Parry-Romberg syndrome: Difference between revisions
No edit summary |
|||
| Line 37: | Line 37: | ||
In addition, some individuals with Parry-Romberg syndrome may also experience associated neurological abnormalities. These may include severe headaches that last for extended periods of time and may be accompanied by visual abnormalities, nausea, and vomiting (migraines); facial pain (trigeminal neuralgia); and/or periods of uncontrolled electrical disturbances in the brain (seizures) that usually are characterized by rapid spasms of a muscle group that spread to adjacent muscles (contralateral Jacksonian epilepsy). The range and severity of associated symptoms and findings may vary from case to case. In most cases, Parry-Romberg syndrome appears to occur randomly for unknown reasons (sporadically).<ref>[http://www.peacehealth.org/kbase/nord/nord489.htm Parry Romberg Syndrome<!-- Bot generated title -->]</ref> | In addition, some individuals with Parry-Romberg syndrome may also experience associated neurological abnormalities. These may include severe headaches that last for extended periods of time and may be accompanied by visual abnormalities, nausea, and vomiting (migraines); facial pain (trigeminal neuralgia); and/or periods of uncontrolled electrical disturbances in the brain (seizures) that usually are characterized by rapid spasms of a muscle group that spread to adjacent muscles (contralateral Jacksonian epilepsy). The range and severity of associated symptoms and findings may vary from case to case. In most cases, Parry-Romberg syndrome appears to occur randomly for unknown reasons (sporadically).<ref>[http://www.peacehealth.org/kbase/nord/nord489.htm Parry Romberg Syndrome<!-- Bot generated title -->]</ref> | ||
==Diagnosis== | |||
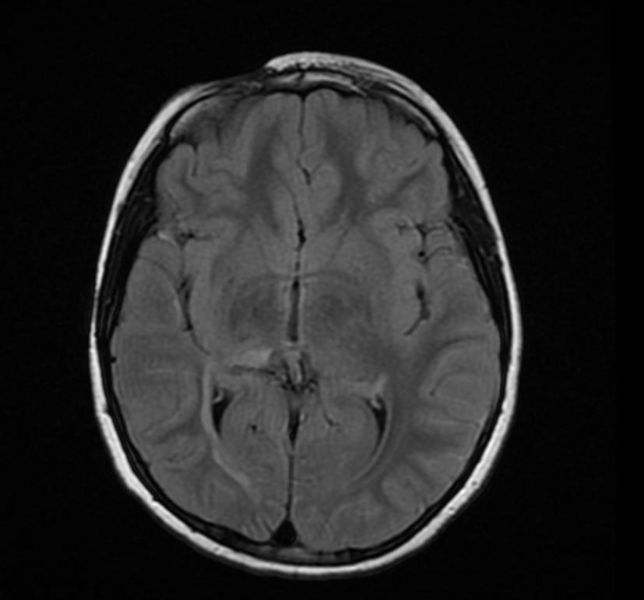
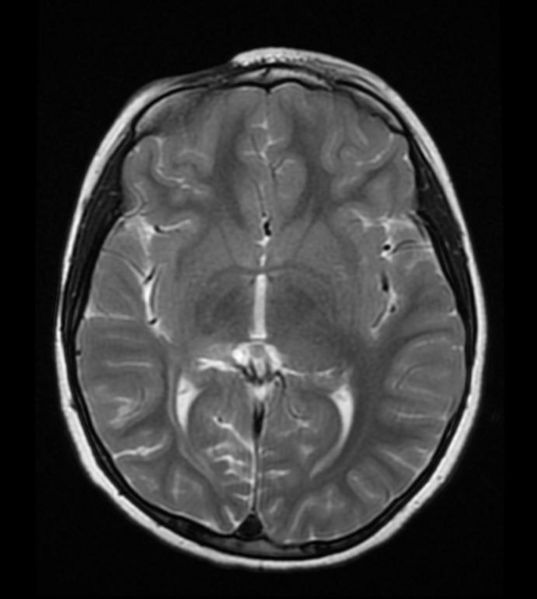
'''Marking thinning of the skin in the right frontal region is consistent with Parry Romberg syndrome''' | |||
<gallery> | |||
Image: | |||
Parry Romberg syndrome 1.jpg | |||
Image: | |||
Parry Romberg syndrome 2.jpg | |||
Image: | |||
Parry Romberg syndrome 3.jpg | |||
Image: | |||
</gallery> | |||
==Treatment== | ==Treatment== | ||
Revision as of 13:34, 6 August 2012
| Parry-Romberg syndrome | |
| ICD-10 | G51.8 |
|---|---|
| ICD-9 | 349.89 |
| OMIM | 141300 |
| DiseasesDB | 30151 |
| MeSH | D005150 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Parry-Romberg syndrome (sometimes called just Romberg syndrome) is a rare, incurable craniofacial disorder which is characterized by the slow atrophy of the subcutaneous (under the skin) muscle usually on half of the face (hemifacial atrophy). It has a higher prevalence in females and normally appears between the ages of 5 and 15. The condition also causes neurological symptoms, including seizures and severe facial pain.[1]
It is classified as a rare disease in the United States.
Eponym
The name comes from Parry (1825) and Henoch and Romberg (1846) who first described the disease.[2][3]
Disease Course
Parry-Romberg syndrome is a rare disorder characterized by slowly progressive degeneration (atrophy) of the soft tissues of half of the face (hemifacial atrophy). Some individuals may experience distinctive changes of the eyes and hair; and neurological abnormalities including episodes of uncontrolled electrical disturbances in the brain (seizures) and episodes of severe pain in tissues supplied by the fifth cranial nerve (trigeminal nerve) including the mouth, cheek, nose, and/or other facial tissues (trigeminal neuralgia). Symptoms and physical findings associated with Parry-Romberg syndrome usually become apparent during the first or early during the second decade of life. In rare cases, the disorder is apparent at birth. The majority of individuals with Parry-Romberg syndrome experience symptoms before the age of 20 years.
In individuals with the disorder, initial facial changes usually involve the tissues above the upper jaw (maxilla) or between the nose and the upper corner of the lip (nasolabial fold) and progress to involve the angle of the mouth, the areas around the eye, the brow, the ear, and/or the neck. Progressive tissue wasting can be on either side of the face. In some rare cases, the atrophy may be bilateral. Affected areas may demonstrate shrinkage and atrophy of tissues beneath the skin (subcutaneous tissue), the layer of fat under the skin (subcutaneous fat), and underlying cartilage, muscle, and bone.
In addition, the skin overlying affected areas may become darkly pigmented (hyperpigmentation) with, in some cases, areas of hyperpigmentation and patches of unpigmented skin (vitiligo). Many individuals also experience atrophy of half of the upper lip and tongue as well as abnormal exposure, delayed eruption, or wasting of the roots of certain teeth on the affected side. Symptoms of Parry-Romberg syndrome may begin at any age. Facial atrophy may cease abruptly, or progress slowly and then become stationary. If the atrophy becomes stationary, it may reactivate later in life. In other cases, the atrophy may progress indefinitely. In some cases, hair abnormalities may also appear on the affected side, including whitening (blanching) of the hair as well as abnormal bald patches on the scalp and loss of eyelashes and the middle (median) portion of the eyebrows (alopecia).
In addition, some individuals with Parry-Romberg syndrome may also experience associated neurological abnormalities. These may include severe headaches that last for extended periods of time and may be accompanied by visual abnormalities, nausea, and vomiting (migraines); facial pain (trigeminal neuralgia); and/or periods of uncontrolled electrical disturbances in the brain (seizures) that usually are characterized by rapid spasms of a muscle group that spread to adjacent muscles (contralateral Jacksonian epilepsy). The range and severity of associated symptoms and findings may vary from case to case. In most cases, Parry-Romberg syndrome appears to occur randomly for unknown reasons (sporadically).[4]
Diagnosis
Marking thinning of the skin in the right frontal region is consistent with Parry Romberg syndrome
Treatment
There is no cure and there are no treatments that can stop the progression of Parry-Romberg syndrome. Reconstructive or microvascular surgery may be needed to repair wasted tissue. The timing of surgical intervention is generally agreed to be the best following exhaustion of the disease course and completion of facial growth. Most surgeons will recommend a waiting period of one or two years before proceeding with reconstruction. Muscle or bone grafts may also be helpful. Other treatment is symptomatic and supportive.
Prognosis
The prognosis for individuals with Parry-Romberg syndrome varies. In some cases, the atrophy ends before the entire face is affected. In mild cases, the disorder usually causes no disability other than cosmetic effects.
References
- ↑ Template:NINDS
- ↑ Template:WhoNamedIt
- ↑ Cory RC, Clayman DA, Faillace WJ, McKee SW, Gama CH (1997). "Clinical and radiologic findings in progressive facial hemiatrophy (Parry-Romberg syndrome)". AJNR Am J Neuroradiol. 18 (4): 751–7. PMID 9127045.
- ↑ Parry Romberg Syndrome