Fetal hemoglobin
|
WikiDoc Resources for Fetal hemoglobin |
|
Articles |
|---|
|
Most recent articles on Fetal hemoglobin Most cited articles on Fetal hemoglobin |
|
Media |
|
Powerpoint slides on Fetal hemoglobin |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Fetal hemoglobin at Clinical Trials.gov Trial results on Fetal hemoglobin Clinical Trials on Fetal hemoglobin at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Fetal hemoglobin NICE Guidance on Fetal hemoglobin
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Fetal hemoglobin Discussion groups on Fetal hemoglobin Patient Handouts on Fetal hemoglobin Directions to Hospitals Treating Fetal hemoglobin Risk calculators and risk factors for Fetal hemoglobin
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Fetal hemoglobin |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Fetal hemoglobin (also hemoglobin F or HbF) is the main oxygen transport protein in the fetus during the last seven months of development in the uterus. Functionally, fetal hemoglobin differs most from adult hemoglobin in that it is able to bind oxygen with greater affinity than the adult form, giving the developing fetus better access to oxygen from the mother's bloodstream.
In newborns, fetal hemoglobin is nearly completely replaced by adult hemoglobin by approximately the twelfth week of postnatal life. In adults, fetal hemoglobin production can be reactivated pharmacologically, which is useful in the treatment of such diseases as sickle-cell disease.
Overview
Oxygenated blood is delivered to the fetus via the umbilical vein from the placenta, which is anchored to the wall of the mother's uterus. As blood courses through the mother, oxygen is delivered to capillary beds for gas exchange, and by the time blood reaches the capillaries of the placenta, its oxygen saturation has decreased considerably. In order to recover enough oxygen to sustain itself, the fetus must be able to bind oxygen with a greater affinity than the mother.
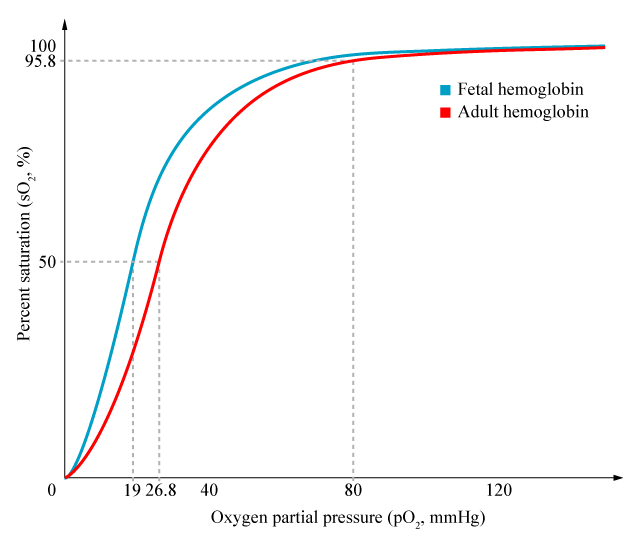
Fetal hemoglobin's affinity for oxygen is substantially greater than that of adult hemoglobin. Notably, the P50 value for fetal hemoglobin (i.e., the partial pressure of oxygen at which the protein is 50% saturated; lower values indicate greater affinity) is roughly 19 mmHg, whereas adult hemoglobin has a value of approximately 26.8 mmHg. As a result, the so-called "oxygen saturation curve", which plots percent saturation vs. pO2, is left-shifted for fetal hemoglobin in comparison to the same curve in adult hemoglobin.
This greater affinity for oxygen is explained by fetal hemoglobin's interaction with 2,3-bisphosphoglycerate (2,3-BPG). In adult red blood cells, this substance decreases the affinity of hemoglobin for oxygen. It is also present in fetal red blood cells, but does not interact with fetal hemoglobin, leaving its affinity for oxygen unchanged. Adult hemoglobin alone actually has a higher affinity for oxygen than its fetal equivalent, but the levels of 2,3-BPG reduce it.
For mothers to deliver oxygen to a fetus, it is necessary for the fetal hemoglobin to extract oxygen from the maternal oxygenated hemoglobin across the placenta. This requires the fetal hemoglobin to have a higher oxygen affinity than that of the maternal carrier. This is achieved by a fetal hemoglobin subunit γ (gamma), instead of the b (beta) subunit. The γ subunit has less positive charges than the adult hemoglobin b subunit. This means that 2,3-bisphosphoglycerate (2,3-BPG) is less electrostaticly bound to fetal hemoglobin as compared to adult hemoglobin. This means that 2,3-BPG is less effective in lowering the oxygen affinity of the fetal hemoglobin. This lowered affinity of HbF for 2,3-BPG allows for adult hemoglobin (the maternal hemoglobin of the mother) to readily transfer its oxygen to the fetal hemoglobin.
Distribution
After the first 10 to 12 weeks of development, the fetus' primary form of hemoglobin switches from embryonic hemoglobin to fetal hemoglobin. At birth, fetal hemoglobin comprises 50-95% of the child's hemoglobin. These levels decline after six months as adult hemoglobin synthesis is activated while fetal hemoglobin synthesis is deactivated. Soon after, adult hemoglobin (hemoglobin A in particular) takes over as the predominant form of hemoglobin in normal children.
Structure and genetics
Most types of normal hemoglobin, including hemoglobin A, hemoglobin A2, hemoglobin S, and hemoglobin F, are tetramers composed of four protein subunits and four heme prosthetic groups. Whereas adult hemoglobin is composed of two alpha and two beta subunits, fetal hemoglobin is composed of two alpha and two gamma subunits, commonly denoted as α2γ2. Because of its presence in fetal hemoglobin, the gamma subunit is commonly called the "fetal" hemoglobin subunit.
In humans, each chromosome 11 contains two identical copies of the gene that encodes the gamma subunit. The gene that codes for the alpha subunit is located on chromosome 16 and is also present in duplicate.
Treatment of sickle cell anemia
When fetal hemoglobin production is switched off after birth, normal children begin producing adult hemoglobin (HbA.) But children with sickle-cell disease instead begin producing a defective form of hemoglobin called hemoglobin S. This variety of hemoglobin aggregates, forming filaments and so causes red blood cells to change their shape from round to sickle-shaped, which have a greater tendency to stack on top of one another and crowd blood vessels. These invariably lead to so-called painful vaso-occlusive episodes, which are a hallmark of the disease.
If fetal hemoglobin remains the predominant form of hemoglobin after birth, however, the number of painful episodes decreases in patients with sickle cell anemia. Hydroxyurea, used also as an anti-cancer drug, is a viable treatment for sickle cell anemia, as it promotes the production of fetal hemoglobin while inhibiting sickling due to hemoglobin S polymerization.
Combination therapy with hydroxyurea and recombinant erythropoietin—rather than treatment with hydroxyurea alone—has been shown to further elevate hemoglobin F levels and to promote the development of HbF-containing F-cells [2].

References
- Hemoglobin synthesis
- Hemoglobin structure and function
- Hemoglobin F fact sheet
- Fetal hemoglobin [doc]
- Hydroxyurea in sickle-cell disease
- Management of sickle-cell disease
- Effect of hydroxyurea on the frequency of painful crises in sickle cell anemia (original 1995 study)