Venous insufficiency: Difference between revisions
No edit summary |
Kiran Singh (talk | contribs) |
||
| Line 337: | Line 337: | ||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
[[Category:Physical examination]] | [[Category:Physical examination]] | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
Revision as of 16:37, 16 June 2015
| Venous insufficiency | |
 | |
|---|---|
| Venous insufficiency |
Editor-in-Chief: Robert G. Schwartz, M.D. [5], Piedmont Physical Medicine and Rehabilitation, P.A.; Michael Traurig, M.D., Vein Centers of Excellence, Greenville, SC; Associate Editor(s)-In-Chief:: C. Michael Gibson, M.S., M.D.; Cafer Zorkun, M.D., Ph.D. [6]
Overview
Venous insufficiency is a condition in which the veins do not efficiently return blood from the lower limbs back to the heart. Venous insufficiency involves one or more veins.
Normal Anatomy and Function
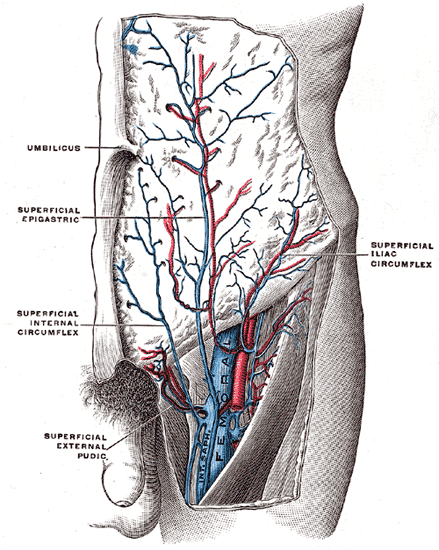
- The superficial veins lie in the subcutaneous fatty layer of the body just beneath the skin and superficial to the deep fascia enveloping the body musculature. The principal veins in the legs are the great and lesser saphenous veins and their tributaries; in the arms they are the basilic and cephalic veins and their tributaries.
- The deep veins accompany arteries and bear the same name as the arteries they parallel. It is common in the extremities for there to be two or more veins accompanying a small to medium sized artery.
- The perforating veins penetrate the deep fascia and connect the superficial veins to the deep veins. Those along the inner (medial) side of the lower leg play a major role in the pathogenesis of the postphlebitic leg.
- The intramuscular sinusoidal veins are large, very thin walled, valveless veins within skeletal muscle. They connect directly with the deep veins.
-
Great saphenous vein
-
Small saphenous vein and its tributaries.
-
The femoral vein and its tributaries.
Function

Veins serve to return blood from organs to the heart.
In systemic circulation oxygenated blood is pumped by the left ventricle through the arteries to the muscles and organs of the body, where its nutrients and gases are exchanged at capillaries, entering the veins filled with cellular waste and carbon dioxide.
The de-oxygenated blood is taken by veins to the right atrium of the heart, which transfers the blood to the right ventricle, where it is then pumped to the pulmonary arteries and eventually the lungs.
In pulmonary circulation the pulmonary veins return oxygenated blood from the lungs to the left atrium, which empties into the left ventricle, completing the cycle of blood circulation. Normal venous flow is dependent on four factors:
- Dynamic Flow: The heart related flow (dynamics / spontaneous flow). Flow in the arterial system is dependent on the pumping action of the heart and the elasticity and muscular activity of the arteries.
- Phasic Flow: The breathing-related intra-abdominal pressure changes lead to respiratory fluctuation of venous flow with faster flow during expiration due to lower intraabdominal pressure (upward movement of diaphragm) and slower flow during inspiration due to higher intraabdominal pressure (downward movement of diaphragm). This pressure dependent flow pattern is transmitted through the upper leg veins into the major deep veins in the distal lower leg and into the major superficial veins (great and small saphenous veins) in the recumbent patient.
- The muscle pump or the venous pump: The muscle pump mechanism is highly developed in the calf muscles. Large venous sinusoids located in these muscles. As they contract, the force helps to emptying the below veins. Contractions of the calf muscles can produce a sufficient pressure to empty the sinusoids into the deep veins. The deep veins are affected with the similar compressing force due to a strong fascial structure. As a result, with each muscle contraction venous blood is pumped towards to the heart.
- The valves: The valves are prevent retrograde flow. They prevent retrograde flow from heart to veins and from deep veins to superfacial veins.
Classification
CEAP Classification: Clinical Presentation, Etiology, Anatomical Localization, Pathophysiological Dysfunction
- According to Clinical Presentation
- Asymptomatic
- Symptomatic
- According to Etiology
- Congenital
- Primary
- Secondary)
- According to Anatomical Localization / Distribution
- Superficial
- Deep
- Perforator
- Alone
- In combination
- According to Pathophysiological Dysfunction
- Reflux
- Obstruction
- Alone
- In combination
Evaluation
- Class 0: No evidence of venous disease.
- Class 1: Telangiectasia (Superficial spider veins), reticular veins, malleolar flare
- Class 2: Simple varicose veins only
- Class 3: Ankle oedema of venous origin (not foot edema)
- Class 4: Skin pigmentation in the gaiter area (lipodermatosclerosis)
- Class 5: Dermatological changes with a healed venous ulcer
- Class 6: Dermatological changes with an open (active) venous ulcer
Pathophysiology

Disturbed venous return from peripheral veins) can have the following causes:
- Impairment of the calf muscle pump
- Obstruction of the deep veins
- Valve incompetence of the epifascial veins
- Valve incompetence of the perforating veins
- Valve incompetence of the subfascial veins
Causes of Venous Insufficiency
Risk Factors
- Ageing
- Family history
- Female hormones
- Gravitational hydrostatic forces (exacerbated during pregnancy)
- Hydrostatic muscular compartment force
- Sedentary lifestyle
Diagnosis
Clinical manifestations of venous insufficiency include various conditions such as telangiectasias, varicose veins, and axial incompetence. These are easily treated. In contrast, venous insufficiency may be refractory to treatment as in the severely damaged postthrombotic limb which manifests segmental occlusion in combination with universal venous reflux. Venous Duplex Ultrasonography is commonly used to diagnose venous reflux.
Signs and Symptoms
- Leg discomfort and / or pain: Complains may include dull aching, heaviness, or cramping. Venous claudication may mimic arterial intermittent claudication, though it typically takes longer to subside after stopping exercise.
- Skin pigmentation and discoloration of the skin. Venous insufficiency is characterized by a dark bluish / purple discoloration. Over time, long standing stasis of blood leads to the deposition of hemosiderin, giving the skin a dark, speckled appearance. If the leg is placed in a dependent position, the bluish/purple discoloration may darken dramatically, further suggestive of venous insufficiency. This occurs as a result of gravity working against an already ineffective blood return system. Patients with severe arterial insufficiency, on the other hand, may have relatively pale skin as a result of under perfusion. When their legs are placed in a dependent position, gravity enhances arterial inflow and the skin may become more red as maximally dilated arterioles attempt to bring blood to otherwise starved tissues. In cases of severe ischemia, the affected areas (usually involving the most distal aspect of the foot), can appear whitish or mottled, giving the leg a marbleized appearance. Dead tissue turns black (a.k.a. gangrene). Cellulitis (infection in the skin) will cause the skin to appear bright red. These changes can be difficult to detect in people of color.
- Ulceration: Non-healing ulcers especially around the medial malleolus
- Lipodermatosclerosis: LDS or liposclerosis refers to a thickening in the tissues underneath the skin.
- Varicose eczema: the skin becomes red, wet and scaly.
- Leg swelling
Physical Examination
- Auscultation findings of arteriovenous fistulas may be present
- Increased skin temperature may found
- Thin skin: Sign of poor skin nutrition.
-
Venous insufficiency
-
Assymetric Leg, Swelling secondary to Deep Venous Thrombosis in Right Leg
-
Venous Stasis Ulcer
-
Edema of Right Foot
-
Massive edema
Tourniquet tests
Performing a Tourniquet test is necessary to determine the level of valvular incompetence in the superficial system and to ascertain whether deep venous system involvement is present. Tourniquet test is developed by Brody and later on modified by Trendelenburg.
The patient should wait in a supine position with the limb elevated for at least one minute before starting to perform the Tourniquet test. This maneuver empties the veins by reducing venous congestion in the superficial venous system. Four tourniquets are then placed at the upper thigh, lower thigh, calf, and upper ankle.
Then ask to patient to stand. If the superficial veins of the calf segment fill, perforating vein incompetence is usually present. The tourniquets are then removed from the bottom upward. If removing the ankle tourniquet fills the superficial venous system, presence of perforating vein incompetence is suspected.
If after removal of the below-knee tourniquet the lesser saphenous system fills, then presence of lesser saphenous incompetence is most likely. In following step, the above-knee tourniquet is removed to assess the competence of the Hunter's canal perforator. At the end, if the superficial venous system remains empty, then the high thigh tourniquet is removed to detect saphenofemoral incompetence.
Trendelenburg test
A Trendelenburg test determines the competency of the valves in communicating veins between the superficial and deep veins of the leg. The leg is raised above heart level until the veins become empty, then the leg is quickly lowered. Superficial veins of the leg normally empty into deep veins, however retrograde filling occurs when valves are incompetent, leading to varicose veins.
The Trendelenburg test is often confused with Trendelenburg's sign, which is related to conditions affecting the hip and femur.
Perthes test
The Perthes test is a clinical test for assessing the patency of the deep femoral vein prior to varicose vein surgery. It is named after German surgeon Georg Perthes.
The limb is elevated and an elastic bandage is applied firmly from the toes to the upper 1/3 of the thigh to obliterate the superficial veins only.
With the bandage applied the patient is asked to walk for 5 minutes. If deep system is competent, the blood will go through and back to the heart. If the deep system is incompetent, the patient will feel pain in the leg.
This test is sometimes referred to as the Delbet-Mocquot test, named after French physicians Pierre Delbet and Pierre Mocquot.
Modified Perthes test
The test in done by applying a tourniquet at the level of the saphenofemoral junction to occlude the superficial pathway, and then the patient is asked to move in situ. If the deep veins are occluded, the dilated veins increase in prominence and pain occurs.
This is a more reliable test as it does not depend on patient's pain threshold.
Ultrasonography
Gray scale ultrasonography (Compress ultrasonography)
Color Doppler Ultrasonography
Duplex scanning of the deep and superficial veins can detect obstruction. In addition, the function of valves in each segment of the evaluated veins can be assessed by determining the direction of blood-flow using Doppler ultrasound. Function of the proximal valves is evaluated during Valsalva maneuver in the recumbent patient and Doppler sampling in the common and superficial femoral veins during increased abdominal pressure.
The examination is often done in the upright position, as this is the best way to evaluate valve function.
Landmarks for venous reflux examination:
- Common femoral vein
- Femoral vein
- Upper third part
- Distal third part
- Popliteal vein
- Gastrocnemius veins
- Saphenofemoral junction
- Saphenous vein (above the knee)
- Saphenous vein (below the knee)
- Saphenopopliteal junction
- Mode of termination, short saphenous vein
Therapeutic decision depends on color flow duplex ultrasound evaluation results. Following an examination there are four main levels of venous pathology:
- Superficial venous reflux only
- Deep venous reflux only
- Mixed superficial and deep venous reflux
- Occluded deep venous system
Photoplethysmography (PPG)
Air Plethysmography (APG)
Mercury Strain-gauge Plethysmography
Real-Time Digital Phlebography
Light Reflection Rheography
MRI
MRI provides sagittal, coronal, and cross-sectional views and is able to detect acute occlusion.
Computed Tomography
Phlebography
- Ascending
- Descending
Thermography
Thermography provides an infrared map of cutaneous temperature and can be used to help identify suferficial and perforating veins.
Treatment
Conservative treatment
The symptoms of varicose veins can be controlled to an extent with the following:
- Elevating the legs often provides temporary symptomatic relief.
- "Advice about regular exercise sounds sensible but is not supported by any evidence."[1]
- The wearing of graduated compression stockings with a pressure of 30–40 mmHg has been shown to correct the swelling, nutritional exchange, and improve the microcirculation in legs affected by varicose veins.[2] They also often provide relief from the discomfort associated with this disease. Caution should be exercised in their use in patients with concurrent arterial disease.
- Anti-inflammatory medication such as ibuprofen or aspirin can be used as part of treatment for superficial thrombophlebitis along with graduated compression hosiery – but there is a risk of intestinal bleeding. In extensive superficial thrombophlebitis, consideration should be given to anti-coagulation, thrombectomy or sclerotherapy of the involved vein.
- Diosmin 95 is a dietary supplement distributed in the U.S. by Nutratech, Inc. The U.S. Food and Drug Administration does not approve dietary supplements, and concluded that there was an "inadequate basis for reasonable expectation of safety." [3] [4]
- Lumbrokinase (Bolouke) is another dietary supplement. It has phase II and III clinical trials that demonstrate its effectiveness as a fibrinolytic agent. Lumbrokinase has been used successfully in cases of venous insufficiency where "cleaning of the valves" might be of help in restoring valve function and anatomy [7]
- More aggresive thrombolytic therapy with injectable low molecular weight heparins (such as lovenox or arixtra) can also reduce fibrin formation and has been successfully clinically to reduce the signs and symptoms of venous insufficiency [8].
Compression Therapy: External banding to restore saphenous competence
- Graduated compression stockings
- Custom made
- Standard size
- Knee length
- Thigh length
- Compression tights
- Bandages
- Single component
- Multiple components
- Inelastic
- Elastic
- Intermittent pneumatic compression
- Single chamber
- Sequential chambers
- Foot-pump
- Lower leg
- Full leg & trunk
Stent Application
Self-expanding metallic stents are used in venous stenting.
Hemodynamic correction of varicose veins (CHIVA)
CHIVA is the acronym for Conservative and Hemodynamic cure of Incompetent Varicose veins in Ambulatory patients translated from the French cure Conservatrice et Hémodynamique de l'Insuffisance Veineuse en Ambulatoire[5] published in France in 1988.
- Pathophysiological principles
CHIVA relies on an hemodynamic impairment assessed by data and evidences depicted through Ultrasound dynamic venous investigations. According to this new concept, the clinical symptoms of venous insufficiency are not the cause but the consequence of various abnormalities of the venous system. For example,a varicose vein being overloaded, may be dilated not only because of valvular incompetence (the most frequent) but because of a venous block (thombosis) or arterio-venous fistula, and so the treatment has to be tailored according the hemodynamic feature.
- Procedure and outcomes
It generally consists in 1 to 4 small incisions under local anesthesia in order to disconnect the varicose veins from the abnormal flow due to valvular incompetence which dilates them.[6] The patient is dismissed the same day. This method leads to an improvement of the venous function in order to:
- Cure the symptoms of venous insufficiency as varicose veins, legs swelling, ulcers.[7] [8]
- Prevent varicose recurrence due to progressive enlargement of collateral veins which replace and overtake the destroyed veins: CHIVA vs Stripping: varicose recurrence divided by 2 to 5 at 10 years.[9]
- Preserve the superficial venous capital for unpredictable but possible need for coronary or leg artery vital by-pass which increases with ageing.
- Consequences to be achieved properly, CHIVA method needs a comprehensive knowledge of both hemodynamics and Ultrasound venous investigation.
Surgery
- Superficial Venous Stripping: Stripping consists in a removal of all the saphena vein main trunk from the groin down to the ankle.The complications include deep vein thrombosis (5.3%),[10] pulmonary embolism (0.06%), and wound complications including infection (2.2%). For traditional surgery, reported recurrence rates, which have been tracked for 10 years, range from 5-60%. In addition, since stripping removes the saphenous main trunks, they are no longer availlable for venous by-pass in the future (coronary and/or leg artery vital disease)[11]
- Conventional surgery: Conventional surgery for varicose veins does relieve symptoms and has a role on the prevention of chronic venous ulceration.
- Valve repair techniques
- Techniques with Phlebotomy
- Internal Valvuloplasty
- Venous Segment Transfer
- Vein Valve Transplantation
- Neo Valve
- Allograft Cryopreserved Valve
- Techniques without Phlebotomy
- Wrapping, Banding, Cuffing, and External Stenting
- External Valvuloplasty
- Transmural Valvuloplasty
- Transcommissural Valvuloplasty
- Angioscopy-Assisted External Valve Repair
- Percutaneously placed device
- The Portland valve
Sclerotherapy
- Conventional Sclerotherapy
- Foam Sclerotherapy
A commonly performed non-surgical treatment for varicose and "spider" leg veins is sclerotherapy. It has been used in the treatment of varicose veins for over 150 years.[12] Sclerotherapy is often used for telangiectasias (spider veins) and varicose veins that persist or recur after vein stripping.[13][14] Sclerotherapy can also be performed using microfoam sclerosants under ultrasound guidance to treat larger varicose veins, including the greater and short saphenous veins.[15][16] A study by Kanter and Thibault in 1996 reported a 76% success rate at 24 months in treating saphenofemoral junction and great saphenous vein incompetence with STS 3% solution.[17] A Cochrane Collaboration review[18] concluded sclerotherapy was better than surgery in the short term (1 year) for its treatment success, complication rate and cost, but surgery was better after 5 years, although the research is weak.[19]
A Health Technology Assessment found that sclerotherapy provided less benefit than surgery, but is likely to provide a small benefit in varicose veins without reflux.[20] Complications of sclerotherapy are rare but can include blood clots and ulceration. Anaphylactic reactions are "extraordinarily rare but can be life-threatening," and doctors should have resuscitation equipment ready.[21] There has been one reported case of stroke after ultrasound guided sclerotherapy when an unusually large dose of sclerosant foam was injected.
Endovenous Ablation (Saphenous Venous Ablation - Closure)
- Endovenous laser ablation (EVLA) is a relatively simple and quick technique which can be performed under a local anesthetic. Endovenous laser techniques employ an 810 nm-diode laser to heat the long or short saphenous vein (or major tributaries), inducing a combination of endothelial damage, focal coagulative necrosis, shrinkage of the vein and thrombotic occlusion.
- Radiofrequency ablation
The Australian Medical Services Advisory Committee (MSAC) in 2008 has determined that endovenous laser treatment for varicose veins "appears to be more effective in the short term, and at least as effective overall, as the comparative procedure of junction ligation and vein stripping for the treatment of varicose veins."[22] It also found in its assessment of available literature, that "occurrence rates of more severe complications such as DVT, nerve injury and paraesthesia, post-operative infections and haematomas, appears to be greater after ligation and stripping than after EVLT". Complications for endovenous laser treatment include minor skin burns (0.4%)[23] and temporary paraesthesia (2.1%).[23] The longest study of endovenous laser ablation is 39 months.
Two prospective randomized trials found speedier recovery and fewer complications after radiofrequency obliteration (AKA radiofrequency ablation) compared to open surgery.[24][25] Myers[26] wrote that open surgery for small saphenous vein reflux is obsolete. Myers said these veins should be treated with endovenous techniques, citing high recurrence rates after surgical management, and risk of nerve damage up to 15%. In comparison, radiofrequency ablation has been shown to control 80% of cases of small saphenous vein reflux at 4 years, said Myers. Complications for radiofrequency ablation include burns, paraesthesia, clinical phlebitis, and slightly higher rates of deep vein thrombosis (0.57%) and pulmonary embolism (0.17%).One 3-year study compared radiofrequency, with a recurrence rate of 33%, to open surgery, which had a recurrence rate of 23%.
References
- ↑ BMJ 2006;333:287-292 (5 August), Varicose veins and their management, Bruce Campbell (subscription)
- ↑ Curri SB et al. Changes of cutaneous microcirculation from elasto-compression in chronic venous insufficiency. In Davy A and Stemmer R, editors: Phlebology '89, Montrouge, France, 1989, John Libbey Eurotext.
- ↑ New Dietary Ingredients in Dietary Supplements, U.S. Food and Drug Administration, Center for Food Safety and Applied Nutrition Office of Nutritional Products, Labeling, and Dietary Supplements February 2001 (Updated September 10, 2001), http://www.cfsan.fda.gov/~dms/ds-ingrd.html
- ↑ Memorandum [1]
- ↑ Claude Franceschi, Cure CHIVA, 1988, Editions de L'Armançon, 21390 Precy-Sous-Thil France
- ↑ [2]
- ↑ Maeso and all, Comparison of clinical outcome of Stripping and CHIVA for Treatment of varicose veins in Lower Extremities, Ann Vasc Surg 2001; 15: 661-665
- ↑ Zamboni and all: Minimally Invasive Surgical management of primary Venous Ulcers vs Compression Treatment: a randomized Clinical Trial. Eur J Vasc Endovsc Surg 00, 1-6 (2003)
- ↑ Varicose Vein Stripping vs. Hemodynamic Correction (C.H.I.V.A.): a Long Term Randomised Trial S. Carandina and all; Eur J Vasc Endovasc Surg xx, 1e8 (2007) doi:10.1016/j.ejvs.2007.09.011, online http://www.sciencedirect.com
- ↑ van Rij AM et al. Incidence of Deep Venous Thrombosis after Varicose Vein Surgery, Br J Surg 2004 Dec; 91(12):1582-5
- ↑ Hammarsten J, Pedersen P, Cederlund CG, Campanello M. Department of Surgery and Radiology, Hospital of Varberg, Sweden Long saphenous vein saving surgery for varicose veins. A long-term follow-up. Eur J Vasc Surg. 1990 Aug;4(4):361-4.
- ↑ Goldman M, Sclerotherapy Treatment of varicose and telangiectatic leg vein, Hardcover Text, 2nd Ed, 1995
- ↑ "Veins & Lymphatics," L. K. Pak et al, in Lange's Current Surgical Diagnosis & Treatment, 11th ed., McGraw-Hill,
- ↑ Tisi PV, Beverley C, Rees A. Injection sclerotherapy for varicose veins. Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No.: CD001732.
- ↑ Paul Thibault, Sclerotherapy and Ultrasound-Guided Sclerotherapy, The Vein Book / editor, John J. Bergan, 2007.
- ↑ Padbury A, Benveniste G L, Foam echosclerotherapy of the small saphenous vein, Australian and New Zealand Journal of Phlebology Vol 8, Number 1 (December 2004)
- ↑ Kanter A, Thibault P. Saphenofemoral junction incompetence treated by ultrasound-guided sclerotherapy, Dermatol Surg. 1996. 22: 648-652.
- ↑ http://www.mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD001732/abstract.html
- ↑ Rigby KA, Palfreyman SJ, Beverley C, Michaels JA. Surgery versus sclerotherapy for the treatment of varicose veins. Cochrane Database of Systematic Reviews 2004, Issue 4. Art. No.: CD004980. [3]
- ↑ Michaels JA, Campbell WB, Brazier JE, MacIntyre JB, Palfreyman SJ, Ratcliffe J, et al. Randomized clinical trial, observational study and assessment of cost-effectiveness of the treatment of varicose veins (REACTIV trial). Health Technol Assess 2006;10(13). [4] This Health Technology Assessment monograph includes reviews of the epidemiology, assessment, and treatment of varicose veins, as well as a study on clinical and cost effectiveness of surgery and sclerotherapy
- ↑ William R. Finkelmeier, Sclerotherapy, Ch. 12, ACS Surgery: Principles & Practice, 2004, WebMD (hardcover book)
- ↑ Medical Services Advisory Committee, Endovenous laser therapy (ELT) for varicose veins. MSAC application 1113, Dept of Health and Ageing, Commonwealth of Australia, 2008. http://www.msac.gov.au/internet/msac/publishing.nsf/Content/2E0BACBB8704139ACA25745E001C2F21/$File/1113report.pdf
- ↑ 23.0 23.1 Elmore FA and Lackey D, Effectiveness of laser treatment in eliminating superficial venous reflux, Phlebology 2008 :23 :21-31
- ↑ Rautio, T, et al., Endovenous oblitration versus conventional stripping operation in the treatment of primary varicose veins, J Vasc Surg 2002:35:958-65
- ↑ Lurie F, et al., Prospective randomized study of endovenous radiofrequency oblitration (closure) versus ligation and vein stripping (EVOLVeS: two-year follow-up. Eur J Vasc Endovasc Surg 2005;29:67-73
- ↑ Kenneth Myers, An opinion —surgery for small saphenous reflux is obsolete!" Australian and New Zealand Journal of Phlebology, Vol 8, Number 1 (December 2004)
Additional Resources
- Haimovici's vascular surgery. Editor-in-chief: Ascher, Enrico 5th ed. 2004 ISBN 0632044586