in understanding whether the reticulocyte count is appropriate or inappropriate to the situation. This is often a more important question than whether the percentage is in the normal range; for instance, if someone is anemic but only has a reticulocyte percentage of 1%, this means that the bone marrow is likely not producing new blood cells at a rate that will correct the anemia. The number of reticulocytes is a good indicator of bone marrow activity, because it represents recent production. This means that the reticulocyte count, and the reticulocyte production index that can be calculated from it, can be used to determine whether a production problem is contributing to the anaemia, and can also be used to monitor the progress of treatment for anaemia.
The specimen requirement for a reticulocyte count is EDTA anti-coagulated whole blood (lavender-top bottle if using the Vacutainer®, Vacuette® or Monoject® systems; red-top if using the S-Monovette® system).
When there is an increased production of red blood cells to overcome chronic or severe loss of mature red blood cells, such as in a haemolytic anaemia, people often have a markedly high number and percentage of reticulocytes. A very high number of reticulocytes in the blood can be described as reticulocytosis.
Abnormally low numbers of reticulocytes can be attributed to chemotherapy, aplastic anaemia, pernicious anaemia, bone marrow malignancies, problems of erythropoietin production, or other causes of anaemia due to poor RBC production.
-
Reticulocyte (Courtesy of Melih Aktan M.D.)
-
Reticulocyte (Courtesy of Melih Aktan M.D.)
See also
References
- ↑ The Disease Database
- ↑ Sailer, Christian, Wasner, Susanne. Differential Diagnosis Pocket. Hermosa Beach, CA: Borm Bruckmeir Publishing LLC, 2002:77 ISBN 1591032016
- ↑ Kahan, Scott, Smith, Ellen G. In A Page: Signs and Symptoms. Malden, Massachusetts: Blackwell Publishing, 2004:68 ISBN 140510368X
- ↑ Davis BH, Bigelow NC (1994). "Reticulocyte analysis and reticulocute maturity index". In Darzynkiewicz Z, Crissman HA (eds.). Flow cytometry. Methods in Cell Biology. 42. San Diego: Academic Press. pp. 263&ndash, 74. ISBN 0-12203-052-4.
- ↑ http://www.medicaldesign.com/articles/ID/532
Template:Blood Template:SIB he:רטיקולוציט id:Retikulosit fi:Retikulosyytti sq:Retikulociti